
REPORT 633
Holes in the safety net:
A review of TPD
insurance claims
October 2019
About this report
This report summarises the findings and recommendations from ASIC’s
thematic review of total and permanent disability (TPD) insurance in
Australia.
In particular, it reviews outcomes for consumers, claims handling practices,
the role of data in managing the risk of consumer harm, and our findings on
insurers with higher than predicted rates of declined claims.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 2
About ASIC regulatory documents
In administering legislation ASIC issues the following types of regulatory
documents.
Consultation papers: seek feedback from stakeholders on matters ASIC
is considering, such as proposed relief or proposed regulatory guidance.
Regulatory guides: give guidance to regulated entities by:
explaining when and how ASIC will exercise specific powers under
legislation (primarily the Corporations Act)
explaining how ASIC interprets the law
describing the principles underlying ASIC’s approach
giving practical guidance (e.g. describing the steps of a process such
as applying for a licence or giving practical examples of how
regulated entities may decide to meet their obligations).
Information sheets: provide concise guidance on a specific process or
compliance issue or an overview of detailed guidance.
Reports: describe ASIC compliance or relief activity or the results of a
research project.
Disclaimer
This report does not constitute legal advice. We encourage you to seek your
own professional advice to find out how the Corporations Act and other
applicable laws apply to you, as it is your responsibility to determine your
obligations.
Examples in this report are purely for illustration; they are not exhaustive and
are not intended to impose or imply particular rules or requirements.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 3
Contents
Executive summary ................................................................................. 4
What we did in this review ................................................................. 6
Summary of findings .......................................................................... 7
ASIC’s expectations and action ....................................................... 16
A TPD insurance in Australia ........................................................... 20
What is TPD insurance? .................................................................. 20
Snapshot of the TPD insurance market ........................................... 22
Regulatory environment and gaps ................................................... 24
B Poor consumer outcomes from the activities of daily living
(ADL) test ........................................................................................ 31
The significance of eligibility criteria in TPD cover .......................... 31
Detailed data findings on ADL claims .............................................. 36
Consumer harms from low-value ADL cover ................................... 43
Other TPD product design issues .................................................... 44
Further action ................................................................................... 47
C Claims handling and withdrawn claims ...................................... 50
Withdrawn claim rates ..................................................................... 50
Why claims are withdrawn ............................................................... 51
The claim lodgement process .......................................................... 53
Frictions in the claim assessment process ...................................... 57
Further action ................................................................................... 69
D Poor-quality data and consumer harm ........................................ 72
Good data is essential for managing the risk of consumer harm .... 73
Insurers had poor data ..................................................................... 75
Further action ................................................................................... 84
E Declined claims: Findings and outliers ....................................... 86
Industry-wide findings on key factors .............................................. 88
Findings on insurer-declined claim rates ......................................... 94
Further action ................................................................................... 96
Appendix 1: Methodology .................................................................... 97
Our approach ................................................................................... 97
Stakeholder consultation ................................................................. 98
Data collection ................................................................................. 98
Statistical analysis of declined claim data ....................................... 99
Qualitative review .......................................................................... 101
Consumer research ....................................................................... 102
Appendix 2: Accessible versions of figures ..................................... 103
Key terms ............................................................................................. 108
Related information ............................................................................. 113

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 4
Executive summary
1 Total and permanent disability (TPD) insurance is a type of life insurance that
pays a lump sum if the consumer becomes totally and permanently disabled
under the terms of the insurance policy. Its purpose is to replace future
retirement savings lost due to disablement. A TPD benefit can also help with
the costs of rehabilitation, debt repayments and future costs of living.
2 TPD insurance is widely held—over 13.4 million consumers have TPD cover
and almost 90% are insured through their superannuation fund. It plays a
crucial role as a safety net in supporting the financial security of Australians.
During the 12 months to 31 December 2018, TPD insurance premiums totalled
$3.548 billion and consumers made more than 26,000 claims.
3 This report builds on ASIC’s previous review of life insurance in Report 498
Life insurance claims: An industry review (REP 498). In REP 498 we
identified several concerns about TPD insurance including above-average
declined claim rates, high rates of withdrawn claims and poor claims-
processing times. We undertook to review TPD claims processes.
4 In REP 498 we found that only 65% of notified TPD claims were accepted
by insurers, with the balance of claims either declined by the insurer or
withdrawn by the consumer. We were concerned that the acceptance rate
indicates problems both with the design of TPD policies (with cover being
too restrictive under some policies) and with claims handling procedures.
5 This report identifies four important industry-wide issues that insurers and
superannuation trustees must fix: see Table 1. They are not the only
problems associated with TPD insurance. Other issues include the role of
rehabilitation providers and the difficulty of comparing TPD definitions
particularly in the context of insurance in superannuation (both of which are
touched on in this report).
6 However, we consider that these four issues in particular create poor consumer
outcomes and are connected to our undertaking in REP 498
to review TPD
claims processes. We expect insurers and superannuation trustees to address
the problems we have identified. ASIC will also take action to address these
issues. We have set out ASIC’s expectations and actions in
Table 3.
7 ASIC will take further action, including enforcement action where
appropriate, against insurers and superannuation trustees who fail to properly
address our concerns. We will also consider using our product intervention
powers to prevent harm to consumers.
REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 5
Table 1: Four key industry-wide issues in the TPD market
Issue
What we found
Poor consumer
outcomes from the
‘activities of daily
living’ test
Many insurers selling policies with restrictive cover based on the ‘activities of daily
living’ (ADL) disability test. These policies make some consumers eligible only for a
narrow form of TPD cover due to their work status (e.g. non-permanent, casual or
part-time employees). This narrow cover pays out only if consumers cannot perform
several ‘activities of daily living’ such as feeding, dressing or washing themselves.
We consider that these policies are not designed for, and do not operate to meet the
needs of, the broad range of consumers who are funnelled into this type of cover.
These policies do not appear to provide cover for all consumers who are unable to
work again—they provide cover only to consumers who are so severely disabled that
they cannot care for themselves.
Frictions in claims
handling leading to
withdrawn claims
Approximately 12.5% of TPD claims during the period of our review were withdrawn.
We consider that this high withdrawal rate is, at least, partially due to insurers
subjecting consumers who are vulnerable (due to life-altering illness or injury) to a
claims process that is often unnecessarily challenging and onerous.
Consumer harm
arising from poor data
Insurers had significant deficiencies in their ability to record and search for relevant
claims data. Without accurate and timely data, insurers cannot identify problems in
their products or processes, or determine the changes needed to address problems
and improve consumer outcomes. Insurers will need better data to help them meet
the design and distribution obligations, which will take effect from April 2021.
Insurers with higher
than predicted
declined claim rates
Claims with certain characteristics such as the type of underlying condition or
occupation of the consumer had higher than predicted declined rates. Our analysis
also found that three insurers had higher than predicted declined claim rates: see
paragraphs 41–46.
Key role of superannuation trustees
Insurance is an important feature of the superannuation system and most
superannuation funds offer their members life insurance cover in addition to
retirement benefits. Trustees of MySuper products are generally required by
law to offer members death cover and TPD cover on an opt-out basis.
MySuper products are designed for a broad range of consumers including
those who are highly disengaged.
While our review was focused on insurers, superannuation trustees play a
crucial role in the delivery of life insurance to superannuation fund members,
as they must approve the design of the policy, choose an insurer and agree
commercial terms, and act as the policy holder for group insurance.
We expect superannuation trustees to act in their members’ best interests by
providing access to affordable insurance products that are suitably designed
for their members. This includes safeguarding their members’
superannuation balances from inappropriate erosion.
We also expect superannuation trustees to play a robust role alongside
insurers in ensuring a good claims experience for consumers. This role
encompasses not just advocating for claims with reasonable prospects of
success, but also actively engaging with the consumer’s claim journey to
make sure processes are simple, timely and transparent. This includes the
management of any insurance-related complaints.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 6
What we did in this review
8 Figure 1 summarises the different elements of our review. For further details
of our methodology, see Appendix 1 of this report. The review covered the
period from 1 January 2016 to 31 December 2017.
Figure 1: What we did
Note: See Appendix 1 of this report for an accessible version of the information contained in Figure 1. For details of the
methodology and limitations of our consumer research, see paragraphs 358–365 in Appendix 1.
9 The following insurers were included in our review:
(a) AIA Australia Limited (AIA);
(b) AMP Life Limited (AMP) and The National Mutual Life Association of
Australasia Limited—part of the AMP Group of companies;
(c) Asteron Life & Superannuation Limited (Asteron)—previously known
as Suncorp Life & Superannuation Limited (Suncorp);
(d) MetLife Insurance Limited (MetLife);
(e) MLC Limited (MLC);
(f) TAL Life Limited (TAL); and
(g) Westpac Life Insurance Services Limited (Westpac).
Note: On 28 February 2019, the Suncorp Group announced the completion of the sale of
its life insurance business to Japanese insurer Dai-ichi Life Holdings, which also owns
TAL. See Suncorp Group, Completion of Australian life business sale (PDF 22 KB),
ASX announcement, 28 February 2019.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 7
Summary of findings
Poor consumer outcomes from the ‘activities of daily
living’ test
Finding 1: Claims assessed under the ‘activities of daily living’ test
generally result in poor outcomes, with three out of five such claims
being declined
10 TPD cover is designed for people who are totally and permanently disabled.
However, the meaning of total and permanent disablement varies between
the different TPD products distributed by insurers.
11 Most consumers who make a claim are assessed under the so-called ‘any
occupation’ or ‘own occupation’ tests. Under these tests, consumers making
a claim are considered totally and permanently disabled if they are unable to
work in ‘any occupation’ or their ‘own occupation’ again. However, some
consumers may be paying premiums for TPD cover under a more restrictive
policy definition—the ‘activities of daily living’ (ADL) test.
12 We found that the declined rate for TPD claims assessed under the ADL test
was very high: 60%, or three in five claims, were declined. This was five
times higher than the average declined rate for all other TPD claims (12%).
13 Although ADL claims represented a relatively small percentage of all TPD
claims in our review (4%), based on the 26,150 TPD claims made across all
life insurers in 2018 this translates to almost three claims per day being
assessed under this restrictive definition.
14 The declined rates for TPD claims assessed under the ADL test were
concerningly high for some group superannuation policies. The 10 highest
ADL declined rates at group policy level ranged from 45% to 87%: see
paragraphs 114–118 and Table 6 in this report.
15 There is the risk of harm when consumers pay for ADL cover in that:
(a) they are paying premiums for insurance cover that they are unlikely to
be able to successfully claim on and therefore cannot rely on if they are
disabled;
(b) because most consumers have automatic insurance through their
superannuation, they generally pay the same premium regardless of
whether, in the event of a claim, they are eligible for ADL-only cover or
more general TPD cover; and
(c) economically vulnerable consumers are especially disadvantaged as the
eligibility criteria often mean that casual, contract or seasonal
employees are funnelled into ADL-only cover.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 8
Finding 2: Eligibility criteria in group insurance cover mean that some
consumers are automatically funnelled into low-value ADL cover
which may not be worth paying for
16 Consumers who do not meet certain eligibility criteria in group cover are
often assessed under the restrictive ADL definition.
17 The eligibility criteria in group TPD cover mean that the following
consumers are typically funnelled into the narrower ADL definition:
(a) casual, seasonal or part-time employees who work less than a specified
number of hours (e.g. 15 hours per week);
(b) people who have been unemployed or on leave without pay for a stated
period before the TPD event (often six months, but for some policies
12 months); and/or
(c) people in specified occupations that the insurer considers are high risk.
18 ASIC is concerned that these types of eligibility criteria unfairly affect more
vulnerable consumers, including unskilled workers, people with parental or
other caring responsibilities, and workers in certain industries such as retail
and hospitality. With the changing nature of the workforce and the growth of
the ‘gig economy’, these types of eligibility criteria will capture an
increasingly broad range of consumers.
19 The risks to consumers who hold these types of group policies are
heightened by the low level of engagement that most consumers have with
insurance in superannuation. As the Productivity Commission noted in its
recent report on superannuation, 24% of superannuation members surveyed
did not know whether there was insurance in their fund, and a further 16%
knew they paid for insurance but did not know what they were covered for.
These consumers are likely to be unaware that their insurance may provide
less cover if their employment changes. Consumers are relying on unusable
cover when they could potentially purchase more suitable cover.
Note: See Productivity Commission, Superannuation: Assessing efficiency and
competitiveness, inquiry report no. 91, December 2018 (Productivity Commission
report), pp. 384–5.
20 The fact that 4% of TPD claims are assessed under the ADL test means that
at least 4% of the 12 million consumers (480,000) who hold TPD in
superannuation are potentially at risk of unusable or inadequate cover.
21 The complexity of and lack of comparability across insurance offerings also
make it difficult for consumers to compare policies and understand the cover
they have. Our findings endorse the need for greater standardisation of
terms, especially within superannuation.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 9
Finding 3: The ADL test is unsuitable for a range of common illnesses
and injuries, including mental illness and musculoskeletal disorders
22 The ADL test is suited only to disability caused by the most catastrophic
type of injury or illness. When we compared declined claim rates for certain
conditions under the narrower ADL definition with rates under the broader
general TPD definition, we found that:
(a) mental health claims were approximately five times more likely to be
declined (77% for ADL compared to 15% for the general definition);
and
(b) musculoskeletal claims were more than five times more likely to be
declined (71% for ADL compared to 13% for the general definition).
23 The concerningly high declined claim rate for consumers with mental illness
or musculoskeletal disorders assessed under ADL indicates that this type of
restrictive TPD cover is unsuitable for many consumers to whom it is being
provided or sold. These medical conditions may be a common cause of
disability for certain classes of employees (e.g. manual workers who may be
more susceptible to musculoskeletal injuries yet whose employment
arrangements mean they are defaulted into ADL-only TPD cover).
24 We are aware that one insurer has removed ADL cover from some TPD
policies offered within superannuation. This is a step in the right direction.
25 Superannuation trustees have a key role to play: they have a legal obligation
to offer insurance benefits for fund members (consumers) that are both
appropriate and affordable. Considering the needs of different consumer
cohorts may require careful balancing by trustees, and some degree of cross-
subsidisation is inherent in group insurance as it involves pooling risk.
However, we expect insurers and trustees to stop providing ‘junk’ insurance
products to consumers. Trustees and insurers must ensure that the products
they design and/or distribute are suitable for the consumers to whom they are
provided or sold.
Frictions in claims handling leading to withdrawn claims
Finding 4: Insurers do not have sufficient understanding of the
reasons for withdrawn claims
26 Withdrawn claims are an important indicator of potential consumer harm.
Consumers suffer harm if claims handling processes contain frictions which
result in consumers withdrawing potentially valid claims. The way in which
a claim is withdrawn, and the timing of the withdrawal, may indicate where
there are frictions in the claims handling process. Withdrawn claim rates
may also mask real declined claim rates.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 10
27 Insurers were generally poor at capturing reasons for withdrawn claims. We
found that for over 50% of withdrawn claims, the reason given by the insurer
was lack of response by the consumer to a request for information. This lack
of response could be driven by factors which, if identified, could be properly
addressed.
28 The second most common reason recorded was the consumer withdrawing
for reasons other than eligibility or return to work (31%). Insurers did not
record the actual reason for these active withdrawals.
29 While we acknowledge that it is not always possible for an insurer (or
superannuation trustee) to know the reasons for withdrawn claims, we expect
insurers to improve their understanding of these reasons. When a consumer
begins a claim via a trustee for insurance held in superannuation, a
superannuation trustee has obligations to pursue insurance claims for
members. Therefore, we expect trustees to improve their own understanding
of the reasons for withdrawn claims.
Finding 5: Insurers’ claims handling practices create frictions that
contribute to consumers withdrawing claims
30 Our consumer research found that consumers had limited time, ability, focus
and/or funds to manage a TPD claim because they:
(a) were typically impaired or in pain due to a life-altering illness or injury;
(b) were often dealing with numerous other issues connected with their
illness or injury—medical appointments, overdue bills and debt
collectors, or separate legal processes (e.g. WorkCover, claims against
their employer, and public liability insurance claims); and
(c) had limited or no income to live on.
31 Information obtained from insurers together with our consumer research
identified numerous frictions for consumers in the claim assessment process,
including the following:
(a) Poor insurer communication practices—The way in which insurers’
claims staff communicated with consumers had a significant effect on
consumer experience; empathetic and proactive communication is key
to good claims-handling practice.
(b) Multiple requests for further medical assessments—These requests
often seemed unreasonable or unnecessary and were a concern
reiterated throughout our consumer research.
(c) Potentially threatening behaviour, including surveillance of claimants
and questionable allegations of fraud—Seven out of 20 consumers we
interviewed in our consumer research were subject to physical
surveillance and reported experiencing additional stress. This was not
drawn from a representative sample of claims (details of the

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 11
methodology used are contained in Appendix 1 of this report). Yet our
data analysis showed that where physical surveillance was used more
broadly, the insurer ultimately admitted the claim in over 60% of cases.
(d) Excessive delay—Delay in receiving a claims decision was an issue for
many of the consumers who participated in our consumer research.
‘Unexpected circumstances’ allow insurers to extend the promised
timeframe in the Life Insurance Code of Practice (Life Code) for a TPD
claims decision from six months to 12 months.
(e) ‘Fishing’ for non-disclosure—The Royal Commission into Misconduct
in the Banking, Superannuation and Financial Services Industry (Royal
Commission) raised concerns about insurers seeking to avoid claims by
relying on a legal technicality rather than supporting the consumer
through the claims process.
(f) Ongoing costs of the claims process—The claim assessment process,
including being asked to attend multiple medical appointments, can be
‘time consuming, costly and painful’.
(g) Changes to claims staff—Several consumers emphasised the difficulties
they encountered when the staff managing their claim changed. We
found that several insurers in our review had a claims staff turnover rate
near or above 25% for one of the two years of our review.
32 Our consumer research and data analysis showed that these practices and the
frictions they created contributed to the withdrawal of 4,365 claims during
the period of our review—approximately one out of eight claims reported.
Consumer harm arising from poor data
Finding 6: Insurers did not have adequate data to effectively manage
the risk of consumer harm
33 Good data is key for the effective and proactive management of the risk of
consumer harm. To effectively manage consumer harm, insurers need data
that is timely, accurate, adequate and complete and that uses consistent
definitions. Without timely and insightful data, insurers cannot proactively
identify and address, in a targeted manner:
(a) the value of products to consumers and whether the products are
meeting consumer needs;
(b) key friction points in the TPD claims handling process;
(c) claims handling staff whose conduct may give rise to a higher
likelihood of consumer harm;
(d) claims handling practices leading to consumer harm; and
(e) harm caused to consumers at either a granular or consolidated level.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 12
34 Our review found that, to varying degrees, all seven insurers failed to meet
our criteria for ‘good data’ during 2016 and 2017, for the reasons set out in
Table 2.
Table 2: Findings on insurers’ data resources
Insurers’ responses to our data
requests were slow
No insurer could provide a complete response to our data request by the
due date (a reasonable time in which to respond). Full responses from
some insurers were still outstanding five months after we requested
claims data under statutory notice.
Crucial data was not readily
available in searchable formats
All insurers needed to conduct manual reviews to extract relevant data,
including reviewing paper files.
Some requested data was not
available at all
Some insurers could not tell us how many claims they had assessed
under an ADL definition. Most insurers could not provide accurate data
on something as fundamental as whether a consumer had withdrawn a
claim because they had returned to work.
All insurers’ responses contained
errors
Some insurers resubmitted errors to ASIC after we had informed them of
the errors in our initial feedback.
There were no standard
definitions for key data
This lack of consistency was particularly problematic for claims
notification and lodgement. For example, insurers used a range of
practices to record when a claim ‘begins’. This issue has been improved
through work undertaken with the Australian Prudential Regulation
Authority (APRA)—the ASIC-APRA life claims data collection work.
Insurers did not have access to
comprehensive data about
insurance in superannuation
claims
For some insurance in superannuation claims, insurers became involved
in a claim after the superannuation trustee passed details of a claim and
the consumer on to them. Insurers usually did not have information about
what occurred before the claim was passed on to them—including the
amount of time since the consumer first notified the trustee of the claim,
which is fundamental to understanding how a consumer has been
pursuing a claim.
35 No insurer had a holistic, up-to-date picture of the potential consumer harm
arising from TPD claims handling and outcomes. They could only get this
information from reactive, post-event quality assurance reviews, audits or
analysis—by which time conduct risk and consumer harm had already
crystallised.
Finding 7: Despite some improvements, insurers must invest more
time, resources and funds to strengthen data resources to effectively
reduce the risk of consumer harm
36 Insurers are already improving their data capability largely to meet the
requirements of APRA and ASIC’s data collection initiatives. However,
insurers must do more to address the issues we have identified. We expect
boards and owners of all insurers to ensure there is sufficient investment in
the business to appropriately manage the risk posed by inadequate data
resources. This will require additional investment and the active engagement

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 13
of boards and senior management. We also expect superannuation trustees to
ensure that they receive adequate data from insurers to manage the risk of
harm to their members (consumers).
37 Recent and anticipated changes to life insurer ownership create an
opportunity for these issues to be resolved. We are aware of at least one new
owner investing in data and systems since buying a life company from an
Australian bank, and we encourage other owners to do the same.
Insurers with higher than predicted declined claim rates
Finding 8: Different factors, such as the TPD definition, the consumer’s
age and the underlying TPD condition, have significantly different
likelihoods of a claim being declined—unfairly affecting some consumers
38 We analysed the data we collected and used statistical modelling to identify
factors that were statistically significant in relation to the likelihood of a
claim being declined. Based on the results, ASIC is concerned that
consumers with these characteristics may be receiving unfair treatment.
39 In addition to the significant variations between claims assessed under different
TPD definitions, we made the following findings across the seven insurers:
(a) There was a significant difference between the declined rates for
disease-related claims and for claims for other conditions. Mental
illness–related claims had the highest declined rate at 16.9% closely
followed by injury or fracture conditions at 16.1%. TPD claims for
disease-related conditions had a lower declined rate of 9.7%. While
there may be legitimate reasons for this difference, we expect insurers
to ensure that their claims handling procedures are not operating
unfairly for consumers with mental health, injury or fracture conditions.
(b) The rate of declined claims decreased as the age of the consumer
increased. This could be expected, as it is more difficult for an insurer
to determine that a younger person will never be able to work again,
than to determine the same for an older person. However, two
insurers—MLC and TAL—had a noticeably lower rate of declined
claims for younger consumers. We will be working with the other
insurers to understand this difference.
(c) The age of the policy at the claim event date (the number of days since
the policy began, to the date of the TPD claim) is significant. Generally,
the longer a policy is in force, the lower the declined claim rate.
(d) The length of any delay in claim reporting is significant. Claims that
were reported more than 1,000 days after the claim event were declined
at a higher rate—around 17.4% compared to 12.4% for other claims.
We will be working with insurers, particularly where the insurer on risk

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 14
for a claim is no longer the current insurer for the relevant
superannuation fund, to understand this difference.
(e) There was only a slight difference between the declined rates for claims
on group policies (13.6%) and for retail policies (14.5%).
40 We expect all insurers to review their claims handling practices in light of
this analysis to ensure they are not treating groups of consumers unfairly.
Finding 9: TPD declined claim rates varied significantly between
individual insurers
41 As Figure 2 shows, TPD declined claim rates varied significantly among
insurers, from TAL with a declined rate of 9% to Westpac and Asteron with
declined rates of 28% and 29% respectively.
Figure 2: Declined claim rates for TPD cover, by insurer (2016–17)
Source: ASIC data collection
Note 1: Some of the difference in declined claim rates between insurers can be explained by the
relative mix of each insurer’s policy portfolio and distribution channel including:
• distribution channels: the declined claim rates vary for group (13.6%), retail (14.5%) and
direct (22.6%) (see Table 20 in this report); and
• policies open for sale and closed to sale (i.e. legacy products).
Note 2: See Table 24 in Appendix 2 of this report for the underlying data (accessible version).
42 We collected data about more than 35,000 TPD claims to improve our
understanding of these declined rates. The granularity of our data collection
allowed us to conduct industry-wide analysis that, to our knowledge, has not
been undertaken in the Australian life insurance market before. By assessing
the individual characteristics of each claim, we were able to predict the
declined claim rate for each insurer based on the features of its claims and
then identify factors that contributed to any variance from the predicted rate.
29%
28%
18%
16%
15%
12%
9%
71%
72%
82%
84%
85%
88%
91%
Asteron
Westpac
MLC
AIA
AMP
MetLife
TAL
Declined claims Accepted claims

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 15
43 The data we collected allowed us to analyse the following 10 factors:
(a) the type of definition the claims were assessed under (i.e. ADL, ‘any
occupation’ and ‘own occupation’);
(b) the age of the consumer making the claim;
(c) the primary medical condition giving rise to the claim;
(d) whether the claim was formally underwritten and tailored in some way
to the consumer;
(e) the type of policy the claim was made on (i.e. a group policy, a retail
policy or a direct policy);
(f) the gender of the consumer making the claim;
(g) the amount the consumer was insured for under the policy;
(h) the delay between the date the claim was made and the date that the
consumer became aware of the primary condition;
(i) the length of time the policy had been in effect; and
(j) whether the consumer had a white-collar or blue-collar occupation.
44 The methodology, analysis and statistical results were reviewed and
confirmed as appropriate by Finity Consulting, an actuarial consultancy firm.
The limitations of our methodology, analysis and conclusions are set out in
Appendix 1 of this report.
Finding 10: AMP, Asteron and Westpac had higher than predicted
declined rates for claims with certain characteristics
45 As illustrated by Figure 3, our analysis showed that for claims where a
decision had been made, AMP, Asteron and Westpac had declined claim
rates higher than our analysis predicted. The declined claim rate for Asteron
was almost double what our analysis predicted.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 16
Figure 3: Actual declined rates compared to ASIC-predicted declined rates for claims that
went to a final decision, by insurer (2016–17)
Source: ASIC data collection
Note: See Table 25 in Appendix 2 of this report for the underlying data shown in this figure (accessible version).
46 We may undertake targeted surveillance work to examine the reasons for the
substantially higher declined claim rates and consider appropriate regulatory
action if required.
ASIC’s expectations and action
47 Table 3 summarises our expectations of insurers and superannuation trustees
based on the findings of our review, along with the action we will be taking.
0%
5%
10%
15%
20%
25%
30%
35%
Asteron Westpac
AMP
AIA Metlife TAL
MLC
Declined claim rate
Actual Predicted

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 17
Table 3: ASIC’s expectations
Problem
What we expect of insurers and superannuation trustees
What ASIC will do
Poor consumer
outcomes from
the ADL test and
other restrictive
definitions
(see Section B)
We expect all insurers and superannuation trustees (not just those
included in this review) to:
review all TPD policies that include ADL or other restrictive definitions
(e.g. ‘loss of limbs’) to:
− consider removing definitions in group policies that are so restrictive
as to make the policy unlikely to benefit the consumers to whom the
policy is sold or provided, or appropriately redesign the product; and
− develop measures to assess the value of the product offered or
provided to consumers;
improve data collection on outcomes for different types of TPD cover,
including ADL or other restrictive definitions; and
improve communications with consumers about the type of TPD cover
they will be eligible for under various circumstances.
We expect trustees to consider our findings when negotiating future
group insurance arrangements with insurers. Trustees must be confident
that the definition used for TPD in group insurance arrangements is
consistent with their duty to act in the best interests of fund members
(consumers).
We expect insurers to have addressed our expectations by 31 March
2020.
ASIC will conduct further work during 2020 and 2021 to assess the
suitability of ADL and other restrictive definitions in TPD policies and the
benefit to consumers of the policies that contain these definitions. This
work will be informed by additional data about restrictive definitions that we
expect industry to collect, particularly about claim outcomes, underlying
claim conditions and loss ratios for products where the ADL definition is
used.
ASIC will ask certain insurers selected at our discretion to report to us on
the changes made to their retail and direct product offerings, using our
compulsory notice powers under financial services laws if necessary. We
will consider reporting publicly on the appropriateness of the changes made
by insurers during 2020 and 2021.
We will also consider information that insurers report to us about their
analysis of each policy containing an ADL definition, the changes made to
the TPD policy (removal or redesign of the definition, including eligibility)
and the specific measures in place to assess consumer value. We will
consider using our product intervention powers to regulate the sale of
policies where we are satisfied that there is a reasonable likelihood of
consumer harm or detriment.
We will conduct targeted surveillance of insurers, particularly for products
that had the highest rate of declined claims for various definition types. We
will take enforcement action if appropriate.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 18
Problem
What we expect of insurers and superannuation trustees
What ASIC will do
Frictions in
claims handling
leading to
withdrawn
claims
(see Section C)
We expect all insurers and superannuation trustees to work constructively
towards a consistent set of binding standards for life insurance that
covers both insurers and trustees and contains robust standards for all
third-party providers. The next iteration of the Life Code and the
Insurance in Superannuation Code should incorporate additional or
enhanced obligations including for proactive communication with
consumers during their claim, appropriate use of desktop surveillance,
and documented guidelines on training and competency requirements for
claims handling staff.
We expect insurers and, where relevant, trustees to take immediate steps
to implement our recommended changes to claims handling practices,
reinsurer arrangements and claims staff remuneration scorecards.
We expect insurers to have addressed our expectations by 31 March
2020.
ASIC will consider changes to claims handling practices made by insurers
and superannuation trustees in response to this review and monitor
consumer outcomes including withdrawn claim rates. If we remain
concerned about claims handling practices and withdrawn claims, we will
use our current and proposed powers, including under the Corporations Act
2001 (Corporations Act), to intervene.
We will ask certain insurers selected at our discretion to report to us on the
changes made to their claims handling practices, using our compulsory
notice powers under financial services laws if necessary. We will consider
reporting publicly on the appropriateness of the changes made by insurers
during 2020 and 2021.
We have previously highlighted publicly the need for trustees to improve
their processes around claims handling. This report provides more insight
into areas for improvement and we expect trustees to review their
processes with the benefit of this report by 31 March 2020. We will be
engaging with trustees to review what progress has been made.
Consumer harm
arising from
poor data
(see Section D)
We expect all insurers to:
invest in data resources and improve the quality of their data;
develop plans and timeframes for further developing their data
capabilities to capture, store and retrieve data and information that is
necessary to adequately manage conduct risk and consumer harm;
collect more data including on withdrawn claims, product value,
consumer satisfaction, claim assessment practices, and involvement of
third parties such as legal representatives;
collect data that enables analysis of each individual policy offered
(including where there are multiple covers in one policy), not merely
data aggregated at an insurer level; and
continue to work with APRA and ASIC on the industry-wide collection of
life insurance claims data.
ASIC will recommend to Government strengthening the regulatory
framework for data resources and the management of conduct risk. Our
ability to intervene on issues of data resources and conduct risk
management is limited by the exemptions in s912A(4) and 912A(5) of the
Corporations Act. We recommend that these exemptions be removed.
We will work with APRA, insurers and stakeholders to improve insurers’
data resources. This will include using the types of data fields identified in
Table 14 in this report as the basis for confirming the data capabilities that
insurers need to have in order to capture, store and retrieve data and
information that is necessary to adequately manage conduct risk and
consumer harm.
We will continue to work with APRA to improve the public reporting regime for
claims data and outcomes including considering expanding its existing scope
beyond claims into underwriting and other non-claims areas.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 19
Problem
What we expect of insurers and superannuation trustees
What ASIC will do
Insurers with
higher than
predicted
declined claim
rates
(see Section E)
We expect all insurers to review their claims handling practices in light of
our analysis to ensure they are not treating certain groups of consumers
unfairly. They should also review a statistically significant sample of
declined claims between 1 January 2016 and 31 December with the
claims characteristics set out in Table 23 in this report.
Insurers should complete these reviews by no later than 31 March 2020.
ASIC may ask certain insurers selected at our discretion to report to us on the
outcomes of their reviews, using our compulsory notice powers if necessary.
We may also examine any steps taken by insurers to address the findings of
their reviews. We will consider reporting publicly on insurers’ response to
these expectations.
We may undertake targeted surveillance work to examine the reasons for
substantially higher declined claims rates.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 20
A TPD insurance in Australia
Key points
The growing and main channel by which TPD insurance is distributed is
through group policies; almost 90% of consumers with TPD cover are
insured through their superannuation fund.
Since the publication of REP 498 in 2016, ASIC has undertaken a range of
targeted surveillances and industry reviews to diagnose the drivers of poor
consumer outcomes in the life insurance market.
Important law reforms (such as the product intervention power and design
and distribution obligations) provide ASIC with a more flexible regulatory
toolkit. However, there are still regulatory gaps that restrict ASIC’s ability to
address consumer harm, particularly in the areas of claims handling, unfair
contract terms, licensee resource adequacy, and conduct risk
management. Additional reforms will allow us to address these gaps.
What is TPD insurance?
48 Total and permanent disability (TPD) insurance is a type of life insurance
that pays a lump sum if the consumer becomes totally and permanently
disabled under the terms of the insurance policy. Historically, a TPD
insurance benefit was intended to replace future retirement savings lost by
the consumer when they became disabled. A TPD benefit can also help with
costs of rehabilitation, debt repayments and future costs of living.
49 TPD cover is distributed in three main ways:
(a) group cover—purchased by the trustee of a superannuation fund or an
employer, for the benefit of fund members or employees;
(b) advised or retail cover—distributed through financial advisers; and
(c) non-advised or direct cover—distributed directly by insurers or their
partners or affiliates.
50 TPD policies define ‘totally and permanently disabled’ in different ways. In
2011 the NSW Court of Appeal described the general or ‘common form’ of
TPD definition as:
illness or injury which causes the life insured to be incapacitated to such an
extent as to render the member unlikely ever to engage in or work for
reward in any occupation or work for which he or she is reasonably
qualified by education, training or experience.
Note: See Manglicmot v Commonwealth Bank Officers Superannuation Corporation
Pty Ltd [2011] NSWCA 204
.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 21
Key TPD policy definitions
There are three main definitions of ‘totally and permanently disabled’ used
in TPD policies:
• Own occupation—The consumer is considered totally and permanently
disabled if they are unable to work in their ‘own occupation’ ever again.
Since 2014 this type of cover cannot be held within superannuation,
although some funds offer it as additional cover held outside
superannuation. It is typically more expensive cover.
• Any occupation—This is the general or ‘common form’ of TPD definition.
The consumer is considered totally and permanently disabled if they are
unable to work ever again in ‘any occupation’ for which they are suited
by ‘education, training or experience’. Increasingly, insurers are adding
‘rehabilitation’ or ‘retraining’ to this definition, making it harder to meet.
• ADL—The consumer is considered totally and permanently disabled if
they are unable to meet, usually, three ‘activities of daily living’ such as
feeding, bathing and toileting themselves.
Other types of TPD cover include ‘home duties’ and ‘loss of limbs’. The many
variations on these definitions make it hard for consumers to compare policies.
51 TPD is a complex and challenging product from a consumer perspective.
Sometimes it is difficult for an insurer to reach the conclusion that a person
meets the TPD definition (typically that they are unlikely ever to work
again). Insurers have at times taken a very cautious approach to paying
claims, although they are required to meet their obligations under the policy.
Superannuation is the main way life insurance cover is
provided in Australia
52 The introduction of the Superannuation Guarantee in July 1992 meant that
superannuation coverage expanded considerably—and with it the growth of
life insurance cover within superannuation.
53 Offering insurance cover through superannuation can provide consumers
with default access to beneficial cover at a competitive price, regardless of
their medical history. Superannuation trustees negotiate default coverage
with insurers for a set period (usually three years). Superannuation fund
members (the ultimate consumers) have coverage as specified in the policy
during that period. Trustees may re-tender insurance arrangements and
insurance arrangements may be renegotiated between trustee and insurer,
resulting in changes over time to the level or pricing of default cover, as well
as other aspects of the policy, such as automatic acceptance limits.
54 It is important to note that members only have access to the insurance
coverage in the policy that applied at the time they suffered the injury or
illness leading to the claim. In some cases, the TPD injury or illness could
occur several years before a claim is actually lodged. This means that some

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 22
insurers are liable to cover losses incurred by members of superannuation
funds that they are no longer insuring and no longer collecting premiums for.
55 In 2005 the Super Choice law reforms led to competition between insurers to
acquire and retain group life contracts with superannuation trustees. This
resulted in:
(a) pricing that did not always align with policy benefits—for example, an
increase in default coverage with no corresponding increase in
underlying premium rates, and in many cases a fall in rates;
(b) policies with generous ‘opt in’ features that allowed consumers to take
or increase cover with little or no evidence of health status; and
(c) in some cases—immediate rights to benefit, with ‘at work’ periods of as
little as one day to be eligible to make a claim.
56 These factors contributed to the increased value of TPD insurance through
superannuation. However, the pricing of that insurance was not sustainable
in the long term and has been followed by a tightening of policy terms and
an increase in premiums over the past five years.
Snapshot of the TPD insurance market
57 The TPD insurance market:
(a) is increasingly foreign owned—a series of acquisitions since 2016 has
seen the Australian life insurance industry become majority foreign
owned. Three of the four major banks have decided to sell their life
insurance businesses;
(b) is increasingly group policy focused—data published by APRA for the
2018 calendar year shows that almost 90% of consumers with TPD
cover obtained insurance through their superannuation fund;
Note: See APRA, Life insurance claims and disputes statistics (PDF 623 KB),
December 2018 (released 27 June 2019).
(c) continues to experience a high volume of claims—during the 12 months
to 31 December 2018, a total of 26,150 claims were made on TPD
cover (across all life insurers in the industry); and
(d) continues to experience low profitability—in the 12 months to
December 2018, life insurer net profit from all lump sum risk products
(a subset of which is TPD insurance) fell from $1.4 billion to $509
million, a reduction of more than 64%. This followed significant losses
experienced in the 2013 and 2014 financial years on group life
insurance.
Note: See APRA, Quarterly life insurance performance statistics, 28 February 2019.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 23
58 The most recent life insurance data published by APRA shows that total
annual life insurance premiums to 31 December 2018 were $17.351 billion;
of this amount, $3.548 billion was for TPD cover: see Figure 4.
Figure 4: Total life insurance premiums (millions of dollars), by cover type (at 31 December 2018)
Source: APRA, Life insurance claims and disputes statistics, December 2018 (released 27 June 2019)
Note: See Table 26 in Appendix 2 for the underlying data shown in this figure (accessible version).
59 As at 31 December 2018, there were 16 million lives insured for death cover,
and a comparable number (13.4 million) of consumers who had TPD cover.
For the actual number of lives insured by channel during the period, see
Figure 5.
Figure 5: Total lives insured (in thousands), TPD and death cover (at 31 December 2018)
Source: APRA, Life insurance claims and disputes statistics, December 2018 (released 27 June 2019)
Note: See Table 27 in Appendix 2 for the underlying data shown in this figure (accessible version).
6,390
5,033
3,548
1,469
478
322
111
Death cover
Income protection
TPD cover
Trauma cover
Funeral cover
Consumer credit
insurance
Accident cover
Predominantly
sold in group
insurance
Total premiums
collected for all
cover types was
$17.351bn
16,034
13,299
1,994
555
186
13,456
11,999
1,177
48
232
Total (all channels)
Group (inside superannuation)
Retail (advised)
Direct (non-advised)
Group (outside superannuation)
TPD cover Death cover

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 24
60 Table 4 summarises the total number of TPD claims made during the period
for each channel, highlighting the increasing dominance of the group channel.
61 During the 12 months to 31 December 2018, a total of 26,150 TPD claims
were received across all channels: 14,772 claims were accepted, 2,067 were
declined and 1,619 were withdrawn. At the end of the period 7,692 claims
were undetermined.
Table 4: TPD claims received, by channel and outcome (12 months to 31 December 2018)
Outcome
Claims—retail
Claims—direct
Claims—group
Claims—total
Received (number)
2,691
103
23,356
26,150
Accepted (number)
1,268
36
13,468
14,772
Declined (number)
197
25
1,845
2,067
Withdrawn (number)
298
10
1,311
1,619
Undetermined (number)
928
32
6,732
7,692
Accepted (percentage)
87%
59%
88%
88%
Declined (percentage)
13%
41%
12%
12%
Withdrawn (percentage)
11%
10%
6%
6%
Source: APRA, Life insurance claims and disputes statistics, December 2018 (released 27 June 2019)
Regulatory environment and gaps
ASIC’s previous work to improve outcomes for consumers
in the life insurance industry
62 ASIC published REP 498 in 2016. We identified concerns with TPD
insurance, including the following:
(a) TPD had the highest average declined claim rates—Declined rates
were particularly high for three insurers (37%, 25% and 24%, compared
to an industry average of 16%).
(b) Claims processing times were not consistent with good industry
practice—The average processing time of TPD claims for one insurer
was 21 months.
(c) High rates of withdrawn claims—TPD claims that were notified to the
insurer but did not proceed to an acceptance or decline decision were as
high as 33% for one insurer (compared to an industry average of 10%).

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 25
When claims declined and withdrawn claims are combined, only 65%
of claims notified were being paid.
(d) High rates of policy definition disputes—Over 50% of disputes about
policy definitions were about TPD products and pre-existing conditions.
63 Since the publication of REP 498 in 2016, ASIC has undertaken a range of
targeted surveillances and industry reviews to diagnose the drivers of poor
consumer outcomes in TPD insurance markets. Most importantly:
(a) We reviewed the design and sale of direct life insurance—term life,
accidental death, trauma, TPD and income protection insurance sold
directly to consumers over the phone without personal advice. In August
2018, ASIC released Report 587
The sale of direct life insurance
(REP 587). This report found that direct life insurance was often delivering
poor consumer outcomes, with high rates of lapses and declined claims.
We also identified a direct link between poor sales conduct, including
pressure selling, and poor consumer outcomes. We are now consulting on
our proposal to ban unsolicited telephone sales of direct life insurance.
Note: See Consultation Paper 317 Unsolicited telephone sales of direct life insurance
and consumer credit insurance (CP 317).
(b) We reviewed the role of superannuation trustees in insurance claims
handling and complaints. In September 2018, ASIC released Report 591
Insurance in superannuation (REP 591). This report highlighted a high
level of variation in TPD definitions used in insurance products that
pose significant challenges for consumers in understanding and
comparing insurance cover.
(c) We worked with APRA to develop the Life insurance claims and
disputes statistics publication (APRA-ASIC life claims data collection).
In March 2019, APRA and ASIC released a series of publications and
an online tool on ASIC’s MoneySmart website
allowing consumers to
compare life insurers’ performance in handling claims and disputes.
This was the first time this scale of data had been made publicly
available on an industry and individual insurer basis. This data will be
updated on an ongoing basis.
64 A timeline showing when regulatory action and other significant inquiries
and reforms took place is provided in Figure 6.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 26
Figure 6: Recent regulatory milestones in life insurance
Note: This diagram outlines the time periods for data collected in recent ASIC and APRA reviews of the life insurance industry
alongside the commencement of the relevant Life Insurance Industry Codes. For a description of the commencement of these
Codes, see paragraphs 65–71 of this report. For a description of the findings of the Royal Commission, see paragraphs 72–75.
For a description of the passage of law reform relating to the product intervention powers, see paragraphs 81–83.
The importance of robust industry codes of practice
65 Industry codes play an important part in ensuring that financial products and
services are provided fairly in Australia. Where they enjoy the support and
commitment of the sponsoring industries, codes can deliver real benefits to
consumers and those who are bound by and must comply with them.
66 All life insurers that are members of the Financial Services Council (FSC)
must comply with the Life Insurance Code of Practice (Life Code). The Life
Code came into effect on 1 October 2016 and requires life insurers and those
offering life insurance products to service their customers in a ‘timely,
honest, fair and transparent way’. Insurers were required to comply with the
Life Code from 1 July 2017.
67 The Insurance in Superannuation Voluntary Code of Practice (Insurance in
Superannuation Code) is a voluntary code of conduct for superannuation
trustees. Superannuation trustees who have opted to use this code have until
1 July 2021 to comply.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 27
68 As at the date of this report, 69 superannuation trustees have publicly
adopted the Insurance in Superannuation Code in various forms. The
superannuation industry is largely represented by the FSC, the Association
of Superannuation Funds of Australia Limited, and the Australian Institute of
Superannuation Trustees. These three bodies are the owners of the Insurance
in Superannuation Code owners and are responsible for its development.
69 The period of our review covered the first six months of the Life Code’s
implementation. Compliance with the Life Code is monitored by the Life
Code Compliance Committee. Subscribers to the code must report
significant breaches of the code to this committee and must implement
corrective measures as agreed.
70 The FSC is currently reviewing the Life Code in light of the ongoing
concerns about life insurance highlighted since the code’s implementation,
including by the report of the Parliamentary Joint Committee on
Corporations and Financial Services’ inquiry into the life insurance industry,
and the Royal Commission. ASIC has also provided feedback on the Life
Code, including in relation to our recommendations about the design and
sale of direct life insurance in REP 587
.
71 In Section C of this report, we identify enhancements that should be included
in the next iteration of the Life Code for claims handling practices. In
addition, we consider that the FSC needs to consult broadly and
transparently about enhancements to the Life Code.
Royal Commission into Misconduct in the Banking,
Superannuation and Financial Services Industry
72 The Royal Commission was established on 14 December 2017 to inquire
into past cases of misconduct. The final report was submitted to the
Governor-General and tabled in Parliament on 4 February 2019.
73 Case studies on claims handling practices in life insurance were considered
in the sixth round of hearings, held in September 2018. The case studies
examined practices that had breached financial services laws and/or caused
consumer detriment, and where conduct had fallen below community
standards and expectations.
74 In its final report, the Royal Commission made 11 specific referrals to ASIC
about eight entities. This was in addition to two referrals made during the
Commission’s hearings. ASIC will continue to work closely with all relevant
agencies, including APRA and the Commonwealth Director of Public
Prosecutions, during these investigations.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 28
75 The final report contained 15 recommendations for law reform affecting the
life insurance and general insurance industries, including the following
recommendations that are relevant for TPD insurance claims handling:
(a) Recommendation 4.6—The Insurance Contracts Act 1984 (Insurance
Contracts Act) should be amended so that an insurer may only avoid a
contract of life insurance on the basis of non-disclosure or misrepresentation
if it can show that it would not have entered into a contract on any terms.
(b) Recommendation 4.7—The unfair contract terms provisions set out in the
Australian Securities and Investments Commission Act 2001 (ASIC Act)
should apply to insurance contracts regulated by the Insurance Contracts Act.
(c) Recommendation 4.8—The handling and settlement of insurance
claims, or potential insurance claims, should no longer be excluded
from the definition of a financial service.
(d) Recommendation 4.9—The law should be amended to provide for
enforceable provisions of industry codes and for the establishment and
imposition of mandatory industry codes.
(e) Recommendation 4.10—The Life Code should be amended to empower
the Life Code Compliance Committee to impose sanctions on a
subscriber that has breached the Code.
(f) Recommendation 4.11—The Corporations Act should be amended to
require life insurers to take reasonable steps to cooperate with the
Australian Financial Complaints Authority in its resolution of disputes.
(g) Recommendation 4.13—Treasury in consultation with industry should
determine the practicability, and likely pricing effects, of legislating
universal key definitions, terms and exclusions for default MySuper
group life policies.
Note: See Royal Commission, Final report, February 2019, vol 1.
The need for new powers and tools to address misconduct,
consumer harm and regulatory gaps
76 ASIC has supported the expansion of our powers to address potential
misconduct and consumer harm where there are regulatory gaps.
77 Some of the most significant regulatory gaps exist where there are carve-outs
from the legislation that we administer, including the following:
(a) Claims handling exemption—Many claims handling activities do not
fall within the current definition of providing a financial service, and
others are excluded by reg 7.1.33 of the Corporations Regulations 2001
(Corporations Regulations). The exclusion restricts ASIC’s ability to
take action on claims handling conduct. In 2019 Treasury commenced a
public consultation about removing this exclusion in response to
Recommendation 4.8 of the Royal Commission.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 29
(b) Adequate available resources—The general obligation of an Australian
financial services (AFS) licensee under s912A(1)(d) of the Corporations
Act—namely, to have adequate available resources (including financial,
technological and human resources) to provide the financial services
covered by the licence and to carry out supervisory arrangements—does
not apply to life insurers that are regulated by APRA.
(c) Adequate risk management systems—The general obligation of an AFS
licensee under s912A(1)(h) of the Corporations Act to have adequate
risk management systems does not apply to life insurers that are
regulated by APRA.
78 For consumers, the intrinsic value of an insurance product lies in the ability
to make a successful claim when an insured event occurs. When insurers act
unfairly in claims handling, under the present regulatory regime, ASIC is
limited in the interventions we can take.
79 If the current legislative framework is revised, ASIC could take action for
conduct such as:
(a) incentives for claims staff and management that conflict with the
insurer’s obligation to assess each claim on its merits;
(b) inappropriate claims-handling practices;
(c) unnecessary or extensive delays in handling claims; and
(d) deficient systems and data, which give rise to conduct risk and
consumer harm.
Recent legislative reform
80 Two important pieces of legislative reform were passed in early 2019:
(a) the Treasury Laws Amendment (Design and Distribution Obligations
and Product Intervention Powers) Act 2019; and
(b) the Treasury Laws Amendment (Protecting Your Superannuation
Package) Act 2019.
Design and distribution obligations and product intervention powers
81 The product intervention powers were recommended by the Financial
System Inquiry in 2014. ASIC has long supported these reforms which
strengthen our consumer protection toolkit by equipping us with the power
to intervene where there is a risk of significant consumer detriment. The
power allows ASIC to temporarily intervene including, where necessary, to
ban a product where significant consumer detriment has occurred, will occur
or is at risk of occurring.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 30
82 The product intervention powers came into effect on 6 April 2019. ASIC did
not have these powers when this review commenced. The way in which we
could use intervention powers if necessary in the future in relation to
restrictive insurance definitions is explored in Section B of this report.
83 The design and distribution obligations will require accountability for
insurers, superannuation trustees and other financial service providers to
design, market and distribute financial products that meet consumer needs.
These obligations come into effect on 5 April 2021. The design and
distribution obligations do not apply to MySuper products.
Protecting Your Super reforms
84 The Protecting Your Super reforms apply from 1 July 2019 and prescribe
new arrangements to protect consumers’ superannuation balances from
erosion due to inappropriate insurance and fees. The main features
concerning insurance are as follows:
(a) Cancellation of insurance—Superannuation funds will cancel insurance
on accounts that are inactive for at least 16 months unless a member
opts to keep the insurance.
(b) Inactive accounts—Accounts with less than $6,000 that are inactive for
16 months will be transferred to the Australian Taxation Office (ATO).
The ATO will merge that account with a consumer’s active
superannuation account. If the consumer does not have another active
account, the ATO will keep the consumer’s superannuation safe.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 31
B Poor consumer outcomes from the activities of
daily living (ADL) test
Key points
We found that claims assessed under the ADL definition in TPD policies
had extremely high declined rates. Three in five claims assessed under an
ADL test were declined and some TPD policies had declined rates above
70%, making them effectively ‘junk’ insurance.
Most of this junk insurance was held by default within superannuation. The
design of these products results in certain cohorts of consumers (e.g. casual
employees) being funnelled into ADL-only TPD cover when it may not meet
their needs.
The unsuitability of this type of restrictive TPD cover for consumers is
reflected in the high rate of declined claims for disability caused by mental
illness and musculoskeletal conditions. Consumers with these common
conditions cannot rely on the TPD cover they are paying for.
Eligibility and disability criteria for TPD cover are complex and vary between
policies. Consumers are unlikely to be aware that the ADL definition applies
to them, especially when they pay the same premium as consumers who can
access general TPD cover. Our findings support the need for removal of
overly restrictive terms and for greater standardisation of key terms across
different policies.
The significance of eligibility criteria in TPD cover
85 TPD insurance can play a vital role in consumers’ financial security and
wellbeing. When consumers experience an event that prevents them from
returning to work, TPD insurance can act as a safety net, providing a lump
sum financial payment to replace, for example, future superannuation
savings, as well as contributing to ongoing medical and rehabilitation costs.
86 However, some consumers are paying for TPD cover that they may never be
eligible to claim on, or—if they are eligible—to make a successful claim on.
Our review found that claims assessed under the restrictive definition of
‘activities of daily living’ (ADL) in TPD policies—sometimes called
‘activities of daily working’ (ADW), ‘everyday working activities’ or
similar—generally resulted in very poor outcomes for consumers.
87 We collected data on claims assessed under the ADL definition because it is
the most common of the narrow or restrictive definitions that sit alongside
the broader TPD definitions. Other examples of restrictive definitions are
‘loss of limbs’, ‘permanent loss of cognitive abilities’ and ‘loss of ability to
perform home/domestic duties’. Taken together, around 5% of all TPD

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 32
claims are assessed under these types of definitions, with ADL making up
80% of this figure. Many of our concerns also apply to the other restrictive
definitions used in TPD policies.
Finding 1: Claims assessed under the ‘activities of daily living’ test
generally result in poor outcomes, with three out of five such claims
being declined
88 The average declined rate for claims made under ADL was extremely high,
at 60%. Although ADL claims represented a relatively small percentage of
all TPD claims (4%), this still equates to over three claims per day.
Note: Four per cent of 26,150 TPD claims in 2018 is 1,046 claims. See APRA,
Quarterly life insurance performance statistics
, 28 February 2019.
89 This means that three in five consumers assessed under an ADL definition
for TPD were unable to make a successful claim on their policy. A consumer
assessed under the ADL definition was four times more likely to have their
claim declined than the average consumer for all TPD claims (14%). This
means that some consumers are paying for insurance on which they are
unlikely to make a successful claim if they suffer an illness or injury that
will affect their capacity to work in the future.
90 ADL is suited only to the most debilitating or catastrophic type of injury or
illness. Some portion of the declined claim rate likely reflects the fact that
the disability threshold for ADL is high. Of more concern, however, is that
the high declined rate appears mainly to be caused by eligibility criteria—
because consumers with injuries unsuited to the narrow ADL definition are
forced to rely on it by the terms of their cover.
91 This is particularly apparent in group policies, held by superannuation
trustees to cover their fund members, that funnel cohorts of consumers (e.g.
casual employees) into ADL-only cover when it may not meet their needs.
Given that 4% of TPD claims are assessed under the ADL test, this means
that 4% of the 12 million consumers (480,000) who hold TPD in
superannuation are potentially at risk of unusable or inadequate cover. This
makes TPD poor value and potentially junk insurance for those consumers.
How ADL and other TPD definitions work
Finding 2: Eligibility criteria in group insurance policies mean that
some consumers are automatically funnelled into ADL-only cover
which may not be worth paying for
92 TPD policies vary between insurers. In most cases, they include a general
TPD definition (see paragraph 50), and narrower definitions which apply to
consumers who do not meet certain eligibility requirements under the
general definition.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 33
93 To qualify for a TPD benefit, consumers must generally meet:
(a) threshold eligibility criteria; and
(b) disability criteria (including a waiting period): see Figure 7.
Figure 7: How claims are assessed under TPD policies
Source: ASIC review
Note: See paragraphs 94–103 for a detailed description of the process depicted in Figure 7.
Eligibility criteria in TPD policies
94 Consumers have to meet certain eligibility criteria to access the different
definitions of TPD. For insurance in superannuation, the superannuation
trustee will usually publish information about these eligibility criteria in an
insurance guide or Product Disclosure Statement.
95 Examples of eligibility criteria are employment status (e.g. permanent
employee) and number of hours worked (e.g. minimum of 15 hours per
week) at the date of disablement. Consumers who meet the eligibility criteria
can usually access a broader TPD definition.
96 Conversely, consumers who do not meet the eligibility criteria (e.g. some
casual employees) are unable to access broader TPD cover and may only be
able to rely on more restrictive cover. In this way, consumers are funnelled
into more restrictive definitions as shown in Figure 7.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 34
97 These restrictive TPD definitions may include:
(a) an inability to perform two (or three) activities of daily living, activities
of daily working, or everyday working activities;
(b) an inability to perform normal home duties (for consumers who do not
undertake paid work but engage in home-related activities); and/or
(c) permanent loss of the use of specified body parts (for consumers who
are unable to satisfy any of the other definitions). Some policies also
include permanent loss of cognitive abilities.
98 While each policy varies in its specific eligibility criteria, consumers who
are often funnelled into the narrower ADL definition include:
(a) casual or part-time employees who work less than a specified number of
hours (e.g. 15 hours per week);
(b) seasonal employees;
(c) those who have been unemployed or on leave without pay for a stated
period before the TPD event (often six months, but some policies allow
up to 12 months); and/or
(d) listed occupations that the insurer considers high risk.
99 ASIC is concerned that these types of eligibility criteria unfairly affect more
vulnerable consumers, including unskilled workers, people with parental or
other caring responsibilities, and workers in certain industries such as retail
or hospitality. Aboriginal and Torres Strait Islander consumers who live in
remote areas may also be particularly at risk due to the nature of itinerant
rural work. With the changing nature of the workforce and the growth of the
‘gig economy’, these types of eligibility criteria will capture an increasingly
broad range of consumers.
Disability criteria in TPD policies
100 The disability criteria define the conditions a person must meet to show they
are totally and permanently disabled in accordance with the policy’s terms.
For general, ‘any occupation’ TPD (see paragraph 50), these may include:
(a) the person is not able to perform their usual occupation because of
injury or illness for a specified number of months in a row (also known
as the waiting period); and
(b) in the insurer’s opinion, the person is unlikely ever to be able to engage
in regular paid work for which the person is qualified by education,
training or experience.
101 To satisfy the disability criteria of the ADL test, the consumer must prove
that, after a waiting period, they are permanently unable to perform a set
number of specified activities (usually two but sometimes three). These
‘activities of daily living’ vary between policies. Examples include hearing,

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 35
seeing, speaking, walking, toileting, bathing, writing, feeding, managing
continence, getting in and out of a chair, and lifting.
102 While ‘activities of daily living’ and ‘activities of daily working’ may
sometimes overlap, the activities listed for the latter are usually work-related
(e.g. reading, communicating verbally and moving small objects).
103 The ADL test focuses on the physical activity itself and does not usually
reference:
(a) neurological or cognitive abilities;
(b) the pain involved with performing certain activities; or
(c) the medications required to sustain such activities in the long term (and
the effect of these medications on a person’s cognitive abilities).
Variations in terminology and scope for interpretation
104 The description of each activity included in an ADL definition varies among
policies. For example, the insurance guide for Cbus Personal Super (insured
by TAL) describes communicating as the ability to
:
speak in your first language so that you’re understood in a quiet room and
hear an instruction in your first language said in a normal voice in a quiet
room (even with a hearing aid), or understand a simple message in your
first language, and relay that message to another person.
Note: Cbus, Insurance guide: Personal Super (PDF 2.5 MB), 5 October 2018.
105 This can be contrasted with the policy wording for Local Government Super
(also insured by TAL), which describes communicating differently, as the
ability to:
hear (with hearing aid or other aid if normally used) and speak with
sufficient clarity to be able to hold a conversation in a quiet room in the
Insured Person’s first language.
Note: Local Government Super, Product Disclosure Statement: Accumulation Scheme,
1 July 2019.
106 The differences in eligibility and disability criteria from policy to policy
make it extremely difficult for consumers to compare policies and
understand when they will be covered and what they will be covered for.
Furthermore, complexity and ambiguity in the disability criteria introduce a
level of subjectivity that makes it more likely an adverse claim outcome will
be disputed, either through internal or external dispute resolution or through
the courts, prolonging the stress to consumers of submitting a TPD claim:
see paragraphs 144–148, which discuss the need for greater standardisation
of terms.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 36
Detailed data findings on ADL claims
Three out of five claims were declined when assessed
under ADL
107 Even though ADL claims made up only 4% of total finalised claims in our
review, the average declined rate of 60% is concerning. It means that
consumers assessed under the ADL definition are more likely to have their
claim declined than accepted.
108 When comparing the outcomes of claims assessed under the ADL definition
with those of claims assessed under other TPD definitions, the likelihood of
a claim being declined under the ADL definition is significantly higher: see
Table 5.
Table 5: Outcomes for claims assessed under ADL compared to
other TPD definitions (2016–17)
Definition Declined rate As percentage of
all finalised
claims
As percentage of
all declined
claims
ADL/ADW
60%
3%
13%
Any occupation
12%
91%
79%
Own occupation
14%
5%
6%
Other
40%
1%
3%
Source: ASIC data collection
Note 1: Some insurers could not provide us with data about ADL claims for all of their
superannuation trustees. When data about claims made on policies held by those trustees was
excluded, the proportion of claims assessed under ADL was 4%.
Note 2: ‘Other’ includes a range of different TPD definitions like ‘home duties’ or ‘permanent
loss of limbs’.
Note 3: These declined rates include claims subject to each type of definition that were declined
on the basis of eligibility criteria (e.g. whether the consumer was insured under the policy at the
time of the TPD event).
Declined rates for ADL claims by insurer
109 Our review found a variation in the level of declined ADL claims across
insurers and across different policies for the same insurer. The declined rate
for some insurers and policies raises concerns about the low likelihood of
consumers making a successful claim.
110 Almost all ADL claims in our review (89%) related to a group insurance
policy and almost all the ADL group policies were not underwritten (99%),
meaning that there was no information obtained about the consumer’s
medical history before they were covered by the policy.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 37
111 Asteron had the highest average declined rate for claims assessed under
ADL (79%). It was followed by MLC (70%) and AIA (61%): see Figure 8.
As MetLife was not able to provide us with any ADL data, we were unable
to compare its performance with that of other insurers.
Figure 8: Percentage of declined claims assessed under the ADL test
that went to a final decision, by insurer (2016–17)
Source: ASIC data collection
Note: See Table 28 for the underlying data shown in this figure (accessible version).
112 Significantly, there were also varied outcomes of ADL claims for policies
issued by the same insurer to different superannuation trustees, with some
group policies having a much higher declined rate than others.
113 This variation likely reflects:
(a) different eligibility criteria (e.g. six instead of 12 months of
unemployment before the TPD event date, which would funnel more
consumers into ADL-only TPD cover);
(b) different ADL disability criteria (e.g. inability to perform three instead
of two activities, and how these activities are defined);
(c) the superannuation trustee’s level of engagement with the claim
process, including carrying out its legal obligation to advocate for the
consumer’s claim if it has a reasonable prospect of success; or
(d) a combination of the above factors.
Declined rates for some policies assessed under ADL were
concerningly high
114 Our analysis showed that the declined rates for ADL claims were high across
some group insurance policies for which we were provided data: see Table 6.
As well as several AIA products with high declined claim rates as shown in
Table 6, other policies of concern included the MLC MasterKey policy
issued to NULIS Nominees (Australia) Limited (NULIS) where 73% claims
assessed under ADL were declined.
79%
70%
61%
60%
50%
44%
15%
Asteron
MLC
AIA
All
Westpac
TAL
AMP

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 38
115 It is important to note that:
(a) TAL was unable to provide us ADL-specific claims data for many of its
superannuation trustee clients, including its largest, AustralianSuper
(which made up approximately 10% of all of the claims in our review).
(b) MetLife was unable to provide us with definition-specific claims data
for non-standard TPD definitions, such as ADL and ADW, including
for large trustees like Hostplus and MTAA Super.
116 TAL and Asteron provided us with data showing that one of each of their group
policies also had declined rates above 75% for claims assessed under an ADL
or related definition. We have not included this data in Table 6 because the
relevant superannuation trustees questioned its accuracy. However, it does raise
concerns that both TAL and Asteron continued to underwrite policies despite
their data showing high declined claim rates for a cohort of consumers.
Table 6: Policies with the highest ADL declined claim rates (2016–17)
Insurer Superannuation trustee Superannuation fund Number of ADL
claims finalised
(more than 10)
Percentage of
finalised claims
declined
AIA Government Employees
Superannuation Board (GESB)
GESB Super 16 87%
AIA
LGIAsuper
Local Government Super
11
82%
AIA
GESB
West State Super
29
79%
MLC
NULIS
MasterKey Super
245
73%
AIA BT Funds Management Limited
and Westpac Securities
Administration Limited
Asgard Independence Plan
Two and Retirement Wrap
and Westpac Mastertrust
101 58%
AIA Equity Trustees
Superannuation Limited
SmartMonday Super 23 52%
AIA Sunsuper Pty Ltd Sunsuper—industry
division
62 48%
MLC
NULIS
Plum Personal Plan
11
45%
Source: ASIC data collection provided by the insurers in our review (some figures were changed following feedback from
trustees during our final accuracy review)
Note 1: For some individual policies there were only a relatively small number of claims assessed under ADL. The small number
of claims can lead to higher variability for declined claims.
Note 2: Before November 2017, the SmartMonday policy was held by Aon Superannuation Pty Ltd as trustee of the Aon Master
Trust. The trustee was changed to Equity Trustees Superannuation Limited. The data provided to us showed that more than
90% of claims assessed under ADL were declined in the first instance.
Note 3: Some of these trustees have since entered into arrangements with different insurers to those listed above.
Note 4: GESB is an exempt public sector superannuation scheme (EPSSS) under Sch 1AA of the Superannuation Industry
(Supervision) Regulations 1994 (SIS Regulations), and as such is subject to prudential oversight by the Western Australian
government instead of APRA.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 39
117 The high average declined rate for ADL claims across the industry,
including Australia’s largest insurers, indicates that this is a type of TPD
cover that does not provide value to consumers. As TPD cover is typically
offered by default through superannuation, consumers assessed under the
ADL definition generally pay the same premium as consumers assessed
under the broader TPD definition.
118 While it is the case that some consumers who receive default insurance
cover inside superannuation would find it difficult to get any cover at all
outside superannuation, the cover is of little value if the consumers find it
difficult to successfully claim on it.
Outcomes for mental illness and musculoskeletal
disorders demonstrate the unsuitability of ADL
Finding 3: The ADL test is unsuitable for a range of common illnesses
and injuries, including mental illness and musculoskeletal disorders
119 Our review considered how ADL claim outcomes for various medical
conditions compared with the overall outcomes for TPD claims. When
comparing the primary underlying condition for all TPD claims with the
primary underlying condition for claims assessed under ADL, the profile
was very similar: see Table 7.
Table 7: Primary condition: Proportion of ADL claims compared to
total claims (2016–17)
Primary condition Proportion of ADL
claims
Proportion of all TPD
claims
Disease
36%
30%
Injury or fracture
16%
14%
Mental illness
19%
20%
Musculoskeletal disorders
27%
31%
Other
2%
5%
Source: ASIC data collection
120 However, despite similar claims profiles for the primary condition, the
outcomes for some conditions varied significantly. On average, the declined
claim rate for mental illness claims under ADL was 77%, compared with a
declined claim rate of 15% for mental illness claims excluding ADL.
Musculoskeletal claims also had a significant declined rate under ADL, at
71% compared with 13% for all claims excluding ADL.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 40
121 This means that consumers are approximately five times more likely to be
declined for claims involving either a mental illness or musculoskeletal
disorder when assessed under ADL than when assessed under other TPD
definitions: see Table 8.
Table 8: Primary condition: ADL declined claims compared to all
other declined claims (2016–17)
Primary condition ADL declined claims All declined claims
excluding ADL
Disease
41%
9%
Injury or fracture
60%
15%
Mental illness
77%
15%
Musculoskeletal disorder
71%
13%
Other
89%
13%
All
60%
12%
Source: ASIC data collection
122 Two insurers in our review had very high declined ADL claim rates for:
(a) mental illness—83% for MLC and 81% for AIA; and
(b) musculoskeletal disorders—85% for MLC and 72% for AIA.
123 The concerningly high declined rate for consumers with mental illnesses and
musculoskeletal disorders assessed under ADL indicates that this type of
restrictive TPD cover is unsuitable for many consumers to whom it is being
provided through superannuation. These medical conditions may be a
common cause of disability for certain classes of employees (e.g. manual
workers who may be more susceptible to musculoskeletal injuries and yet
have precarious working conditions that see them funnelled into ADL-only
TPD under the eligibility terms of their insurance policy).
124 Superannuation trustees are ultimately responsible for the insurance benefits
provided through superannuation. A trustee is required, among other things, to:
(a) consider the fund’s membership profile;
(b) design benefits for automatic (default) insurance members with the
objective that the benefits are both appropriate and affordable for
members; and
(c) understand the insurer’s practical application of the definition of
disablement.
Note: See s52(7) of the Superannuation Industry (Supervision) Act 1993 (SIS Act),
APRA Prudential Standard SPS 250
Insurance in superannuation and APRA Prudential
Practice Guide LPG 270 Group insurance arrangements.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 41
125 Considering the needs of different consumer cohorts may require careful
balancing, and some degree of cross-subsidisation is inherent in group insurance
which is about pooling risk. However, we expect insurers and superannuation
trustees not to use ‘junk’ products as part of their design of group policies.
Not all ADL claims had a high declined rate
126 One policy we reviewed demonstrated positive consumer outcomes for ADL
claims. The product issued by TAL to Cbus had an accepted claim rate of
86% under its ‘everyday work activities’ definition (30 out of 35 claims).
127 The following factors may explain the high acceptance rate for TAL’s Cbus
‘everyday work activities’ claims:
(a) The eligibility criteria in the policy are more generous than those of
many other policies, allowing people who have been unemployed for up
to 12 months to claim under the broader TPD definition (compared to the
more common barrier of only six months of unemployment before you
lose access to the broader TPD definition). As building industry workers
may work intermittently on project contracts, the 12-month period
ensures that this time between contracts is sufficiently accounted for.
(b) The disability criteria in the policy are based on an inability to do two
rather than three ‘everyday work activities’.
(c) The disability criteria in the policy are clearer, more concise and more
effective than other definitions we reviewed, setting out specifically and
in plain language what the consumer will be assessed against—for
example, ‘you can’t read ordinary newsprint and pass the standard eye
test for a car licence (even with glasses or contact lenses)’. This not
only makes the criteria easier for consumers to understand but also
reduces subjectivity in the claim assessment process.
128 The higher acceptance rate may also be explained by the claim assessment
model and claims philosophy. Cbus demonstrated high levels of engagement
with its members throughout the claims process. Cbus:
(a) has designated ‘Claims Assist Officers’ who keep in regular contact
with members to assist with all aspects of the claims lodgement process;
(b) reviews claim forms to ensure that the minimum information is
provided by the member before it is sent to the insurer; and
(c) where it considers it appropriate, refers claims back to the insurer for a
second review.
129 This example illustrates the importance not only of the TPD definition itself
but also the role of the superannuation trustee and its own claims philosophy.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 42
Pricing information and data about ADL claims was poor
130 When assessing the profitability, as well as value, of ADL claims, insurers
were generally unable to provide us with financial information for ADL
claims separately from other TPD claims.
131 One of the challenges of offering TPD insurance within superannuation is
the pricing of the policy, which is usually bundled with death cover. As
group insurance is offered to consumers on an automatic-acceptance basis,
there is no individual risk assessment when the cover is provided to
determine whether a consumer will be eligible to claim under the broader
TPD definition or the narrower ADL definition. This eligibility assessment is
only performed at claim time.
132 Further, consumers’ eligibility may well change throughout their working
life (e.g. during periods of part-time work or unemployment), but the pricing
for TPD cover is set according to a general level of risk based on age and,
sometimes, on occupational category. This pricing needs to be informed by
better data about group members.
133 ADL data availability across insurers was inconsistent. MetLife was unable
to provide us with any ADL claims data for the relevant period and TAL
could only provide us with limited ADL data. Some superannuation trustees
also questioned the accuracy of the ADL data provided by some of the
insurers during our final accuracy review.
134 The lack of data availability and accuracy for ADL claims raises concerns
about the ability of insurers and superannuation trustees to:
(a) appropriately assess claim outcomes for TPD consumers;
(b) for trustees—understand their membership profiles; and
(c) use relevant data to design products that are suitable for the groups of
consumers to whom the cover is provided.
135 Section D of this report describes in further detail how insurers often did not
maintain up-to-date information about consumers (e.g. contact details,
occupation status and number of hours worked). This also applies to
superannuation trustees.
Note: Trustees have the obligation under APRA Prudential Standard SPS 250 to maintain
accurate claims records to support identification, monitoring and management of risks
associated with the provision of insurance through superannuation. These records include
claims experience, membership, sum insured and premiums paid in relation to beneficiaries.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 43
Consumer harms from low-value ADL cover
136 TPD policies with eligibility criteria that funnel cohorts of consumers into
ADL cover present multiple risks of consumer harm:
(a) Consumers are paying for insurance they are unlikely to benefit from—
There is a wasted cost to consumers in paying premiums when it is unlikely
that they will be able to receive a benefit under the policy. While offering
ADL in group policies provides cover to consumers who may otherwise not
be able to obtain cover, there is no benefit in providing this cover if
consumers are highly unlikely to be able to make a successful claim.
(b) Consumers are paying the same premium for more restrictive cover—
For default insurance provided through superannuation, which is how
most people have death and TPD cover, consumers pay the same
premium for ADL-only TPD cover as they would if a less restrictive
TPD definition applied.
While cross-subsidisation is a necessary feature
of group insurance, it must be appropriate. This issue was highlighted
by the Productivity Commission:
There is also likely to be cross-subsidisation from inappropriate cover,
‘zombie’ policies that members cannot use (for example, exclusions due to
duplicate [income protection] policies), or where they are subject to more
onerous eligibility criteria.
Note: See Productivity Commission report, p. 390.
(c) Economically vulnerable consumers are disadvantaged—Eligibility
criteria typically target consumers who are more likely to have lower
incomes (e.g. those who have not worked for a specified period or those
employed casually or seasonally). This means that economically
vulnerable consumers are more likely to have their TPD claim declined,
as they are less likely to be assessed under the general TPD definition.
(d) The cost of insurance premiums erodes consumers’ superannuation—
For TPD provided through superannuation, the cost of premiums erodes
the superannuation balance of the consumer. Again, as ADL cover often
applies to consumers who do not work full time or have not worked for
some time, this erosion is even more significant for these consumers,
due to likely low superannuation balances.
(e) Consumers may not be able to rely on cover—Consumers are paying
premiums for insurance cover that they cannot rely on when they need
it, at a time of likely financial hardship due to an incapacity for work.
137 Considering that the purpose of TPD insurance is to provide financial
assistance to consumers experiencing a severe and ongoing medical
condition which renders them unlikely to work again, there are also broader
costs to society when consumers are unable to make a successful claim on
insurance cover they have been paying for. These costs may include reliance
on social security payments or the National Disability Insurance Scheme.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 44
Some insurers are moving away from ADL
138 Since commencing our review, at least one insurer has removed ADL from some
TPD policies offered within superannuation. We also expect other insurers to
review the suitability of their TPD product design in light of our findings.
Other TPD product design issues
139 Table 9 summarises other emerging issues in TPD product design identified
in our review. Product innovation is necessary and important. Some of the
potential benefits that have been identified by the insurance industry include:
(a) increased certainty for insurers around claims performance and pricing;
(b) greater sustainability of products; and
(c) the possibility that consumers may be able to access benefits earlier.
140 However, some of these developments may also contain risks for consumers.
Individual product features have the potential to create risks of poor
consumer outcomes or poor value. They may create unnecessary frictions at
claims time or—where a consumer is asked to continue to prove their
disablement—prevent the consumer from getting on with their life.
Table 9: Emerging issues in TPD product design
Design feature
How it works
Payment by instalment Income-style benefits are paid while the consumer is encouraged to attempt
rehabilitation and/or retraining. This policy design is based on a desire to promote
rehabilitation and a concern that the traditional lump sum TPD benefit has the
potential to provide a perverse incentive since it relies on a person establishing that
they are permanently unable to work. It is also seen as a more sustainable product
from a prudential perspective.
TPD policies that pay benefits by instalment require the consumer to provide
evidence of ongoing disability each year before receiving an instalment payment. At
the time of publishing this report, we are aware of only one insurer in the market
offering this policy where TPD benefits are paid out over six yearly instalments.
Note: See Actuaries Institute, Mental health and insurance (PDF 2.7 MB), green paper,
October 2017, p.14.
Hybrid payments The insurer pays out a portion of a claim at the time the claim is accepted and the
remainder after reassessment. For example, a TPD policy may pay 60% of the TPD
benefit ‘up-front’ and the remaining 40% if the consumer is reassessed as being still
totally and permanently disabled in three years’ time.
Severity policies Different amounts are paid out for different kinds of injury or impairment. Claims are
assessed in a similar way to claims under state government injury schemes.
Sunset clauses These clauses state that there is a time limit for a consumer to lodge a claim from
the date of the TPD event, in line with many state government injury schemes. They
have be
en implemented in some cases by provisions in superannuation trust deeds.
Insurers cannot impose a time limit on claims lodgements.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 45
Design feature
How it works
Continuous care TPD policies commonly contain a term that the life insured will be under the regular
care and attendance of a medical practitioner. Some insurers have moved to a
more restrictive definition to state that the life insured will be under the continuous
direction and professional care of a medical practitioner.
Rehabilitation and
retraining clauses
Insurers routinely provide rehabilitation services to help consumers recover from
injury. Some insurers are tightening their definitions of TPD by including a retraining
and rehabilitation requirement in the policy.
Note: See also Parliamentary Joint Committee on Corporations and Financial Services,
Options for greater involvement by private sector health insurers in worker rehabilitation
,
report, October 2018.
Profit sharing An insurer and a superannuation trustee undertake to divide part of the profits
generated by a successful insurance business. This practice can create a conflict
between the financial interests of the insurer/trustee and their legal obligations to
consider each insurance claim on its merits.
Note: See REP 591, p. 15.
‘Bundling’ of TPD and life
cover
Members of superannuation funds without dependants are sometimes unable to opt
out of life cover while retaining their disability (TPD and/or income protection) cover.
Note: See Productivity Commission report, p. 20.
141 As most of these product design features are still relatively novel, there is
insufficient data available on consumer outcomes for these types of policies.
However, ASIC will closely monitor developments in this area, especially in
light of its new product intervention powers, and the design and distribution
obligations to be phased in before 6 April 2021.
142 Rather than simply tweaking historical definitions in response to the latest
claims experience, insurers must design TPD cover to suit the target market
(as required under the new design and distribution obligations). Insurers
should consider scenarios where a benefit should be paid and where it would
be more appropriate to assist a claimant in retraining and a return to new
work, and design standardised wording to cover those scenarios.
143 We expect insurers offering TPD products to:
(a) collect and analyse claims and claimant-specific data, including
underlying conditions and claimant demographics;
(b) put in place measures to assess the value that the products offer to
consumers, including return-to-work rates, and make changes to
products to address any concerns; and
(c) implement strategies to protect vulnerable consumers and those who
may lack awareness of their insurance cover inside superannuation, and
regularly assess the success of these strategies.
Note: For more on our expectations of insurers and data, see Section D of this report.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 46
Lack of standardisation produces poor consumer outcomes
144 Our analysis of restrictive TPD definitions highlights the problem of
variation in the terminology used across different policies, which can make it
difficult for consumers to understand and compare policies. It can also lead
to ambiguity in the proper interpretation of policies, which in turn can lead
to disputed claims and litigation. ASIC has previously highlighted the
difficulty of comparing TPD definitions in the context of insurance in
superannuation: see REP 591
.
145 Because most consumers are provided with default life and TPD cover when
they join a superannuation fund, the scope for harm from a lack of standard
terms is heightened by a low level of consumer awareness and engagement
with the insurance cover provided by their superannuation fund. The
Productivity Commissioner found that 24% of the members it surveyed did
not know whether insurance was included in their fund, and that a further
16% knew they had insurance but did not know what they were covered for.
Note: See Productivity Commission report, pp. 384, 385 and 390.
146 The Productivity Commission report also recognised that ‘[c]omplexity and
lack of comparability across product offerings is an obstacle that makes
switching to better superannuation products difficult for members’ and that
development of standard definitions ‘including removing opaque and
inequitable exclusions, is a crucial step in reducing this problem’.
Note: See Productivity Commission report, p. 407.
147 Following these reports and further evidence considered by the Royal
Commission, it was recommended by the Royal Commission (and agreed by
the Government) that Treasury, in consultation with industry, should
determine the practicability, and likely pricing effects, of legislating
universal key definitions, terms and exclusions for default MySuper group
life policies: see Recommendation 4.13. Treasury began that consultation
process in May 2019.
Note: We understand that industry will consider standardising key terms for TPD
policies in the next iteration of the Insurance in Superannuation Code.
148
ASIC considers that standardising key terms should assist consumers to
better compare policies and understand the policy they are paying for.
Greater standardisation can provide a safety net for less engaged consumers
as there should be fewer ‘nasty surprises’ in policies when making a claim.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 47
Further action
Strengthening ASIC’s regulatory powers
149 The concerns highlighted in this Section illustrate the need to further
strengthen ASIC’s regulatory powers in relation to insurance products. The
recently granted product intervention powers enable us to intervene where
we see evidence of significant consumer harm. Depending on how insurers
and superannuation trustees respond to the concerns we have identified
about ADL cover, we will consider the appropriate use of these new powers.
150 New design and distribution obligations commencing in 2021 will also be
relevant to how insurers design TPD products, as insurers will need to make
an appropriate target market determination for the product. ASIC will be
able to exercise a number of enforcement powers if these obligations are
breached.
151 ASIC also supports extending the consumer protection regime for unfair
contracts to insurance contracts. If this proposed reform becomes law, ASIC
will conduct further work to assess the fairness of restrictive terms in TPD
policies, including ADL.
What we expect of industry
152 Table 10 summarises our expectations based on Findings 1, 2 and 3.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 48
Table 10: ASIC’s expectations
What we expect
What industry should do
We expect all insurers and superannuation trustees
to:
review all TPD policies that include ADL or other
restrictive definitions and consider removing or
appropriately redesigning the product; and
if redesigning the product, develop measures to
assess the value of the product offered or provided
to consumers.
We expect insurers and superannuation trustees to review all TPD policies that include ADL or other restrictive
definitions, taking into account:
claims data (including declined rates) over the past 10 years for claims assessed under the ADL definition;
premiums;
customer experience data;
ADL eligibility threshold;
ADL disability threshold;
the class(es) of consumers typically insured under the policy in a group insurance arrangement;
outcomes of internal dispute resolution, external dispute resolution and litigation; and
consumer research.
Insurers and trustees should decide whether to:
remove ADL and other restrictive TPD definitions from their MySuper insurance policies; or
redesign the product so that it provides better value for consumers under a policy.
In assessing any new definitions, insurers and trustees are expected to:
develop specific measures to assess the value that the new TPD definition will offer customers;
undertake research into the various consumer cohorts in a group insurance policy; and
conduct trials of any newly designed TPD definition against these measures before market launch.
We expect all insurers and superannuation trustees to
improve data collection on different types of TPD
cover including ADL or other restrictive definitions.
Insurers and superannuation trustees should collect and maintain specific data on ADL and other restrictive
definitions, including:
ADL claims lodged, withdrawn, declined and accepted;
premiums paid by consumers making ADL claims that were lodged, withdrawn, declined and accepted; and
information about consumers lodging ADL claims (e.g. employment status, age, occupation and contact details).

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 49
What we expect
What industry should do
We expect all insurers and superannuation trustees to
improve communication with consumers about the
type of TPD cover they will be eligible for under
various circumstances.
In addition to our expectations for insurance cover disclosure set out in REP 591
, we expect insurers who decide to
keep ADL or other restrictive terms in their TPD policy to clearly and effectively communicate with consumers when
they are or become only eligible under ADL or other restrictive terms (e.g. when they have been unemployed for six
or 12 months or reduce their working hours). This will help consumers make an informed decision about whether the
TPD insurance in their group policy offers any real value to them and whether to opt out of their cover.
Superannuation trustees who decide to keep ADL or other restrictive definitions in their group TPD policy should be
able to:
clearly justify why they have chosen to offer that cover rather than alternative cover; and
explain to regulators and members how the insurance was designed to be in the best interest of members,
balancing affordability with the needs of different members.
For MySuper group life TPD policies
Superannuation trustees must consider our findings when negotiating future group insurance arrangements with
insurers. Trustees should develop their data collection and analysis capability, consistent with existing obligations
under Prudential Standard SPS 250
to better understand the composition and diverse needs of their members, to
ensure their group insurance arrangements are in the best interest of their members.
Using our regulatory powers, ASIC will act where we are satisfied that there is a likelihood of significant consumer
harm.
For all other TPD policies Insurers should be prepared to outline to ASIC, by no later than 31 March 2020, the following information:
analysis, findings and/or conclusions of their work on each policy containing an ADL or other restrictive definition;
the specific measures in place to assess consumer value; and
any changes made to the TPD policy (e.g. removal or redesign of definition, including eligibility) and specific
reasons for the change.
Using our regulatory powers (including product intervention powers), ASIC will act where we are satisfied that there
is a likelihood of significant consumer harm.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 50
C Claims handling and withdrawn claims
Key points
Consumers face a number of hurdles in making a successful TPD claim.
Withdrawn claims are a potential indicator of ‘frictions’ in the claims
handling process leading to consumer harm.
Insurers and superannuation trustees do not have sufficient awareness and
understanding of withdrawn claims and the reasons for withdrawal.
Poor practices when a claim is lodged, as well as during the claim
assessment process itself, can contribute to TPD claimants suffering
additional harm when they are already under stress.
Some insurers and trustees are implementing changes to improve the
claims process for consumers.
Withdrawn claim rates
153 In REP 498 we found that while 84% of TPD claims which went to a
decision were paid out, 10% of TPD claims were withdrawn before a
decision was made to accept or decline the claim. This meant that of all
notified and lodged claims, only 65% were paid. Based on these findings, we
undertook further work to understand the drivers for withdrawn claims.
154 Withdrawn claims are an important indicator of potential consumer harm.
Onerous and/or deficient claims handling processes can lead a consumer to
withdraw a potentially valid claim. The timing and cause of the withdrawal
may indicate where there are problems with, or frictions in, the claims handling
process. Withdrawn claim rates also potentially mask real declined claim rates.
155 Our review found that 12.5% of claims reported in the period or
undetermined at the start of the period were withdrawn—a total of 4,365
claims. We also found that the rate of withdrawn claims varied considerably
across insurers principally because of inconsistent claim reporting practices
between the insurers. At the time of our review:
(a) AMP, Westpac and TAL captured data about claims that did not
proceed to a completed claim form being lodged (such as inquiries); and
(b) AIA, Asteron, MetLife and MLC did not treat a claim as capable of
being withdrawn until a completed claim form had been lodged.
Note: The ASIC-APRA data collection project addressed some of the inconsistencies in
insurers’ claim reporting practices, with APRA issuing Reporting Standard LRS 750
Claims and disputes (LRS 750) in October 2018 to address this issue. However, some
life insurers’ systems still have some way to go to achieve industry-wide consistent,
comprehensive and reliable data (see Section
D of this report).

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 51
Why claims are withdrawn
Finding 4: Insurers do not have sufficient understanding of the
reasons for withdrawn claims
156 As part of our review, we examined a range of onerous TPD claims
practices, drawing on the findings of our consumer research to identify
factors that lead consumers to withdraw claims.
157 We asked insurers to provide us data on why consumers withdraw claims.
We found that insurers’ ability to do this varied and the insights they had
into withdrawn claims were generally poor.
158 We also found that the limited insight insurers had was inconsistent with
information consumers provided to us. This raises doubt over insurers’
understanding of the reasons for withdrawn claims.
Reasons given by insurers for claims being withdrawn
159 While insurers were inconsistent in capturing the reasons for withdrawn
claims there are two broad categories of withdrawn claims:
(a) An active withdrawal usually occurs when the consumer, their
superannuation fund trustee or fund administrator informs the insurer
that the consumer will no longer pursue the claim.
(b) A passive withdrawal is when the insurer notes the claim as withdrawn
if the consumer has not responded directly to a request for information,
or the trustee or the fund administrator notifies the insurer that the
consumer has not responded to a request for information.
160 It was difficult to compare the reasons for withdrawn claims across all seven
insurers in our review due to the difference in lodgement processes.
161 As mentioned at paragraph 155 above, AIA, Asteron, MetLife and MLC did
not treat a claim as capable of being withdrawn until a completed claim form
had been lodged. We examined the reasons given for withdrawal after a
completed claim form was given to the insurer. As Table 11 shows, the two
most common reasons for withdrawn claims at those insurers were:
(a) active withdrawal for reasons other than returning to work or eligibility
to claim on another policy such as an income protection policy (41%);
and
(b) passive withdrawal (40%).
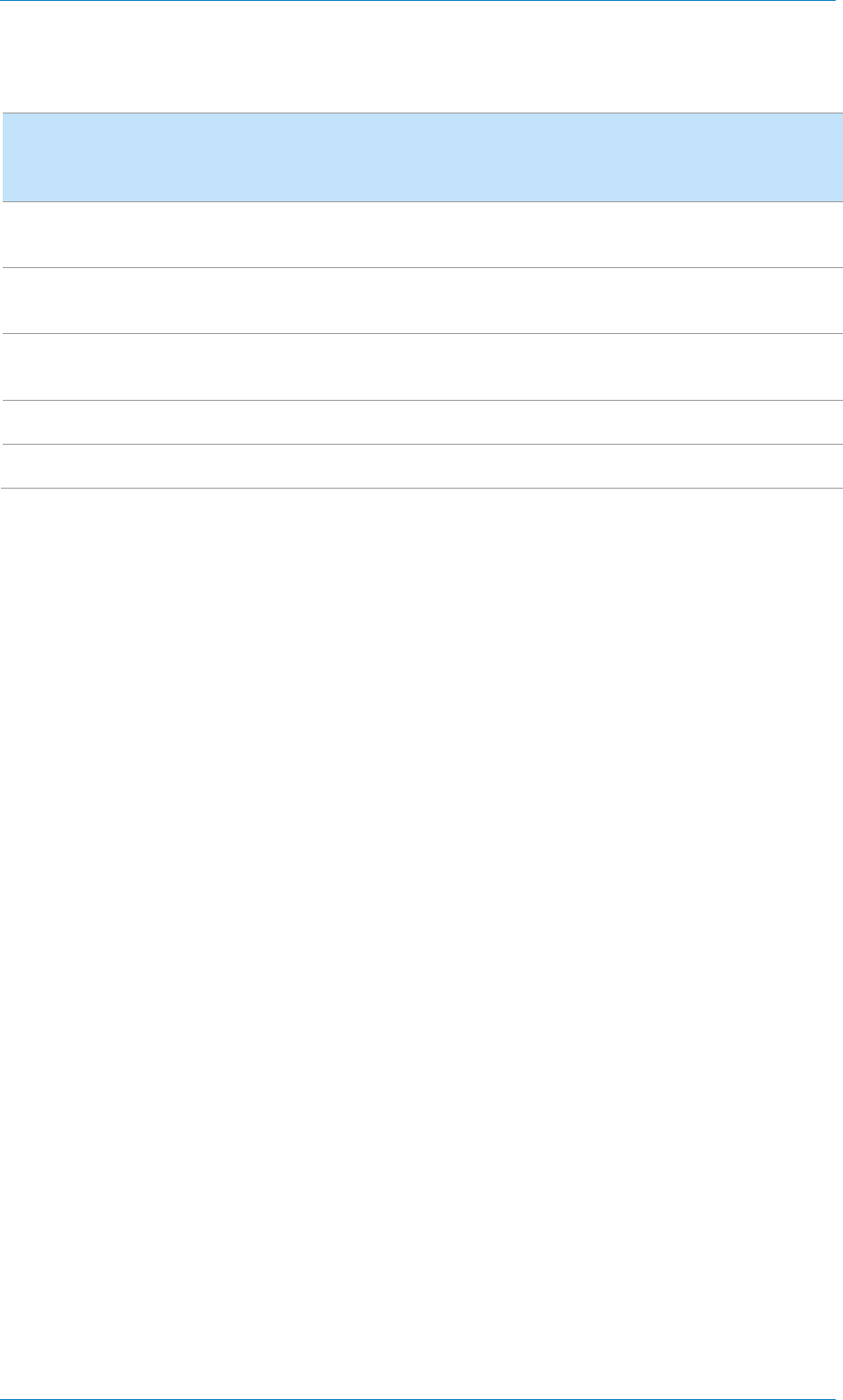
REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 52
Table 11: Reasons for withdrawn claims, by insurer (2016–17)
Reason given for
withdrawn claim
AIA Asteron MLC MetLife Total—for
insurers
shown
No reply/response to
request for information
94 25 61 83 263
Informed by consumer of
decision to withdraw
163 8 41 59 271
Return to work/eligible
under another policy
89 8 25 1 123
Other/unknown
0
0
4
1
5
Total withdrawals
346
41
131
144
662
Note: Only these four insurers provided us with accurate data on the reasons for withdrawn claims.
162 The data limitations meant that even for the four insurers who provided this
data, we were not able to accurately determine the number of active
withdrawals made by consumers who were returning to work. As set out in
Section D of this report, given the current focus on rehabilitation and return-
to-work outcomes, we expect insurers to capture this data in the future.
Reasons given by consumers for withdrawing their claim
163 The reasons given by consumers (and their advocates) for withdrawing their
claims were often different to those given by the insurers.
164 We identified many reasons that consumers withdraw their claims,
including:
(a) onerous and lengthy claim assessment processes;
(b) worsening of the consumer’s medical condition during the claims
process, including (re)emergence of a mental health condition;
(c) having one insurance claim accepted (e.g. TPD, trauma or income
protection) and being unable or unwilling to proceed with another;
Note: Consumers with more than one superannuation account may be covered by more
than one TPD policy and be able to lodge multiple claims.
(d)
cost of pursuing a claim;
(e) being accused by the insurer of fraud; and
(f) embarrassment and/or privacy concerns.
165 The disconnect between the reasons given by insurers and the reasons given
by consumers for claims being withdrawn further highlights insurers’ lack of
understanding of the existing frictions in the claims handling process.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 53
166 While we acknowledge that it is not always possible to know the reasons
behind a passively withdrawn claim, we expect insurers and superannuation
trustees to improve their understanding of the reasons for withdrawn claims,
as these reasons provide opportunities for identifying and minimising
frictions in the claims handling process.
The claim lodgement process
167 After notifying an insurer or superannuation trustee about their intention to
make a claim, the consumer must negotiate the first major hurdle which is
lodging the claim. We found that over 50% of withdrawn claims were
withdrawn within 60 days of claims being notified. This suggests that
consumers may be withdrawing their claims during the lodgement process.
168 We found two specific areas in the lodgement process that can create
significant hurdles for consumers:
(a) the engagement of the superannuation trustee (for group claims); and
(b) the way claim forms and supporting materials are submitted.
The role of trustees and other third parties
169 Under the SIS Act, superannuation trustees have a legal obligation to do
everything that is reasonable to pursue an insurance claim for the benefit of a
beneficiary, if the claim has a reasonable prospect of success: see SIS Act,
s52(7)(d). Our analysis showed the importance of this obligation—we found
that the role played by the trustee in the claims process affects withdrawn
claim rates and is critical at the beginning of a claim.
170 While the first step in any group insurance claim is for the consumer to
contact the superannuation trustee, trustees’ involvement in the claim
lodgement process varies considerably. Some trustees use a triage process
when a member initially notifies the fund of their intention to claim. This
process supports the member to submit claim forms and other required
documents. Other trustees are less engaged, with some being no more than a
‘post box’ for the claim to be sent to the insurer.
Note 1: For more on ASIC’s work to improve the handling of insurance claims by
superannuation trustees, see ASIC’s article ‘Lifting the bar
’, Superfunds magazine, June
2019, pp 16–18.
Note 2: Financial advisers perform a similar role and can assist their clients when their
clients notify them of an intention to claim on a retail policy.
171
Superannuation funds that offer dedicated claims advocates can be
particularly helpful to consumers at this vulnerable and often challenging
time. Cbus, for example, uses a ‘Claims Assist Officer’ and Hostplus uses a

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 54
‘Claim Coordinator’. Their role is to explain the claims process to the member
and ensure that their claim includes the information and documentation
needed for the insurer to begin assessing the claim. Other superannuation
trustees have introduced similar roles to assist their members.
172 We also examined the role of other third parties in the claims process,
including lawyers and advisers. We were concerned that consumers could
suffer harm when the engagement of a third-party adviser leads to a worse
outcome. This can happen when:
(a) consumers engage, and pay for, advisers for claims that the insurer was
likely to accept anyway;
(b) advisers have financial incentives (e.g. ‘no win, no fee’ arrangements)
to have a claim proceed to determination excluding other outcomes that
may be preferable to the consumer such as rehabilitation and returning
to work; and
(c) where a claim is not paid, consumers may be out of pocket due to an
adviser’s fee for service.
173 We found that insurers collected limited data on the involvement of third-
party advisers. Legal representatives were the only type of adviser some
insurers collected data on and even this was inconsistent. Our data showed
that consumers had legal representation in 6,639 out of the 35,026 (18.9%)
claims covered by this review. Consumers with legal representation:
(a) were more likely to have their claim declined (14.4% compared to
8.4%). This may be because some consumers only engage lawyers to
assist when their claim becomes contentious; and
(b) were less likely to withdraw their claim than consumers without legal
representation (3.8% compared to 14.7%). This may because the
likelihood of a consumer withdrawing a claim due to ‘claim fatigue’
will decrease when they have assistance.
174 As noted in Section D of this report, we expect insurers to start collecting
data on the involvement of all advisers in the claims process, including the
date when they first become involved.
175 Our consumer research identified mostly positive consumer experiences of
engaging lawyers to help with a claim. Approximately half of the 20
consumers interviewed had used a lawyer to assist with their claim or claim-
related dispute. A smaller number used a financial adviser. The decision to
use a lawyer or financial adviser was usually made at the beginning of the
process, before the claim was lodged.
176 While these experiences were positive, we consider that insurers and
superannuation trustees can do more to reduce the need for consumers to
engage a third party to assist with their claim. All superannuation trustees

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 55
should consider having dedicated claims advocates to provide support to
members, and insurers should simplify the claims process and make it
transparent and easy. If done successfully, this will reduce the need for—and
potential costs associated with—lawyers and other external third parties to
guide consumers through the claims process.
How claim forms are submitted
177 Lengthy and complex claim forms may act as a prohibitive barrier to
consumers, particularly where the consumer is suffering a mental or physical
illness that makes it difficult, if not impossible, to complete long forms.
178 Our review of insurers’ claim forms found that, while there was some
variation in questions asked, the forms did not vary greatly in complexity or
length among insurers, apart from one insurer, which was AMP.
179 The AMP claim form provided to us was 18 pages long—approximately
three times the length of the other insurers’ claim forms. Many of the
questions appeared unreasonably onerous and several appeared irrelevant to
the initial assessment of a TPD claim.
180 We are also concerned that parts of the form seemed to be designed to:
(a) retrospectively target information which might support declining the
claim based on non-disclosure, whether or not that disclosure is relevant
to the claim event, with questions such as:
(i) which hand do you mostly use?
(i) how much alcohol do you drink on average each week?
(ii) what is your smoking status?
(b) elicit information that could form a basis for AMP to defend declining a
claim, including specific questions about a consumer’s job satisfaction
and performance, such as:
(i) what do you like about your work?
(i) what don’t you like about work?
(ii) do you receive a regular performance appraisal?
181 Such questions could be used to build a case that the reason the consumer
ceased work was not disability but disliking work or underperforming.
182 While the answers to these questions may also inform an assessment of the
consumer’s potential for rehabilitation based on education, training or
experience (part of the common form ‘any occupation’ TPD definition), the
initial claim form is not the optimal time to collect this information. Better
practice we observed is where superannuation trustees and insurers try to get
the minimum essential information from the consumer so that the assessment

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 56
process can start. Additional information can then be obtained as and when
necessary to progress the claim.
183 The negative effect of a long claim form was supported by our consumer
research. One consumer (Harley) commented that the application form
‘seemed to go on forever’, with repetitive questions he felt were designed
‘to catch him out’.
Tele-claim lodgement process
184 To reduce the amount of written information required from the consumer to
start the claim assessment process, some superannuation trustees and
insurers have developed tele-claim lodgement processes where claim details
are collected over the phone. Other supporting information, such as medical
assessment forms, are sent to the consumer after the claim is lodged.
185 Overall, we consider that developments like tele-claim lodgement are
positive as they ease the burden of filling out forms and expedite the
assessment process. One superannuation trustee told us that they give the
consumer a copy of the completed tele-claim lodgement form for them to
check for accuracy, sign and return. Others told us that consumers do not
routinely receive a copy of their claim details to check for accuracy or for
their records.
186 Both the Life Code and the Insurance in Super Code have several obligations
that focus on helping consumers to navigate the claim process. However,
given the findings of our review, we expect these standards to be
strengthened and enhanced in order to improve the claims lodgement
process: see Table 12.
Note: The data we collected for our review captured the first six months of insurers’
activity after adopting the Life Code. The consumers interviewed spoke of claims
mostly under assessment before the Code commenced.
187
We encourage insurers and superannuation trustees to explore all methods
for consumers to lodge claims, such as tele-claim lodgement, paper forms
and online forms, and to make each option available. Where a tele-claim
lodgement process is used, we expect consumers to automatically receive a
written record of the information collected about their claim when it is
lodged, and to be able to correct any errors recorded in the claim form.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 57
Frictions in the claim assessment process
Finding 5: Insurers’ claims handling practices create frictions that
contribute to consumers withdrawing claims
188 Our review identified significant factors which were, or led to, frictions that
cause harm to consumers in the claim assessment process, including:
(a) poor insurer communication practices;
(b) repeated requests for further medical assessments and other supporting
information;
(c) threatening behaviour, including allegations of fraud;
(d) the use of surveillance;
(e) excessive delay;
(f) ‘fishing expeditions’—undertaking a ‘general review’ of a consumer’s
medical history when there is no evidence of potential inconsistency
between underwriting disclosures and claims information;
(g) ongoing costs of the claims process; and
(h) staff training and retention issues, and poor staff incentives.
189 Our consumer research identified instances where a number of these factors
were experienced during the course of a TPD claim.
Note: The names of consumers that participated in the consumer research have been
changed throughout this report as well as some specific details to help maintain their
confidentiality.
Raymond’s experience
Raymond worked as a self-employed tradesman for many years, before an
accident left him with a permanent back injury. Raymond had also
previously suffered from post-traumatic stress disorder (PTSD).
During the year between lodging and withdrawing his TPD claim, Raymond
was assigned a number of different case managers, had to fill out a
‘briefcase full’ of paperwork, and was required to see numerous doctors
and other medical specialists. He felt like this was a tactic by the insurer ‘to
wear him down’ and make him withdraw his claim.
On one occasion, he was asked to get a letter from a health professional
stating whether he was fit to return to work, which they faxed to the insurer.
When Raymond got home, he also scanned and emailed the letter to the
insurer to make sure it was received, as the insurer had lost other
documents he had sent in the past.
The police later arrived at Raymond’s house, stating that the insurer had
made an allegation that he had altered the doctor’s letter and committed
insurance fraud. Raymond showed them the original letter with the fax
stamp, and no further action was taken.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 58
However, Raymond decided he no longer wanted to deal with the TPD
insurer or the claims process, which he felt was aggravating his PTSD, and
so withdrew his claim.
190 This experience illustrates the sometimes onerous and adversarial nature of
the TPD claims process and the cumulative effect of friction points which
can cause a consumer to withdraw their claim. The tactics employed by the
insurer during the claims process clearly exacerbated and worsened the
consumer’s condition, to the extent of triggering a latent PTSD condition.
The importance of transparent, proactive and empathetic
communication
191 Our consumer research showed that the ways in which insurers’ claims staff
communicated with consumers had a significant effect on the consumer
experience, both positive and negative.
Consumer experiences with claims handling staff
Harley had disheartening experiences and rude interactions with the
insurer—a series of three case workers, changed without explanation (and
without briefings from their predecessors), and an in-home interview with
an assessor from the insurance company who he described as ‘quite
aggressive, clinical’ and having ‘no compassion’.
Ken’s case manager was fantastic. She helped with any question or query
about the process and was empathetic: ‘[S]he was a great person to be
doing that [job]. Because you are upset and stressed.’ Ken emphasised
how important it was for him to have had the same case manager all the
way through the process: ‘You build rapport’.
John said: ‘They leave messages with bad news on a Friday afternoon, so
you stress all weekend. People want to deal with these things immediately.
They say, ‘ring me back tomorrow’ knowing they’re not going to be there’.
192 Informative and proactive communication from the insurer is crucial to
effective claims handling. Our consumer research showed that empathy is a
key skill required by staff handling TPD claims. We expect insurers to
design training programs and quality assurance frameworks that ensure
claims are being handled by their staff in a supportive and empathetic
manner.
193 While the Life Code goes some way to support an empathetic claims
process, we consider that more practical and explicit commitments by
insurers are required in order to meet consumer needs. Additionally, insurers
should not unduly rely on the consumer to request updates; the onus should
be on the insurer to proactively communicate with the consumer throughout
the claim assessment process.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 59
Repeated requests for further medical assessments and
other supporting information
194 Insurers’ requests that consumers attend multiple medical appointments was
a theme reiterated throughout our consumer research. We are also aware of
various media reports alleging multiple medical appointments and ‘doctor
shopping’ in TPD claims.
Note: ‘Doctor shopping’ refers to the insurer’s attempt to find a doctor’s opinion that
will support declining a claim.
195
Consumers may also be asked by insurers to provide multiple reports from
their own treating doctors in support of their claim, which can be costly and
time consuming.
196 ASIC acknowledges that there will be legitimate circumstances where more
than one medical examination is needed to determine whether someone meets
the TPD definition. However, our consumer research illustrated the burden
that examinations place on consumers—mentally, physically and financially
(as seen in Raymond’s story). We expect insurers to request only the reports
they need to make a decision on the claim, and to do so in a timely manner.
197 Requesting multiple medical examinations to delay a claim decision or to find
a report favourable to the claim being declined is unfair, inappropriate and
potentially a breach of an insurer’s legal duty of utmost good faith. ASIC will
act where we identify instances of such conduct in breach of the law.
198 We are also aware of allegations of other practices relating to medical
assessments which may be used by insurers to the detriment of consumer
outcomes, including:
(a) ‘doctor-to-doctor framing’, where an insurer’s doctor frames calls to a
consumer’s treating doctor in such a way as to elicit information
potentially prejudicial to the consumer’s claim; and
(b) overuse of or over-reliance on independent medical examinations
(IMEs). The reliability of IMEs has been questioned by some experts,
due to the limitations of a one-off assessment made at a single point in
time by someone with no ongoing relationship with the consumer. This
is especially problematic for conditions that are difficult to assess, such
as some forms of mental illness.
199 While we did not specifically explore these issues as part of our review, we
expect industry to address these risks for consumers, including by
strengthening the Life Code to:
(a) contain standards on how contact between an insurer’s doctor and the
treating doctor should be managed; and
(b) extend commitments relating to the use of IMEs, for example insurers
putting controls in place to ensure that where more than one IME

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 60
request is made per claimed medical condition, the reason for the
decision to request an IME is reviewed for appropriateness by a senior
claims manager and documented accordingly.
Potentially threatening behaviour reported
200 In our consumer research, and in evidence provided to the Royal
Commission (in a case study concerning income protection claims practices,
which can be similar to TPD claims handling practices), we observed
reported instances of insurers engaging in alleged threatening behaviour. The
most egregious conduct reported included:
(a) an account in our consumer research of an insurer making allegations of
fraud to the police (as seen in Raymond’s story);
(b) TAL using an allegation of fraud as a ‘bargaining tool’ in dispute
negotiations with the Financial Ombudsman Service over an income
protection claim; and
Note: See Royal Commission, Round 6 hearings, 13 September 2018, transcript at P-
5725-26 and 14 September 2018, transcript at P-5734.
(c) TAL leading a consumer making an income protection claim to believe
that completing a daily activity diary was required by their insurance
contract, while medical evidence showed that the completion of the
diary was having a negative effect on the consumer’s health.
Note: Royal Commission, Round 6 hearings, 13 September 2018, transcript at P-5719.
See also Royal Commission, Final report, February 2019, vol 2, pp. 335–6.
201 ASIC acknowledges that these are extreme examples of alleged misconduct
by an insurer during a claim assessment process. However, they illustrate
that incorrect allegations of fraud are sometimes made by insurers, and that
threatening behaviour has been used to obtain information that will allow an
insurer to decline a claim, even in circumstances where this action causes
further harm to a consumer’s health.
Note: See also REP 621 Roadblocks and roundabouts: A review of car insurance claim
investigations (REP 621).
202 In REP 498 we set out the guidelines that insurers need to consider when
addressing the risk of fraud. We expect insurers to put in place the necessary
controls to ensure that making allegations of fraud—and engaging police—
are only done on a sound basis. At a minimum, a senior executive from the
insurer and, in group insurance cases, also from the superannuation trustee,
should approve the actions before they are taken. We will be undertaking
targeted surveillances on some of these practices and will consider
enforcement action where appropriate.
Note: See REP 498 at paragraphs 320–324.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 61
Misuse of daily activity diaries
Some insurers ask consumers to complete a record of their activities for a
period of time while on claim, known as a daily activity diary. The insurer’s
rationale for asking consumers to complete this diary is that it may provide
evidence relevant to the assessment of the claim and can also identify
rehabilitation opportunities.
There are two risks associated with the use of daily activity diaries. First,
there is the risk that, for some consumers, the exercise of recording their
activities on a daily basis will result in them constantly reflecting on their
illness and may exacerbate their existing difficulties.
Second, insurers may seek to use a failure by the consumer to complete a
daily activity diary to rely on procedural or technical reasons to reject a
claim or suspend payments, even though the consumer is otherwise totally
and permanently disabled under the policy.
Note: For TAL’s handling of an income protection claim that illustrates both
risks, see Royal Commission, Final report, February 2019, vol 2, pp. 332–41.
TAL has advised ASIC that it no longer allows staff to request that a
consumer complete a daily activity diary as a claim assessment tool.
Instead a daily activity diary may be used as a rehabilitation tool by the
consumer’s treating doctor, with the consent of the consumer.
TAL has advised that it did not use daily activity diaries in TPD claims.
Given the potential for significant consumer harm that can result from the
request for an activity diary to be completed, we expect insurers to review
their practices to determine if there is any valid reason for continuing to use
a daily activity diary as a claim assessment tool. If the insurer deems there
is a valid reason, we expect the insurer to ensure:
• there is a documented clear purpose for cases when an activity diary
may be used as a claim tool;
• the risks of exacerbating the consumer’s health are considered before a
consumer is asked to complete a diary;
• the focus is on using this tool to assist recovery and return to health and
work, rather than trying to identify a reason to reject the claim; and
• senior managers have oversight and monitor the use of activity diaries
by the claim team.
The use of surveillance
203 In our consumer research, seven out of the 20 consumers interviewed
reported that they had experienced additional stress after being subjected to
surveillance.
204 In Raymond’s story, surveillance was a contributing factor to the ‘claim
fatigue’ that led to his decision to withdraw his claim.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 62
205 The misuse of surveillance in life insurance claims has been the subject of
numerous media reports for several years. In REP 498
we acknowledged that
insurers need to address the risk of fraud, including by using surveillance
where appropriate. We also set out good practice guidelines.
Note: See REP 498 at paragraph 322.
206 Since the publication of REP 498, the Life Code has come into effect, and
includes a commitment relating to the reasonable use of surveillance. The Royal
Commission observed that the evidence presented to it indicated that the Life
Code has played a role in reducing the use of surveillance in claims assessment.
Note: See Royal Commission, Final report, February 2019, vol 1, p. 314 and REP 498
at paragraph 322.
207 We were unable to obtain comprehensive, reliable data from insurers on the
use of surveillance, especially desktop surveillance which may include
reviewing social media accounts.
208 Insurers reported that physical surveillance was used in about 2% of TPD
claims finalised or withdrawn between 1 January 2016 and 31 December
2017 (for 675 out of 35,026 claims in total). We found that:
(a) in over 30% of cases where surveillance was used, the claim outcome
was disputed; and
(b) in over 75% of cases where surveillance was used, the insurers
ultimately admitted the claim.
209 Surveillance in claims involving a mental health condition gives rise to a
particularly complex set of issues. As several of the consumer research cases
illustrated, when consumers become aware that they are under surveillance,
this heightens stress and anxiety. Surveillance can therefore exacerbate or
trigger a mental illness.
210 In addition, we question what relevant evidence can be obtained through
surveillance in claims involving mental health conditions. Physical
surveillance would rarely, if ever, provide evidence of the consumer’s
mental health status.
Desktop surveillance
211 Desktop surveillance (also known as digital surveillance) involves
surveillance activities that can be conducted from a computer desktop. It
often involves obtaining information from a person’s social media accounts
and other online searches to verify aspects of a claim. The use of desktop
surveillance by insurers appears to be common.
212 Insurers need to have documented procedures setting out when and how
desktop surveillance is reasonably necessary for a rigorous but fair claim

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 63
assessment process. There are some legal constraints in terms of privacy on
digital surveillance. In addition, insurers must not unreasonably use
information obtained from a person’s social media accounts as a reason for
substantially discounting other evidence such as medical evidence.
Use of Facebook posts in claims assessment
In the case of Hellessey v MetLife Insurance, MetLife declined a TPD claim
partly based on information available on the claimant’s, Ms Hellessey’s,
Facebook page.
The NSW Supreme Court did not dispute the relevance of Ms Hellessey’s
Facebook posts as part of the information to be considered by the insurer
in making a decision on her TPD claim. It also acknowledged that, on a
superficial view, her Facebook posts appeared to be ‘strongly inconsistent’
with the symptoms of her PTSD and depression.
However, the court found that it was unreasonable for MetLife to use Ms
Hellessey’s Facebook posts as a reason for substantially discounting other
evidence that supported her TPD claim (i.e. her own evidence and expert
medical opinions).
In particular, the court found that it was unreasonable for MetLife to
proceed on the basis of its non-expert conclusions about her Facebook
posts without confirmation by medical experts.
MetLife’s decision to decline the claim was overturned at trial, and the trial
decision was upheld by the NSW Court of Appeal.
Note: See Hellessey v MetLife Insurance Limited [2017] NSWSC 1284; MetLife
Insurance Limited v Hellessey [2018] NSWCA 307
.
213 In the draft Life Code update that was released for public comment by the
FSC in late 2018, ‘surveillance’ is defined to mean ‘an investigator filming
and/or observing a person undertaking activities in public’. This means that
none of the safeguards in the Life Code on the use of surveillance will apply
to desktop surveillance.
214 While insurers have the right to make reasonable inquiries to assess the
validity of a claim, we expect that intrusive physical and desktop
surveillance would only be used in exceptional circumstances (e.g. due to a
reasonable suspicion of misrepresentation or fraud). We consider that the
Life Code should include standards for the use of desktop surveillance.
Excessive delay
215 Delay in the assessment of TPD claims was noted as a concern in REP 498
and is reflected in complaints to insurers’ internal disputes departments and
to external dispute resolution schemes. Delay was also an issue for many of
the consumers who participated in our consumer research.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 64
216 The data that we obtained in this review showed that for claims determined
between 1 January 2016 and 31 December 2017, insurers took on average
8.2 months to determine a claim. More recent data collected by APRA in
Life insurance claims and disputes statistics indicates that the average claim
duration has fallen to 5.7 months.
Note: See APRA, Life insurance claims and disputes statistics (PDF 623 KB),
December 2018 (released 27 June 2019).
217 ASIC acknowledges that the assessment of a TPD claim can be complex and
that not all claims are able to be quickly decided. However, clearly many of
the frictions in the claims handling process discussed in this Section
contribute to unnecessary and sometimes excessive delay.
218 Further to these frictions, REP 498 identified reinsurer involvement as
having a potentially adverse effect on claim outcomes. This is because
reinsurers can play an influential role in claims management but are not a
party to the insurance contract and are not subject to the same consumer
protection obligations as insurers. Consumers are usually not aware that the
reinsurer may be actively involved in assessing their claim.
219 Our review found there can be significant differences in outcomes where
reinsurers are involved, in that:
(a) claims involving reinsurers on average took 604 days to finalise
compared with 241 days where there was no reinsurer involvement;
(b) 23% of claims with a reinsurer involved were declined compared with
13% declined where there was no reinsurer involvement; and
(c) 33% of claims with a reinsurer involved were disputed claims compared
with 4% of claims where there was no reinsurer involvement.
220 These results may be due to reinsurers being more likely to get involved in
complex claims or claims above a certain dollar amount.
221 The Life Code sets high-level obligations on reinsurers; however, it does not
set timeframes around how long a reinsurer has to review a claim. Nor do the
claims handling obligations apply to reinsurers. We consider that the
consumer protections of the Life Code should extend to conduct by
reinsurers to the extent that they are involved in claims assessment. This
includes disclosure of reinsurer involvement in the assessment process.
222 We expect insurers to manage the risks associated with the role of reinsurers
in handling claims by:
(a) capturing better data about reinsurer involvement; and
(b) ensuring their reinsurance arrangements are structured so that they
manage claims fairly and transparently, meet the timeframes in the Life
Code, and maintain a consistent claims philosophy across all parties
(including, when relevant, the superannuation trustee).

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 65
223 Under the Life Code insurers have six months to decide a TPD claim. The
Code also sets timeframes for keeping consumers updated on the progress of
a claim (20 business days) and responding to consumer requests for
information (10 business days).
224 Insurers do not need to adhere to these timeframes, however, if ‘unexpected
circumstances’ occur. These can occur, for example, where:
(a) a claim is received more than 12 months after the claim event occurs
and there are resulting delays in obtaining evidence;
(b) for a TPD claim—the insurer cannot ‘reasonably satisfy’ itself that the
claimant meets the TPD definition; and
(c) the insurer has not received reports, records or information requested
from other parties (e.g. the claimant’s doctor, or a superannuation
trustee).
225 ‘Unexpected circumstances’ allow insurers to extend the Life Code
timeframe for a TPD claim from six months to 12 months. However, the Life
Code Compliance Committee has found that not all insurers have accurately
captured or reported on the ‘unexpected circumstances’ that led to delayed
decisions. The committee commented:
If the causes of the unexpected circumstances are not identifiable, [we]
question how subscribers can identify and implement required changes to
their processes to reduce the numbers of claims being determined outside
the normal target timeframes. Criticism of claims handling timeframes was
a significant impetus for the creation of the Code and [we] expect
subscribers to have systems in place to monitor and report on it.
Note: See Life Code Compliance Committee, Life Insurance Code of Practice: Annual
industry data and compliance report 2017–18, March 2019, p. 19.
226 ASIC expects insurers to accurately capture when they rely on ‘unexpected
circumstances’ in failing to meet Life Code timeframes, and to record which
‘unexpected circumstance’ listed in the code applies in each instance.
227 Additionally, given that superannuation trustees are one of the ‘third parties’
relied upon for information, it is imperative that insurers and trustees work
constructively together towards a consistent set of binding standards for life
insurance that covers both insurers and trustees and sets sufficiently robust
standards for all third-party providers.
Concerns about unfairly ‘fishing’ for unrelated non-
disclosures
228 The Royal Commission raised concerns about insurers seeking to avoid
claims by relying on a legal technicality rather than supporting the consumer
through the claims process. TAL’s witness conceded that its conduct in two
of the income protection claims handling case studies amounted to ‘fishing’.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 66
‘Fishing’ is where an insurer undertakes a ‘general review’ of a consumer’s
history without prior evidence of a relevant and substantive inconsistency
between underwriting disclosures and claim information. One purpose for
this type of review can be to obtain information to justify declining a claim
for non-disclosure by the consumer of a pre-existing condition that was
unrelated to the underlying medical condition that gave rise to the claim.
Note: See Royal Commission, Final report, February 2019, vol. 2, pp. 332–3 and 338–
9. Compare Royal Commission, Round 6 hearings, TAL written submissions at
paragraphs 14–20.
229 The data we collected from insurers showed that only a small proportion of
TPD claims were declined based on non-disclosure by the consumer of a
pre-existing condition (234 claims out of a total of 3,400). However, 81 of
the 234 declined TPD claims were by TAL (and this represented
approximately 11% of the total number of claims declined by TAL).
Note: This review was limited to TPD claims; we understand that investigation and
avoidance of policies may be more prevalent for income protection claims. Our
expectations in paragraph 232 apply equally to all life insurance claims including TPD
and income protection.
230
A larger proportion (28%) of Westpac’s declined claims were also based on
non-disclosure of a pre-existing condition; however, this was a smaller
number of claims.
231 Our consumer research revealed instances of policies being avoided for non-
disclosure of a pre-existing condition. For example, Jacob’s TPD claim for
heart disease was initially accepted but later voided due to non-disclosure. The
insurer found that a general practitioner had diagnosed Jacob with a virus some
years earlier and had recommended an MRI, given the virus’ potential effect on
the heart. When Jacob’s condition improved, the GP rescinded the need for an
MRI. The insurer claimed that if Jacob had gone through with the MRI, it may
have uncovered the underlying heart condition. His failure to disclose this
interaction was used as grounds to void his TPD policy.
232 Whether an insurer’s conduct in avoiding a policy for non-disclosure
constitutes ‘fishing’ is invariably difficult to assess. An insurer may need to
conduct investigations to determine whether there has been non-disclosure or
misrepresentation in an application for insurance. However, an insurer must
not conduct an investigation of the consumer’s history to test for non-
disclosure unless it has a reasonable basis to do so, otherwise the insurer is
unfairly engaging in ‘fishing’.
233 We understand that this position will be reinforced in the next iteration of the
Life Code. We also expect insurers to ensure that their practices when
investigating potential non-disclosure do not give rise to ‘fishing’. This
includes ensuring that they have robust supervision and monitoring
processes in place.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 67
Ongoing financial costs of the claim assessment process
234 The consumer research stories highlighted the ongoing financial costs to a
consumer that are associated with a TPD claim. In the context of a claim
made by a consumer who is unable to work and may be vulnerable and
suffering financial stress, these financial costs may contribute to a decision
to withdraw a claim.
235 Raymond, for example, had to travel from a regional centre to a state capital
for numerous medical examinations, and recalled the experience as being
‘time consuming, costly and painful’. Another consumer, Ellen, highlighted
a lack of flexibility about the times she was required to attend medical
examinations and the fact that ‘parking and travel costs were not covered’.
236 Several other consumer research stories highlighted the indirect costs of
time, number of communications (including by post) and incidental tasks
such as obtaining authentication of documents by a justice of the peace. As
these stories show, consumers making claims incur direct financial costs as
well as indirect opportunity costs.
237 The Life Code commits insurers to covering ‘any extraordinary travel costs
we agree in advance’ for consumers to attend an IME (Section 8.10), but not
other costs.
238 ASIC considers that the Life Code should be strengthened to provide clarity
around when reasonable financial costs which consumers incur in the claim
assessment process will be reimbursed by insurers, particularly for
vulnerable consumers such as regional or remote consumers, or for
protracted claims. This could include reasonable costs associated with:
(a) transportation to attend medical examinations initiated by the insurer,
including parking and petrol;
(b) postage;
(c) extraordinary telephone and internet use;
(d) lost work time of carers who assist consumers to attend medical
examinations;
(e) arrangements for getting copies of documents certified; and
(f) accountants’ fees for compiling financial documents to support a claim.
Problems with staff retention, training and incentives
239 In REP 498 we noted that insurers need to have an adequate number of
suitably trained staff and that claims should be allocated to claims staff who
have the right skills. This is also a requirement under Section 8.20 of the
Life Code. In REP 498, several insurers reported that it was difficult to
recruit and retain claims staff with the appropriate skills and experience.
Note: See REP 498 at paragraphs 330–331.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 68
240 Staff training and retention issues can lead to problems with:
(a) correctly interpreting and applying policy terms to assess a claim;
(b) providing adequate support to the consumer during assessment;
(c) assessing a claim in a timely manner; and
(d) having multiple case managers involved in a claim.
241 These problems can result in a range of frictions being experienced by the
consumer. Our review found that the issues identified in REP 498
have
continued. Recruitment and retention of claims handling staff is an industry-
wide challenge with competition for experienced, suitably trained and high-
performing claims staff being extremely high.
242 All the insurers gave us the percentage of TPD or life insurance claims staff
who had left their firms during the two-year review period, and the staff
turnover rates they considered acceptable. While there were slight
differences in methodologies insurers used to calculate these rates, this data
indicated that several insurers had a claims staff turnover rate which was:
(a) above their acceptable rate for one of the two years; and
(b) around or above 25% for one of the two years—that is, more than a
quarter of the staff in the claims team with responsibility for overseeing
TPD claims left the insurer during the calendar year.
Note: These rates were only for staff leaving the insurer (and not, for example, moving
to another role internally).
243 All insurers in this review told us that they assigned a dedicated case
manager to provide a single point of contact for consumers who had made a
TPD claim. However, with the high level of staff turnover noted above, and
given that TPD claims take on average 5.7 months to finalise and 28% of
claims take longer than six months, there is a high chance that consumers
will have their claim handled by more than one case manager.
Note: See APRA, Life insurance claims and disputes statistics (PDF 700 KB), June
2018 (released 29 March 2019).
244 Our consumer research found a clear link between a poor claims experience
and multiple case managers. Multiple case managers can lead to consumers
having to explain their claim to different staff and/or provide the same
documentation more than once. It may also result in inconsistent information
being given to consumers about their claim.
245 Staff incentives, while potentially useful for recruiting skilled staff, can also
create risks for consumers. We found that since the publication of REP 498
all insurers had removed declined claim rates as a direct performance
measure in scorecards. However, Asteron set financial reserve targets as a
measure to meet performance goals.
Note: We found that conflicts of interest in remuneration could be an issue for insurers
who used incentives and performance measures for staff based on declined claims: see
REP 498
at paragraphs 332–333.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 69
246 We consider that indirect financial incentives like this may also give rise to a
conflict of interest and incentivise staff to decline claims—since the most
direct way a claims assessor can meet financial reserve targets is to decline
claims. While this is more of an issue for income protection claims—where
the reserves that need to be held by insurers are often considerably higher
than for lump sum TPD claims—it can still influence behaviour and result in
unfair consumer outcomes.
247 To address these retention and training issues, we expect insurers to:
(a) have clearly documented guidelines about the training and competency
requirements that claims handling staff must attain to manage claims
and make claim decisions;
(b) assess the effectiveness of handover processes and apply targeted
monitoring and supervision to claims where there has been a change in
case manager. We consider this to be vital; and
(c) remove direct and indirect insurer financial targets (including financial
reserve targets) from the remuneration scorecards of claims staff and
managers, including senior claims management.
Further action
Strengthening ASIC’s powers
248 The concerns highlighted in this Section illustrate the need to strengthen
ASIC’s regulatory powers in relation to claims handling by removing the
exemption for ‘insurance claims handling’ from the conduct provisions of
the Corporations Act.
249 The Royal Commission recommended, and the Government agreed, to
remove this exemption. Enhancing ASIC’s powers in this area will allow us
to better monitor and act on potential misconduct and consumer harm in the
handling of TPD insurance claims.
What we expect of industry
250 Table 12 summarises our expectations based on Findings 4 and 5.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 70
Table 12: ASIC’s expectations
What we expect
What industry should do
We expect the claims handling provisions of
the Life Code and Insurance in Superannuation
Code to be strengthened, and for insurers and
superannuation trustees to develop a
consistent set of binding standards for life
insurance.
We expect insurers and superannuation trustees to ensure that the next iteration of the Life Code and, where relevant,
the Insurance in Superannuation Code incorporate or enhance standards for:
streamlined lodgement practices, including tele-claim lodgement and simplification of forms;
proactive communication with consumers;
appropriate insurer (or third-party provider) contact with treating doctors regarding IMEs and putting controls in place
to ensure that where more than one IME request is made per claimed medical condition, the reason for the decision
to request an IME is reviewed for appropriateness by a senior claims manager and documented accordingly;
appropriate use of daily activity diaries;
appropriate use of desktop surveillance; and
insurers having documented guidelines on the training and competency requirements that claims handling staff must
attain to be able to manage claims and make claim decisions.
Insurers and trustees should work constructively together towards a consistent set of binding standards for life
insurance that covers both insurers and trustees and contains robust standards for third-party providers such as
administrators.
We also expect insurers to reduce delay in the assessment of TPD claims by accurate reporting of ‘unexpected
circumstances’ to the Life Code Compliance Committee.
We expect our recommended changes to
claims handling practices to be implemented by
insurers and superannuation trustees by 31
March 2020.
We expect insurers and superannuation trustees to:
take immediate steps to implement our recommended changes to claims handling practices; and
not enter into agreements with reinsurers on terms that are inconsistent with the agreements between insurers and
relevant trustees, and to maintain better data and records about reinsurer involvement.
Insurers should be in a position to outline to ASIC, by 31 March 2020, the steps taken to implement our recommended
changes to claims handling practices. ASIC will consider publicly reporting on insurers’ responses to this expectation.
We have previously highlighted publicly the need for trustees to improve their processes around claims handling. This
report provides more insight into areas for improvement and we expect trustees to review their processes with the
benefit of this report by 31 March 2020. We will be engaging with trustees to review what progress has been made.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 71
What we expect
What industry should do
We expect direct and indirect financial targets
to be removed from all claim scorecards,
including those of senior management.
We expect insurers to remove direct and indirect financial targets from the remuneration scorecards of claims staff and
managers, including senior claims management. This includes:
making a component of remuneration scorecards dependent on the insurer or claims department meeting profit
targets including loss ratio targets, average cost per claim, return on surplus and return on equity targets. Where the
insurer is part of a wider corporate group, this includes the performance of that wider group;
making a component of remuneration scorecards dependent on the performance of the staff member’s leader when
the leader’s remuneration scorecard is dependent on the insurer or claims department meeting profit targets; and
making a component of remuneration scorecards dependent on meeting financial reserve targets.
We expect insurers to have addressed our expectations by 31 March 2020. ASIC will consider reporting publicly on
insurers’ responses to this expectation.
We expect claims training and handover
practices to be robust enough to manage high
turnover rates and difficulty in recruiting
experienced staff.
Insurers and, where appropriate, superannuation trustees should:
review training programs and ensure they are tailored to meet the specific needs of staff recruited from non-life
insurance backgrounds; and
review claim handover practices and associated controls (e.g. quality assurance monitoring and supervisory
processes) to ensure that consumers’ claim experiences are not negatively affected by a change in claims staff.
Consumers should not have to restate claim details or resubmit claim documentation because of staff changes.
We expect insurers and (where appropriate) trustees to have addressed our expectations by 31 March 2020. ASIC will
consider reporting publicly on insurers’ responses to this expectation.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019
Page 72
D Poor-quality data and consumer harm
Key points
Insurers need good-quality data to manage the risk of consumer harm. It is
required for effective business management and to ensure good consumer
outcomes.
To varying degrees, all seven insurers in our review failed to meet our
criteria for ‘good data’ during the review period. Because of this none of the
insurers in our review could, in ASIC’s opinion, effectively manage the risk
of consumer harm.
Despite recent improvements, insurers still have a considerable way to go.
We expect insurers to make further investments in their data resources and
associated systems to address this issue. We will report publicly during
2020 on insurers’ responses to the issues we have identified.
251 We reviewed the quality of the data provided to ASIC and available to each
of the insurers during the 2016 and 2017 calendar years against the
characteristics of good data in Table 13. To varying degrees, all seven
insurers failed to meet most, if not all, of our criteria for adequate data
capability during the review period.
252 ASIC is of the view that because of this, no insurer could proactively
identify claims where breaches of the law or unfair treatment of consumers
were likely to occur. Insurers could not accurately and comprehensively
identify:
(a) the value of products to consumers and whether the products are
meeting consumer needs;
(b) key friction points in the TPD claims handling process;
(c) claims handling staff whose conduct may give rise to a higher
likelihood of consumer harm;
(d) claims handling practices leading to consumer harm; and
(e) harm caused to consumers at either a granular or a consolidated level.
253 This means insurers could only get this information from reactive, post-event
quality assurance reviews, audits or data analysis. By this time consumer
harm will have already occurred.
254 In ASIC’s view, it was therefore not possible for any of the insurers in our
review to appropriately manage the risk of consumer harm during the review
period (between 1 January 2016 and 31 December 2017).

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019
Page 73
Good data is essential for managing the risk of consumer harm
The importance of good data
255 Good data is required for effective business management and to ensure good
consumer outcomes. Without it, insurers cannot manage the risk of
consumer harm, measure consumer outcomes, or benchmark their
performance against industry best practice.
256 Good data is also integral for ASIC to be able to perform our regulatory
functions under the ASIC Act. As the Productivity Commissioner recently
noted, good data is a ‘must have’ for strategic conduct regulation and pre-
emptive surveillance. The assessment, evaluation and analysis of data are
crucial for ASIC to identify the important problems under our remit and
develop ways to fix them. We cannot achieve our vision of a fair, strong and
efficient financial services system if firms cannot provide timely data that we
can rely on. Poor data prevents us from achieving this vision.
Note: See Productivity Commission report, p. 506 and Malcolm K Sparrow, The
regulatory craft: Controlling risks, solving problems and managing compliance,
Brookings Institution Press, Washington DC, 2000, pp. viii and 261.
257 The availability of good-quality data is necessary for insurers to be able to
manage the risk and perform detailed analysis of potential consumer harm,
such as the following:
(a) Manage their exposure to conduct risk that gives rise to consumer
harm—Conduct risk is the risk of loss to a firm or its customers caused
by inappropriate, unethical or unlawful behaviour by a firm’s
management or employees. When conduct risk crystallises it can result
in consumer harm—both direct financial harm (e.g. from paying
premiums for cover they cannot claim on) and non-financial harm (e.g.
from unfair claims practices causing, or aggravating, a mental health
condition). If insurers effectively manage their exposure to conduct risk,
they will proactively manage consumer harm.
(b) Undertake ongoing tracking of product value—Tracking the value of
insurance products for consumers helps insurers to provide products
that are fit for purpose and delivered with due care and skill.
(c) Compare different indicators of consumer harm—Relevant indicators
include when and why claims are withdrawn, when and why consumers
complain or are dissatisfied with the claims process, and when
consumers turn to advisers such as lawyers to help with claims. This
type of analysis can identify points in the claims process that cause
‘friction’ and give rise to consumer harm.
(d) Develop proactive quality-assurance, peer review and performance
management processes—By identifying claims where there is a higher
likelihood of consumer harm based on lead indicators, insurers can

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019
Page 74
develop proactive quality assurance, peer review and performance
management procedures to ensure that laws are not breached and that
consumers are not misled or deceived but are treated fairly.
(e) Forensically analyse behavioural patterns of claims handling staff and
claims handling teams—The aim of this is to identify claims handling
staff where there is a higher likelihood of consumer harm. This type of
analysis would help ensure that claims staff act in the best interests of
consumers.
The characteristics of good data
258 We found that insurers’ data should have five characteristics to enable
insurers to effectively manage the risk of consumer harm. These are set out
in Table 13.
Note: In developing this list, we considered the work of several expert bodies, in
particular the Basel Committee on Banking Supervision: see
Principles for effective risk
data aggregation and risk reporting (PDF 130 KB), January 2013. We tailored that
work to fit the purposes of claims-related conduct risk and consumer harm.
Table 13: What good data looks like
Characteristic
Why it is important
Timely Good data is as close to ‘real time’ as possible. Firms need to be
able to generate lead indicators if they are to predict the likelihood
of conduct risk crystallising and resulting in consumer harm.
Accurate Good data is correct, reliable and unambiguous. Firms cannot
predict the likelihood or effect of conduct risk and consumer harm
if the data they depend on is unreliable.
Adequate Good data has a sufficient quantity of searchable data points.
Firms must capture enough data fields in a searchable format to
be able to conduct analysis necessary to predict the likelihood
and effect of conduct risk crystallising resulting in consumer harm.
Complete Good data is sourced from all stakeholders in a claims process
(e.g. insurers, superannuation trustees, administrators and other
service providers) and gives a view of the whole claims process
that is not firm-specific. To manage conduct risk and consumer
harm, insurers must have access to relevant data from all
stakeholders. Without this their data is not ‘complete’.
Consistently
defined
Good data has consistently defined terms and inputs. Firms
cannot measure and compare their exposure to conduct risk and
consumer harm against industry benchmarks if key data terms are
defined differently.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019
Page 75
Insurers had poor data
Finding 6: Insurers did not have adequate data to effectively manage
the risk of consumer harm
259 Insurers were unable to meet our definition of good data during the review
period for the following reasons.
Insurers responded slowly to statutory notices
260 In February 2018, we issued compulsory notices which required insurers to
produce the minimum amount of data that we considered necessary for an
insurer to manage its claims-related conduct risk.
261 We required insurers to respond within six weeks. We were still waiting for
responses from some insurers five months after we issued these notices.
262 Several stakeholders commented that ASIC appears to expect firms to be
able to provide it with data ‘at the press of a button’. Historically this was
not possible, but the advent of ‘big data’, artificial intelligence and cloud
computing increasingly makes this achievable. If insurers are envisaging a
world where they will soon be able to ‘continuously underwrite’ based on
‘wearables’ data, we consider that they should have ready access to a high
number of consistently defined, accurate and searchable data points.
Insurers did not have all data in searchable formats, with
some fields not available even by reviewing case notes
263 During our review, it became clear that all insurers, to varying degrees, were
unable to readily produce several data fields that are crucial to understanding
a consumer’s claims journey and whether they experienced harm.
264 To produce this data, all seven insurers had to manually review case notes.
265 For example, one insurer had to conduct manual reviews to extract 36 of the
78 data fields, including the reason the insurer declined the claim, the TPD
disability definition under which the claim was assessed, and whether the
consumer had a legal representative acting on their behalf during the claims
process. Another insurer had to extract six of the 78 fields from paper files
and could only provide a sample response.
266 Some insurers were not able to provide data even with manual review of
case notes. The data fields that individual insurers were, in some cases,
unable to provide, included:
(a) data to assess the value of TPD products to consumers;
(b) data on different TPD definitions that claims were assessed under;
(c) data on the secondary cause of the claim;

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019
Page 76
(d) reasons for a claim being reopened;
(e) the postcode of the consumer’s home address; and
(f) data on when consumers were engaging external claims advisers (other
than lawyers).
Data on the value to consumers of TPD products
There is a clear, industry-wide lack of data that can be used to measure the
value to consumers (or groups of consumers) of TPD products.
In November 2018 we asked 12 insurers to provide key data for each of
their TPD definitions, including loss ratio data. This was to assess the value
of TPD to consumers assessed under an ADL or ADW test.
Only three insurers could do this. Only one insurer could provide loss ratios
for ADL and ‘any occupation’ separately. Two insurers were unable to split
profits (or even estimate a split of profits) for combined products such as
death and TPD cover, let alone for individual TPD assessment definitions.
There were also inconsistencies in the methods used to calculate
profitability among the insurers. For example, some insurers calculated
profit as a percentage of earned premium net of reinsurance, while others
calculated profit as a percentage of gross earned premiums. Some insurers
included investment earnings in their profit, while others did not. This made
it impossible to compare product value between insurers.
Being able to assess the value of products to consumers—and different
groups of consumers—is crucial to managing conduct risk and consumer
harm. It goes to the heart of offering products that are fit for purpose.
All insurers’ responses contained errors
267 Each insurer provided data with significant data quality issues. Some of
these issues remained apparent when insurers resubmitted their data after we
notified them of the problem.
268 The issues that we found included:
(a) duplicate entries for claims and disputes;
(b) dates provided that were not possible, for example:
(i) dates when claims were finalised before they were lodged;
(ii) dates when claims were referred to the chief medical officer of the
insurer before they were lodged;
(iii) dates for decisions on withdrawn claims (where there had in fact
been no decision about the claim); and
(iv) dates when claims were finalised before the date a decision was
made on whether to accept or decline the claim;

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019
Page 77
(c) data provided for group policies where the name of the relevant
superannuation trustee was missing;
(d) payment amounts for undetermined and withdrawn claims (for
undetermined and withdrawn claims there should be no payment amount);
(e) reinsurance payments to insurers that were higher than the total amount
paid out on the claim;
(f) responses for disputes without the dates on which the disputes were
lodged and resolved;
(g) claims classified as not reopened that included reopened dates;
(h) negative duration values for claims; and
(i) claims and disputes that fell outside the relevant period of ASIC’s request.
269 Many of these issues were easily identifiable. Sometimes insurers resubmitted
these mistakes after we had asked them to check their response and resubmit.
Note: As set out at paragraph 344 of this report, when ASIC conducted a final accuracy
review before publishing this report, errors in the data provided by two of the insurers
were identified. For a range of reasons, including materiality, this data has not been
changed in this report and does not change the findings or recommendations. However,
it reiterates our finding that insurers were unable to meet our expectations for good data
during the review period.
270
These mistakes, particularly in the context of a legal requirement to provide
this data under our information-gathering powers, raise concerns about the
adequacy of insurers’ internal reporting capabilities. It suggests that insurers’
core system rules may be poorly implemented, resulting in illogical and
contradictory information being recorded on a claim.
Inconsistent responses to requests for data from regulators
As noted at paragraph 63, since 2017 APRA has been collecting claims
data from life insurers. The data that APRA collected was not as granular
and detailed as the data we collected for this review; it also covered
different time periods. However, for the period which overlapped, the total
number of TPD claims for that period should have been consistent.
This was not the case for the data that one insurer provided to ASIC.
There was a significant difference in the number of finalised, withdrawn and
undetermined TPD claims given in the two responses. Approximately 39%
of the data that was provided to APRA under the public claims data
reporting regime was not reported to ASIC in this insurer’s response to our
notice. The insurer eventually explained this mistake as being the result of
omitting one particular cohort of group insurance claims.
We consider that such an obvious discrepancy in response to the use of
ASIC’s and APRA’s compulsory information-gathering powers raises
significant concerns about the accuracy of this insurer’s claims data and
the thoroughness of its data quality assurance processes.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019
Page 78
271 In addition, contact lists provided by the insurers to ASIC to source participants
for our consumer research further illustrated poor data management practices.
This included key contact details not being recorded or recorded incorrectly.
This would make it difficult for insurers to contact claimants and could account
for why some do not respond to communications or requests for information
from insurers and are considered to have passively withdrawn their claim.
One insurer’s reliance on paper files
One insurer relied on paper files for over a third of TPD claims in 2016 and
2017. These claims were managed on legacy systems.
We highlight two concerns with this practice:
• Some files were lost—The insurer notified us that some of the detail for
2,020 out of the 5,327 claims it handled during 2016 and 2017 were held in
paper format only. Given the difficulty in retrieving from archives and
manually reviewing paper files, we agreed that the insurer could sample 381
of the 2,020 paper files. The insurer was not able to locate 21 of 381 files.
• There were differences between paper files and system records—In some
cases, the claims details recorded on the insurer’s system were different
to the paper record of the claim. For example, a sample of 137 declined
and withdrawn claim files were selected for external review of the
insurer’s claims handling practices. The external reviewer was unable to
review 20 of these files: 10 files could not be located, 7 were found to be
admitted claims (and therefore outside the scope of a review of declined
and withdrawn claims), and 3 were incomplete, with insufficient
information available to complete the testing required.
There were no common standard definitions for key data
fields across the seven insurers
272 During 2016 and 2017, insurers lacked common definitions for several key
claims data fields.
Note: This was consistent with what we found in REP 498 at paragraphs 10–11.
273 This lack of consistency was particularly problematic in the notification and
lodgement of claims—that is, in how different insurers recorded when a
claim ‘begins’. Some insurers recorded a claim as having begun as soon as a
consumer notified them that they were considering making a claim, while
others required a claim form to be submitted. In some cases, insurers only
recorded a claim when the consumer provided enough evidence to complete
a claim assessment.
274 There were other differences, including:
(a) how insurers captured (as well as monitored and analysed) ex gratia
payments, with several insurers advising us that they had no formal
monitoring, analysis or reporting of ex gratia payments); and
(b) the reasons why a claim was declined or withdrawn with some insurers.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019
Page 79
275 ASIC had to undertake an extensive cleansing exercise to improve the
consistency of insurer data. Despite this, we were still unable to ensure the
consistency of data relating to withdrawn and disputed claims.
276 Since the release of REP 498 in November 2016, insurers have undertaken to
adopt greater consistency in their definitions. We are concerned that it took
regulatory action to bring about these changes.
Insurers did not have access to all data about group
insurance claims
277 In 2016 and 2017, insurers had insufficient data from relevant stakeholders
(in particular, superannuation trustees) to manage consumer harm.
‘Siloed’ legal entities
278 We found that data was ‘siloed’ in a group insurance context. There are
usually three main stakeholders in group TPD claims: the superannuation
trustee, the insurer and the administrator. In some cases, the administrator is
a company related to the insurer. Each stakeholder is responsible for
different parts of the claims processes—a responsibility that varies with
different firms’ arrangements.
279 Each stakeholder collected and held data relevant to the part of the claims
process that they were responsible for. In part to protect consumer privacy,
stakeholders limit the sharing of data beyond their own entity. As a result, at
any point in time insurers had incomplete data about the progress of claims,
and therefore, an incomplete picture of their exposure to conduct risk and
potential consumer harms for those claims.
Late notification by superannuation trustees
280 The most noticeable common gap in insurers’ understanding in group claims
was the period before a claim was considered formally lodged. As discussed
in Section C, for group TPD claims the consumer’s first point of contact is
typically the superannuation trustee rather than the insurer. The trustee often
passes details of the claim to the insurer only when it considers a claim
should commence.
281 This gives rise to three issues:
(a) The duration of the claim as recorded by insurers did not take into
account this pre-claim lodgement period, which exacerbated the
inconsistency of data.
(b) Superannuation trustees had different processes around this initial claim
phase. They used different ways to capture information. Some relied on
the consumer completing a lodgement form, while others had started
exploring more efficient methods such as tele-lodgement. There were

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019
Page 80
also differences in whether medical assessment statements were
collected before claim commencement, which meant that the trustees
had different approaches to when they passed claims to insurers. As a
result, insurers received claims from different trustees at different stages
in the claims process. This further aggravated the problem of
inconsistent data.
(c) Insurers were not automatically aware of the period that had already
elapsed between the consumer’s initial contact with the trustee and
when the claim was passed to them. By not having this data, insurers
were not able to identify cases where consumer harm was likely due to
delay—they were completely dependent on trustees notifying them.
Restrictive limits on personal information
282 Where superannuation trustees managed the direct relationship with
consumers, insurers often only had access to limited information about the
consumer. While we recognise the need to protect consumers’ personal
information, insurers do need access to key de-identified data to be able to
understand how groups of consumers might be experiencing harm.
Postcode information
Customer postcode and state of residence were two of the 78 data fields in
our data request. Several insurers could not provide this. We were advised
that this data was held by the superannuation trustees.
In our view, having ready access to consumer postcodes and states is
fundamental to being able to analyse claims experience and to identify
whether location is a factor in claim outcomes.
The absence of this data also meant that ASIC was unable to include
customer postcode as a factor in our statistical analysis of claims
283 For an insurer to properly handle the logistics of a specific claim it must
have regular access to all relevant data. It must ensure it has in place
arrangements with other stakeholders that, while cognisant of the need to
protect consumer privacy, facilitate ready access to the data it needs to
manage conduct risk and consumer harm.
Data quality and availability were identified as an issue by
auditors
284 We identified instances where poor claims data quality and availability had
been identified as an issue by insurers’ internal and external audit functions
during 2015 and 2016.
285 While these audit findings were largely focused on the availability of data
for actuarial and financial analysis, they do highlight awareness of the issues
we have identified. For example, in response to recommendations made by

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019
Page 81
external auditors in 2016 to take steps to resolve historical data issues that
impeded the ability to perform actuarial analysis on claims experience, TAL
noted that its ability to correct historical data deficiencies was limited
without incurring significant cost and potential reputational damage where
this involves contacting policyholders or former policyholders.
286 Internal audits for another insurer showed that a lack of data resources—and
the effect this had on the insurer’s’ ability to analyse claims experience—
was a known issue.
Finding 7: Despite recent improvements, insurers must do more to
strengthen data resources to proactively and effectively manage
consumer harm
APRA-ASIC life claims data collection and insurers’ actions
to improve data resources
287 In REP 498, we announced that we would work with APRA to develop a
consistent public reporting regime for claims outcomes and disputes. APRA
first took steps to formalise common definitions for key life insurance claims
data in November 2017. As expected, insurers found it challenging to report
all the requested data according to the specified definitions.
Note: See APRA, Update on steps to implement a public reporting regime for life
insurance claims information (PDF 560 KB), ‘Results of the phase 1, round 1 data
collection’ and ‘Attachment A: Data quality from phase 1, round 1’, November 2017.
288 In October 2018 and after extensive consultation, APRA released a reporting
standard (LRS 750
) that makes it mandatory for life insurers to provide
specific data to APRA. In March 2019, APRA published industry and
insurer level data, and ASIC published the life insurance claims comparison
tool on the
MoneySmart website.
Note: See Media Release (18-320MR) APRA and ASIC empower consumers with new
reporting standard on life insurance claims (24 October 2018) and Media Release (19-
070MR) APRA and ASIC publish world-leading life insurance data (29 March 2019).
289 Although more work is needed, insurers are now broadly complying with the
common definitions. We expect insurers to continue implementing
procedures and systems to facilitate ongoing reporting to APRA.
Note: See APRA, Letter to all life insurers and friendly societies (PDF 328 KB),
24 October 2018.
290 The FSC is also coordinating a life insurance industry data collection with an
independent firm that will collect and analyse claims and disputes data, help
insurers provide data to ASIC and APRA, and improve the industry’s data
capabilities and ability to understand and communicate its own performance. We
have expressed our support for this approach in principle. We expect the FSC to
make the data collected freely available to consumers at an aggregated insurer level.
291 We recognise that many insurers—as a result of this work by ASIC, APRA
and the FSC—have improved their data capabilities.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019
Page 82
Additional searchable data to manage consumer harm
292 Despite these developments, insurers still have considerable work to do to
ensure that their data allows them to properly manage their exposure to
consumer harm.
293 We are particularly concerned that a lack of searchable data fields prevents
insurers from having timely access to data to proactively identify the
potential for poor conduct before it occurs.
294 Table 14 summarises the types of data that some, and in a few cases, all,
insurers did not collect during 2016 and 2017 in a searchable format. We
consider that all insurers should have access to this data to proactively
manage consumer harm. For relevant products, we consider that insurers will
also need this data to meet the issuer’s design and distribution obligations to
issue an appropriate target market determination.
Table 14: Data needed to manage consumer harm
Type of data
Description
Data for analysis at a
policy level
Insurers need to collect data that enables analysis of each individual policy offered
(including where there are multiple covers in one policy), not merely data
aggregated at an insurer level.
As discussed in Section C
, claims acceptance rates for ADL definitions at a policy
level are markedly different to claims acceptance rates at an insurer level.
Value measures for
each TPD definition
We consider that insurers need to:
as an industry—develop and consult with ASIC on a set of consistently defined
measures to assess the value of products to consumers or groups of consumers
(value measures); and
collect these value measures at the level of granularity required to allow
assessment of the value of each of the various limbs of the TPD definition.
Insurers also need to have access to data on the premiums paid by consumers who
have made claims under each TPD definition, down to the level of claims lodged,
withdrawn, declined or accepted.
Group data from
superannuation
trustees and
intermediaries (e.g.
administrators)
Insurers need access to enough pre-lodgement information about a claim to allow
them to proactively and independently identify examples of consumer harm. This
includes:
the length of time from initial contact to the claim being passed on to the insurer;
the number of times the superannuation trustee has had direct contact with the
consumer (and details of those interactions);
the number of times the consumer has had to resubmit information (and details of
what they needed to resubmit); and
details of any complaints the consumer has made.
Insurers (and trustees) should also collect and keep data on the number of members
who change the default cover provided by group policies they underwrite.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019
Page 83
Type of data
Description
Claims experience of
consumers assessed
under each TPD
definition
As discussed in Section B, insurers need to have timely access to the following
details for each TPD definition in the products they underwrite:
claims lodged, withdrawn, declined and accepted; and
information about consumers lodging ADL claims, including their employment
status, age, occupation and contact details.
Data for analysis of
withdrawn claims
Insurers need to collect data that enables detailed analysis of withdrawn claims
experience at both an individual claims level and a portfolio level. For example,
insurers should be able to identify trends on when in a claims process (e.g. days
since claim lodged) and where in a claims process (e.g. straight after a third request
for a consumer to attend an IME) claims are being withdrawn. They also should be
able to analyse when consumers withdraw claims because they return to work
following use of rehabilitation services provided by the insurer.
Key claim events Insurers need to consistently capture in searchable form:
dates of when every IME was requested by insurers and attended by consumers;
names and profession of each independent medical examiner;
details of any contact with consumers’ medical advisers;
requests for consumers to complete a daily activity diary and any feedback
consumers provide, particularly any suggestion that completion of a diary is or
may cause or aggravate a mental health condition;
use of desktop surveillance and ‘factual interviews’ (in addition to physical
surveillance which most insurers already capture);
requests for all information to support a claim including requests for consumers’
full medical history;
whether the consumer was referred by the insurer to rehabilitation (provided by
either the insurer or an external third party);
whether the insurer determined the claim should be declined on the basis of non-
disclosure of a pre-existing medical condition;
who reviewed and made the final decision on any complaints made about the
claim; and
requests for assessment under urgent financial need (as required under Sections
8.27 to 8.30 of the Life Code).
Involvement of advisers
in claims process
Insurers need to capture when they first become aware that a consumer has
engaged an adviser, in relation to when the claim was opened and other key
milestones. For example, insurers should be able to identify if many consumers are
engaging advisers before lodgement of a claim or immediately after being asked to
attend an IME.
Insurers should also be able to distinguish between the different types of advisers
consumers engage.
Involvement of
reinsurers
Insurers need to develop a consistent approach to capturing when reinsurers
become involved in a claim, and the effect of that involvement on claim outcomes.
Primary and secondary
cause(s) of claims
Insurers need a consistent approach to capturing the cause(s) of a claim (e.g. injury
or illness) as well as the secondary cause(s). We understand that the FSC is
working to collect this data.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019
Page 84
Type of data
Description
Data about workforce Insurers need to develop and capture a consistent definition of several key
performance metrics for claims staff, including:
claims staff turnover; and
caseload per claims staff member.
Data for behavioural
analysis of claims staff
Insurers need to collect data to proactively identify the staff that are more likely to
give rise to conduct risk and consumer harm. This sort of analysis could be based
on work done by trading firms to identify staff who are more likely to be ‘rogue
traders’. The types of data needed would include staff performance ratings, staff
engagement and enablement feedback, claim decisions and frequent practices.
Further action
Strengthening ASIC’s powers
295 As highlighted in paragraph 77, our ability to intervene in issues of data
resources and consumer harm is complicated by exemptions for APRA-
regulated insurers from the requirements to have:
(a) adequate resources including technical and human resources (see
s912A(4) of the Corporations Act); and
(b) adequate risk management systems (see s912A(5)).
296 These exemptions prevent ASIC from:
(a) setting regulatory guidance on our minimum expectations of insurers
and superannuation trustees in relation to their data resourcing and IT
systems capabilities;
(b) directly taking action for poor data and/or IT systems; and
(c) directly taking action to ensure that the conduct risk behind the poor
conduct that gives rise to consumer harm is properly managed.
297 Only APRA can undertake these actions at present. Consistent with our
submission in response to Round 6 of the Royal Commission, ASIC
recommends that these exemptions are removed by the Government, so that
ASIC can deliver on its role as the conduct regulator for financial services.
Note: See Submissions of the Australian Securities and Investment Commission
Round 6: Insurance at paragraphs 181–185.
What we expect of industry
298 Table 15 summarises our expectations based on Findings 6 and 7 of our
review.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019
Page 85
Table 15: ASIC’s expectations
What we expect
What industry should do
Invest in data resources
and improve the quality of
data
The poor state of life insurers’ data capabilities which we identified is arguably the consequence of a failure to invest in data and associated
systems. APRA has for some time publicly expressed concern about underinvestment in systems and data capabilities and the associated
increased operational risk. ASIC is also aware of suggestions that insurers cannot comprehensively fix these issues until a new legal mechanism
is introduced to help rationalise legacy products in the life insurance and managed investment sectors.
Note: See APRA, Submission: Parliamentary Joint Committee on Corporations and Financial Services—Inquiry into the life insurance industry, November 2016,
p. 23 and FSC, 2019–20 Federal Budget: Submission to Treasury (PDF 1.9 MB), pp. 9–10.
We do not accept that resolving the legacy data issues depends on a product rationalisation mechanism. We expect insurers to keep their
systems and data resources at a sufficient standard to manage consumer harm. We note that the lack of a product rationalisation mechanism did
not prevent one insurer from making the considerable investment in data resources and associated systems referred to in paragraph 37.
Work with APRA and ASIC
to improve industry data
resources
ASIC will work with APRA, insurers and stakeholders to improve insurers’ data resources.
This will include using the types of data fields identified in Table 14 as the basis for confirming the data capabilities that insurers need to have in
order to capture, store and retrieve data and information that is necessary to adequately manage conduct risk and consumer harm.
Once confirmed, we expect insurers to provide us with plans and timeframes for developing those data capabilities. We also expect that insurers
will collect data that enables analysis of each individual policy offered (including where there are multiple covers in one policy), not merely data
aggregated at an insurer level.
We will also work with APRA to improve the public reporting regime for claims data and outcomes including considering expanding its scope
beyond claims into underwriting and other non-claims areas.
ASIC will consider publicly reporting on insurers’ responses to this expectation. Using our regulatory powers, we will also act when insurers fail to
provide timely and accurate responses to our data requests under statutory notice.
Improve industry’s data
capabilities and
consistency
Insurers should continue to work with APRA and ASIC on the industry-wide data collection. Insurers should also continue to work with the FSC
and superannuation trustees to bolster the industry’s data capabilities and standardise key data definitions.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 86
E Declined claims: Findings and outliers
Key points
We statistically analysed claims data to identify different categories of
factors that are significant in determining whether a TPD claim is declined
or admitted. This allowed us to compare the declined rates within those
factors—at both the industry-wide and the insurer levels.
We found that different categories of factors such as TPD definition, the
consumer’s age, occupation and underlying medical condition have
significantly different likelihoods of a claim being declined. We are
concerned that this may be unfairly affecting certain groups of consumers.
At a minimum, it suggests that certain groups of consumers may have
cover that is not suitable for them.
We found that the average declined claim rate for claims that went to a final
decision was 13.7%. Asteron (28.6%) and Westpac (27.6%) had the
highest declined claim rates. We also found that AMP, Asteron and
Westpac had declined more claims than our analysis predicted they would.
We will report publicly on insurers’ responses to this analysis. We will work
with AMP, Asteron and Westpac to understand the reasons why their
declined claim rates were higher than predicted and to address any
associated consumer harm.
299 In REP 498 we undertook to examine the reasons why some insurers had
declined claim rates that were substantially higher than the average rate and
to consider regulatory options where these reasons could not be justified.
300 Of the 35,026 claims in our review, 24,773 were finalised, 4,365 were
withdrawn, 5,888 remained undetermined at the end of the period, and 3,400
(13.7%) were declined.
301 The data we collected allowed us to analyse the declined rates for the
following 10 factors:
(a) the type of definition the claims were assessed under (i.e. ADL, ‘any
occupation’ and ‘own occupation’);
(b) the age of the consumer making the claim;
(c) the primary medical condition giving rise to the claim;
(d) whether the claim was formally underwritten and tailored in some way
to the consumer;
(e) the type of policy the claim was made on (i.e. a group policy, a retail
policy or a direct policy);
(f) the gender of the consumer making the claim;
(g) the amount the consumer was insured for under the policy;
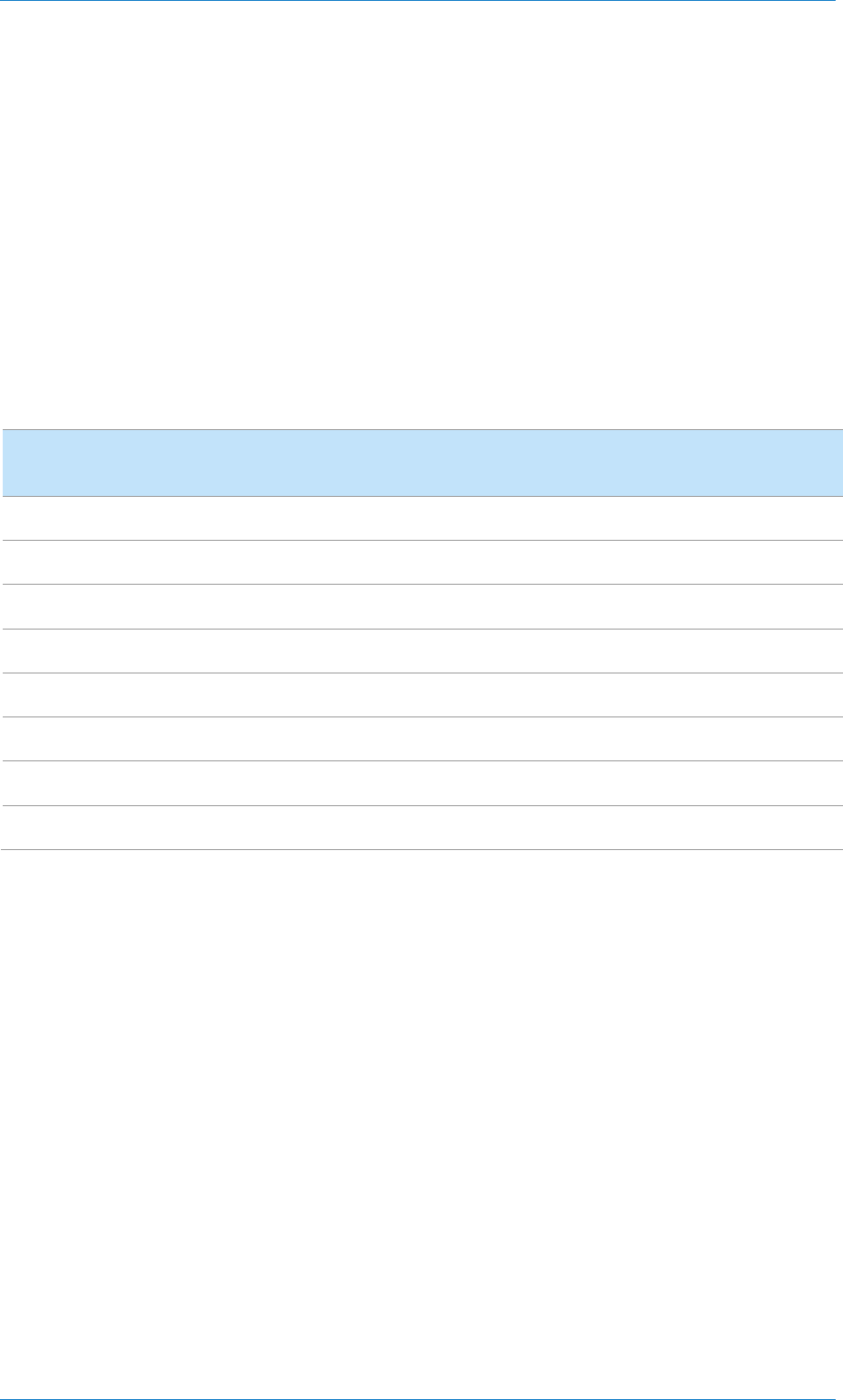
REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 87
(h) the delay between the date the claim was made and the date that the
consumer became aware of the primary condition that the claim was
based on;
(i) the length of time the policy had been in effect when the claim was
made; and
(j) whether the consumer making the claim had a white-collar or blue-
collar occupation.
302 A summary of outcomes for TPD claims received by channel across the
seven insurers during the period of our review is provided in Table 16.
Table 16: Outcomes for TPD claims, by channel (1 January 2016 to 31 December 2017)
Outcome Claims—retail Claims—direct Claims—group Claims—total
Received (number)
3,261
115
31,650
35,026
Accepted (number)
1,534
48
19,791
21,373
Declined (number)
265
14
3,121
3,400
Withdrawn (number)
696
27
3,642
4,365
Undetermined (number)
766
26
5,096
5,888
Accepted (percentage)
85%
77%
86%
86%
Declined (percentage)
15%
23%
14%
14%
Withdrawn (percentage)
21%
23%
12%
12%
Source: ASIC data collection
Note: Received claims are defined to be all claims that were reported during the period or remained undetermined at the start of
the period. Withdrawn rates have been calculated as a percentage of the total received claims.
303 Our analysis allowed us to predict and compare the different declined claim
rates within those factors—both at the industry-wide level and between
insurers—for claims that went to a final decision. To our knowledge, this is
the first time this sort of analysis has been conducted across an insurance
market in Australia.
304 This statistical analysis was reviewed by Finity Consulting Pty Ltd and
confirmed as appropriate.
Note: For more information on our analysis, including the methodology used and the
limitations, see Appendix 1 of this report.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 88
Industry-wide findings on key factors
Finding 8: Different factors, such as the TPD definition, the consumer’s
age and the underlying TPD condition, have significantly different
likelihoods of a claim being declined—unfairly affecting some consumers
305 This finding raises questions of fairness—particularly for consumers who are
paying for insurance by default through their superannuation. Some groups
of consumers are less likely than others to be able to successfully make a
claim on a TPD policy. At a minimum this indicates that some consumers
are paying for cover they may not be able to claim on. For these groups of
consumers, TPD cover may be of limited value. This suggests possible
issues with product design and claims handling processes.
306 Statistical modelling of the data for claims that went to a final decision
enables us to test whether various individual factors are statistically
significant to the probability of claims being declined. We can then estimate
the underlying probability of a particular claim being declined, controlling
for those factors particular to the claim that have been identified as
statistically significant.
307 Comparing the predicted rates between each level of the factors allows a
more accurate comparison of the relative differences than comparing the
actual rates.
Declined rates by TPD definition
308 As Table 17 shows, declined claim rates vary greatly among TPD
definitions. Almost 60% of claims assessed under the ‘activities of daily
living/working’ (ADL/ADW) definition were declined, while less than 12%
of claims assessed under ‘any occupation’ definitions were declined.
309 Most claims with an ‘unknown’ TPD definition were declined because the
consumer was not eligible to make a claim (e.g. they might not have been
insured at the time the underlying TPD condition arose). These claims are
declined before the definition is considered by the insurer.
Table 17: Declined claim rates, by TPD definition (2016–17)
TPD definition Number of
claims finalised
Actual
percentage of
finalised claims
declined
ASIC’s predicted
percentage of
finalised claims
declined
ADL/ADW
737
59.8%
60.4%
Any occupation
22,468
11.9%
12.1%
Other
174
21.3%
22.8%

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 89
TPD definition Number of
claims finalised
Actual
percentage of
finalised claims
declined
ASIC’s predicted
percentage of
finalised claims
declined
Own occupation
1,336
14.3%
14.5%
Unknown
58
96.6%
97.6%
Declined rates by underlying TPD condition
310 As Table 18 shows, consumers with an underlying ‘disease’ condition (e.g.
cancer) experienced a much lower declined rate than consumers with other
underlying conditions. Mental health claims had the highest declined rate,
with just under 17% of all mental health claims being declined.
Note: Data on secondary conditions was often missing from the data provided to us, or
we considered the data to be unreliable and therefore we did not consider it in our
analysis.
Table 18: Declined claim rates, by underlying TPD condition (2016–17)
Underlying
medical condition
Number of
claims finalised
Actual
percentage of
finalised claims
declined
ASIC’s predicted
percentage of
finalised claims
declined
Disease
7,896
9.7%
10.5%
Injury or fracture
3,570
16.1%
15.9%
Mental illness
4,839
16.9%
17.4%
Musculoskeletal
7,618
14.7%
14.8%
Other
736
13.9%
10.6%
Unknown
114
15.8%
12.2%
Declined rates by whether policy individually underwritten
311 As Table 19 shows, consumers who claimed under a policy that was
‘underwritten’ (i.e. tailored to the consumer’s individual circumstances and
taking into account their individual risk factors) had a higher declined rate
than consumers who claimed under generic, non-tailored policies such as
those provided by default through superannuation.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 90
Table 19: Declined claim rates, by whether policy individually
underwritten (2016–17)
Underwriting
status
Number of
claims finalised
Actual
percentage of
finalised claims
declined
ASIC’s predicted
percentage of
finalised claims
declined
No individual
underwriting
20,096 13.6% 13.8%
Individually
underwritten (to
some degree)
1,637 17.4% 17.9%
Unknown
3,040
12.4%
12.7%
Declined rates by distribution channel
312 Most claims are under group insurance, which is usually provided without
personal advice on a default basis through superannuation. In some cases, it
is possible to vary the terms of group insurance policies to better meet the
personal circumstances of a consumer. This explains the slight differences
between the number of group insurance claims finalised and the number of
‘no individual underwriting’ claims finalised.
313 As Table 20 shows, group insurance claims had a lower declined rate than
claims on retail policies sold to consumers through a financial adviser.
Claims made on policies sold direct (with no advice or only general advice)
had a higher declined rate than either group or retail policies. However, there
were only 62 claims finalised for the direct channel in the period.
Note: As discussed in paragraphs 169–176, superannuation trustees and financial
advisers play a role in the claim lodgement process when their members or clients
notify them of an intention to make a claim. Invariably some potential claims will not
be lodged—for example, after the trustee or adviser notifies the member or client that
they are not eligible to make a claim. Our analysis does not consider these pre-
lodgement factors. See paragraph 355 in Appendix 1 for details.
Table 20: Declined claim rates, by distribution channel (2016–17)
Distribution
channel
Number of
claims finalised
Actual
percentage of
finalised claims
declined
ASIC’s predicted
percentage of
finalised claims
declined
Group policies
22,927
13.6%
13.8%
Retail policies
1,784
14.5%
15.7%
Direct policies
62
22.6%
19.4%

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 91
Declined rates by gender
314 There was relatively little difference between the declined claim rates for
finalised claims by males (13.5%) and females (14.0%).
Declined rates by age
315 The average age of consumers who had a claim that was finalised during the
period of the review was 48 years. As Figure 9 shows, declined claim rates
decreased as consumer age increased. This may be because it can be more
difficult to prove that a younger person will never be able to work again than
an older person.
Figure 9: Declined claim rates for claims that went to a final decision, by age range (2016–17)
Source: ASIC data collection
Note: See Table 29 in Appendix 2 for the underlying data shown in this figure (accessible version).
Declined rates by age of policy
316 The ‘policy age’ is the age of the policy from the date it was entered into to
the date when the claim event occurred. The average policy age of all
policies that consumers lodged a claim on was 2,993 days—just over eight
years and two months.
317 As Figure 10 shows, the older a policy, the lower the declined rate. This is
consistent with the finding that the older the consumer making the claim, the
0
500
1,000
1,500
2,000
2,500
3,000
3,500
4,000
4,500
5,000
0%
5%
10%
15%
20%
25%
30%
35%
16–20
21–25
26–30
31–35
36–40
41–45
46–50
51–55
56–60
61–65
Number of claims finalised
Percentage of claims declined
Age range (years)
Number of claims
Declined claim rate

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 92
lower the declined rate. We would expect some correlation between policies
with a higher ‘policy age’ and older consumers.
318 There are also other reasons. One insurer noted when submitting its data:
The longer a policy is in force, generally the lower the decline[d] rate. This
relates to a reduced chance of non-disclosure through underwriting, and a
reduced impact of product conditions on the claim outcome.
Figure 10: Declined claim rates for claims that went to a final decision, by age of policy (2016–17)
Source: ASIC data collection
Note: See Table 30 in Appendix 2 for the underlying data shown in this figure (accessible version).
Declined rates by reporting delay
319 As Figure 11 shows, claims that were reported more than 1,000 days after
the claim event were declined at a higher rate (17.4%) compared to claims
reported in less than 1,000 days (12.4%). We are concerned that there may
0
500
1,000
1,500
2,000
2,500
3,000
3,500
0%
5%
10%
15%
20%
25%
Less than 100
101–200
201–300
301–400
401–500
501–600
601–700
701–800
801–900
901–1,000
1,001–2,000
2,001–3,000
3,001–4,000
4,001–5,000
5,001–6,000
6,001
–7,000
7,001
–8,000
8,001–9,000
9,001–1,0000
Greater than 10,000
Number of claims finalised
Percentage of claims declined
Age of policy (days)
Number of claims
Declined claim rate

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 93
be a correlation between this difference and claims made on group insurance
policies where the insurer on risk is no longer the current insurer for the
superannuation fund. We expect insurers and superannuation trustees to
monitor this issue closely.
320 Claims are often reported to the insurer long before a claimant’s TPD
condition is diagnosed (the ‘claim event date’). This means that there are
claims with a ‘negative’ reporting delay. Figure 11 also shows that five
claims were reported more than 1,000 days before the claim event date.
These claims were all admitted.
Figure 11: Declined claim rates for claims that went to a final decision, by reporting delay
(2016–17)
Source: ASIC data collection
Note: See Table 31 in Appendix 2 for the underlying data shown in this figure (accessible version).
Declined rates by occupation
321 There were over 3,200 different occupations listed in the data provided by
insurers. We manually classified these as either ‘blue collar’ or ‘white collar’
based on the occupation description. For 1,830 claims, the occupation was
missing or unknown.
322 Table 21 shows that declined claim rates for blue-collar occupations were
slightly lower than the rates for white-collar occupations.
0
500
1,000
1,500
2,000
2,500
0%
5%
10%
15%
20%
25%
30%
Less than -1,000
-1,000 to -200
-200 to 0
0–100
101–200
201–300
301–400
401–500
501–600
601–700
701–800
801–900
901–1,000
1,001–1,100
1,101–1,200
1,201–1,300
1,301–1,400
1,401–1,500
1,501–1,600
1,601–2,000
2,001–2,500
2,501–3,000
3,001–4,000
4,001–5,000
More than 5,000
Number of claims finalised
Percentage of claims declined
Reporting delay (days)
Number of claims
Declined claim rate

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 94
Table 21: Declined claim rates, by occupation class (2016–17)
Occupation class Number of
claims finalised
Actual
percentage of
finalised claims
declined
ASIC’s predicted
percentage of
finalised claims
declined
Blue collar
8,963
13.0%
13.0%
White collar
13,980
14.0%
14.2%
Unknown
1,830
15.3%
16.0%
Source: ASIC data collection
Findings on insurer-declined claim rates
323 We analysed the data to identify which consumers had significantly higher
rates of declined claims, both at an overall insurer level and for particular
types of claims. We found that two insurers, Asteron and Westpac, had
declined rates above 25%. We also found that those two insurers had
significantly higher declined rates than our analysis predicted—the decline
rate for Asteron was almost double the rate our analysis predicted. AMP also
declined more claims than our analysis predicted.
324 These findings raise significant concerns. We will engage with these insurers
to understand the reasons for these findings and will consider further
regulatory action if required.
Declined claim rates by insurer
Finding 9: TPD declined claim rates varied significantly between
individual insurers
325 As Table 22 shows, the overall declined claim rates varied significantly
among insurers. Asteron and Westpac had the highest declined rates at
28.6% and 27.6% respectively. On their face, we consider that these declined
rates are of concern. The average declined rate for all claims finalised in the
period was 13.7%.
Table 22: Declined claim rates, by insurer (2016–17)
Insurer Number of
claims finalised
Actual
percentage of
finalised claims
declined
ASIC’s predicted
percentage of
finalised claims
declined
AIA
7,013
16.1%
16.1%

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 95
Insurer Number of
claims finalised
Actual
percentage of
finalised claims
declined
ASIC’s predicted
percentage of
finalised claims
declined
AMP
2,900
15.1%
12.1%
MLC
2,099
18.3%
23.5%
MetLife
2,988
12.4%
12.6%
Asteron
796
28.6%
16.0%
TAL
8,622
8.7%
10.6%
Westpac
355
27.6%
18.0%
Source: ASIC data collection
Statistical analysis of predicted declined claim rates for
claims that went to a final decision
Finding 10: AMP, Asteron and Westpac had higher than predicted
declined rates for claims with certain characteristics
326 The overall declined claim rates vary greatly among insurers. Many of the
differences are because of the mix of consumer cohorts who hold the
insurers’ policies. Different proportions of claims among insurers by factors
such as TPD definition type, underlying condition, gender and age of the
consumer, distribution channel, underwriting status, and advice type—all
contribute to different declined claim rates.
327 The granularity of the data we obtained enabled us to use statistical analysis
to estimate the underlying probability of claims being declined or admitted
by each insurer, controlling for the insurers’ mix of claims based on the 10
claim factors we collected. We then compared the (actual) declined claim
rate for each insurer with what our analysis predicted the rate to be based on
the claim characteristics.
328 For example, the declined rate for claims with an underlying condition of
‘disease’ is 9% while the declined rate for claims with an underlying
condition of ‘mental health’ is 17%. Therefore, we expect that an insurer
with a high proportion of disease-based claims would have a lower declined
rate than an insurer with a high proportion of mental health claims.
329 The predicted declined rates in Table 22 show how different claim mixes can
affect declined rates. Based on MLC’s claim mix, our analysis predicted
MLC to have a declined rate of 23.5%. MLC’s actual declined rate was
lower, at 18.3%.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 96
330 TAL also had a declined rate that was lower than predicted, while AIA and
MetLife were in line with what our analysis predicted.
331 AMP, Asteron and Westpac all had declined rates higher than our analysis
predicted based on their mix of claims. The declined claim rate for Asteron
was almost double what our analysis predicted.
332 We may undertake targeted surveillance work to examine the reasons for
these higher than predicted decline rates and any associated consumer harm.
Further action
333 Table 23 summarises our expectations based on Findings 8 to 10 of our
review.
Table 23: ASIC’s expectations
What we expect
What industry should do
Review claims handling
practices and decisions
in light of industry-wide
findings
All insurers should:
undertake a review of their claims handling practices in light of the industry-wide
findings and confirm that those practices are fair and appropriate. In particular,
the reviews should focus on the factors where we found high industry-wide
declined rates and assess how insurers assess claims with those factors; and
undertake a review of a statistically significant sample of declined claims
between 1 January 2016 and 31 December 2018 with the following claims
characteristics:
− claims that were reported more than 1,000 days after the claim event;
− claims made on group policies that the insurer no longer underwrites (i.e.
legacy policies where the superannuation trustee has since changed insurer);
− mental illness claims made by consumers under the age of 30 at the time of
the claim event.
We may ask certain insurers selected
at our discretion report to us on the outcomes of
their reviews,
using our compulsory notice powers if necessary. We may also examine
any steps taken by insurers to address the findings of the reviews. We will consider
reporting publicly on insurers’ response to these expectations.
AMP, Asteron and
Westpac
We may undertake targeted surveillance work to examine the reasons for AMP,
Asteron and Westpac’s higher than predicted decline rates and to address any
associated consumer harm.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 97
Appendix 1: Methodology
334 During 2017 to 2019 we conducted a multi-staged review of TPD insurance
claims. The review covered conduct from 1 January 2016 to 31 December 2017.
Note: We undertook to do this work when we released REP 498. See REP 498, Table 7,
pp. 98–9.
335 We focused on identifying four important problems related to the concerns
identified in REP 498
, and on developing solutions to fix them. There are
other problems associated with TPD insurance, including the role of
rehabilitation providers and the difficulty of comparing TPD definitions in
the context of insurance in superannuation. But we consider that these four
problems create poor consumer outcomes and are connected to our
undertaking in REP 498 to review TPD claims files and systems.
336 The four important problems we identified were:
(a) poor consumer outcomes from insurers selling policies that provide
restrictive cover under the ADL test;
(b) frictions in claims handling processes leading to withdrawn claims;
(c) consumer harm arising from poor data; and
(d) higher than predicted declined claim rates for certain types of claims.
Our approach
337 The following insurers were included in our review:
(a) AIA;
(b) AMP and The National Mutual Life Association of Australasia Limited
(part of the AMP Group of companies);
(c) Asteron (previously Suncorp Life & Superannuation Limited);
(d) MetLife;
(e) MLC;
(f) TAL; and
(g) Westpac.
No
te: On 28 February 2019, Suncorp announced the completion of the sale of its life
insurance business to Japanese insurer Dai-ichi Life Holdings, which also owns TAL.
See Suncorp, Completion of Australian life business sale (PDF 22 KB), ASX
announcement, 28 February 2019.
338 In selecting these firms, the size of the insurer’s life insurance business
relative to its total market size was one relevant factor. We also wanted to
review a cross-section of conduct by insurers owned by banks, and by
insurers owned by overseas companies.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 98
339 These insurers represent 65–70% of the total number of TPD claims finalised or
withdrawn between 1 January 2016 and 31 December 2017 (35,026 claims in
total). The comparative cross-section of insurers included a spread across the
three sales distribution channels: group, retail and non-advised.
Stakeholder consultation
340 We consulted with key stakeholders in the life insurance industry. In
addition to the participating insurers, we held around 40 formal meetings
with external stakeholders including:
(a) superannuation trustees;
(b) reinsurers;
(c) other regulators such as APRA; and
(d) the legal community, consumer advocates and academics.
341 We used this consultation to refine our understanding of the four problems
we were seeking to address. We obtained different perspectives about the
factors affecting the offering of TPD cover, including:
(a) challenges to long-term industry profitability and sustainability;
(b) past practices that had contributed to high rates of declined claims and
long claim durations;
(c) the role of reinsurers;
(d) the role of superannuation trustees;
(e) the consumer experience in making a TPD claim;
(f) frictions in claims handling;
(g) the future of product design; and
(h) the potential advantages of standard cover definitions.
Data collection
342 The insurers were asked to provide data on each of 35,026 TPD claims that were
reported, finalised or withdrawn between 1 January 2016 and 31 December 2017.
For each claim, we requested 78 individual data points, which related to:
(a) insurance type, advice type, and associated superannuation trustees;
(b) key dates such as policy inception, claim notification, decision, and
claim duration;
(c) benefit payments, waiting periods, sum insured and underwriting status;
(d) claim outcomes (accepted, declined or withdrawn claims, and ex gratia
payments);

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 99
(e) assessment practices used (e.g. surveillance or referral to an
independent medical examiner); and
(f) disputes, including whether the consumer had legal representation.
343 To ensure that each insurer could respond to our data request, we discussed
the type of data stored and its accessibility and tested draft data requests for
feedback. Although each insurer received the same request, we worked with
insurers where some data was unavailable or available in a different form.
344 When ASIC conducted a final accuracy review before publishing this report,
errors in the data provided by two of the insurers were identified. For a range
of reasons, including materiality, this data has not been changed in this
report and does not change the findings or recommendations.
Statistical analysis of declined claim data
345 The granularity and depth of information we collected enabled us to perform
in depth analysis of TPD claims that to our knowledge has never been
performed before in Australia.
346 Statistical modelling of the data enables us to estimate the underlying
probability of each claim being declined, controlling for all the individual
factors particular to each claim.
347 The overall declined rates of the seven insurers varied greatly; however, a lot of
the differences are because of the different mix of consumers, from different
occupations and ages for each insurer. Different proportions of claims by
assessment types, underlying conditions, distribution channels, underwriting
types, advice types also contribute to the different decline rates observed.
348 Analysis was performed to determine which factors are significant in
whether a TPD claim is declined or admitted.
349 ASIC’s methodology, analysis and statistical results were reviewed by Finity
Consulting Pty Ltd and confirmed as sound and appropriate.
350 The following 10 factors were analysed to test if they were statistically significant:
(a) the type of definition the claims were assessed under (i.e. ADL, ‘any
occupation’ and ‘own occupation’) (claim assessment);
(b) the age of the consumer making the claim (age of claimant);
(c) the primary medical condition giving rise to the claim (primary condition);
(d) whether the claim was formally underwritten and tailored in some way
to the consumer (underwriting);
(e) the type of policy the claim was made on (i.e. group policy, a retail
policy or a direct policy) (insurance type / advice);

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 100
(f) the gender of the consumer making the claim (gender);
(g) the amount the consumer was insured for under the policy (sum insured);
(h) the delay between the date the claim was made and the date that the
consumer became aware of the primary condition that the claim was
based on (reporting delay);
(i) the length of time the policy had been in effect when the claim was
made (policy age); and
(j) whether the consumer making the claim had a white-collar or blue-
collar occupation (occupation class).
351 There were a number of factors in the data that were not considered in the
analysis. The following were not considered, as claims that are inherently
more difficult to determine, and hence more likely to be declined, have a
much higher incidence of having these parties involved in the claim process:
(a) the involvement of legal representatives;
(b) whether surveillance was used by the insurer;
(c) whether the insurer referred the claim to its chief medical officer to review;
(d) whether the insurer referred the claim to an independent medical
examiner; and
(e) whether a reinsurer was involved in handling the claim.
352 State and postcode were also not considered in the model. This was because
for a large proportion of group claims the address provided by the insurer
was that of the superannuation trustee and not the claimant.
353 Secondary condition was also not considered, as anecdotal evidence suggests
records of secondary conditions are very poor and unreliable.
354 Our analysis identified that the following factors are statistically significant.
In order of significance, they are:
(a) assessment type;
(b) age;
(c) policy age;
(d) primary condition;
(e) reporting delay;
(f) underwriting; and
(g) occupation class.
Limitations
355 Because a statistical model is a simplification of reality, there is uncertainty
in the results of the analysis, which can manifest from several sources:
(a) This analysis is based on claims data from seven insurers only.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 101
(b) The analysis relies on the data provided by the insurers under statutory
notice—different interpretations, definitions, processes and quality can
result in inconsistent data between the insurers.
(c) The model is limited to the data points collected. Other characteristics
of claims could be significant in determining the outcomes of claims.
These factors were not able to be analysed because they were:
(i) not recorded by insurers;
(i) not able to be collected in a format required for analysis; or
(ii) other external factors not considered for this analysis.
(d) The analysis is based on historical data and makes no allowance for
changes in insurers’ processes since the reporting period or trends in
overall claims experience.
(e) Superannuation trustees have different processes for submission of
claims. This can result in claims submitted initially to some trustees not
even reaching the insurer as they are deemed unlikely to be successful
before a claim is lodged with the insurer.
(f) Retail advisers may provide consumers with advice when they notify
their adviser of an intention to make a claim. This can result in potential
claims not reaching the insurer after the adviser informs the consumer
that they are unlikely to be successful.
Qualitative review
356 We asked each insurer to provide us with an outline of their processes in a
qualitative survey that contained 49 main questions, using our compulsory
information-gathering powers.
357 We also obtained and reviewed more than 2,400 documents from the seven
participating insurers using our compulsory information-gathering powers.
The documents related to the insurers’ processes, including:
(a) TPD claims handling policies and procedures;
(b) product design strategies, processes and business cases;
(c) arrangements between insurers and third parties (e.g. reinsurers and
superannuation trustees);
(d) quality assurance review processes and reports;
(e) targets, incentives and performance management frameworks; and
(f) the structure of claims and dispute systems used by insurers.
358 The primary purpose of this work was to understand the insurers’ processes that
were relevant to the four problems we focused on. We also looked at insurers’
practices that have contributed to, or failed to mitigate, very poor outcomes.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 102
Consumer research
359 We commissioned an independent market research firm, Newgate Research,
to conduct qualitative research with 20 consumers who made a TPD claim
with one of the insurers in our review.
360 To source participants for this research, we obtained contact lists from each of
the insurers in our review using our compulsory information-gathering powers.
We contacted a sample of consumers from these lists and asked whether they
would participate in the research and give consent for their contact details to be
passed to the consumer researcher. Newgate then contacted the consumers and
re-established their willingness to be interviewed.
361 The research aimed to:
(a) explore the consumer journey and experience of the claims process;
(b) analyse interactions and communications between consumers, insurers
and/or superannuation trustees, and other third parties who help in the
claims process;
(c) identify key decision points for consumers; and
(d) provide recommendations for how to improve the claims process.
362 The research involved one-to-one interviews with the consumers. Interviews
lasted up to 90 minutes and were, usually, conducted in the consumer’s
home or over the phone, between November 2018 and January 2019.
363 There are limitations to this kind of research. Our research was qualitative in
nature. This provides in-depth understanding of the motivations, behaviours
and knowledge of consumers. Due to the small sample sizes, qualitative
research cannot be generalised to the wider population; it is used for
illustrative purposes only. The research covered a larger number of declined
and withdrawn claims than was representative of all TPD claims given our
desire to develop an understanding of the drivers of withdrawn claims.
364 Consumers who participated in the research were self-selected. Others
declined to participate in the research due to fear of effects on their ongoing
claims, anxiety or simply a lack of interest. Accordingly, the sample may not
reveal the full scope of consumer experiences.
365 Some of the interviews were carried out with consumers some time after the
events in question. This means that there could be unconscious biases
present or consumers could have forgotten relevant information.
366 The names of consumers that participated in the consumer research have
been changed throughout this report as well as some specific details to help
maintain their confidentiality.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 103
Appendix 2: Accessible versions of figures
367 This appendix is for people with visual or other impairments. It provides
accessible versions of the figures included in this report.
368 We show the underlying data for each figure, where appropriate, or we may
include a text description of the figure’s key messages.
Table 24: Declined claim rates for TPD cover, by insurer (2016–17)
Insurer
Percentage of declined claims
Percentage of accepted claims
TAL
9%
91%
MetLife
12%
88%
AMP
15%
85%
AIA
16%
84%
MLC
18%
82%
Westpac
28%
72%
Asteron
29%
71%
Note 1: This table shows the data contained in Figure 2.
Note 2: Some of the difference in declined claim rates between insurers can be explained by the
relative mix of the insurers’ claims and policies, including:
• policy distribution channels: the declined claim rates for group (13.6%), retail (14.5%) and
direct (22.6%) are different (see Table 20); and
• policies open for sale and not open for sale (i.e. legacy products).
Table 25: Actual declined rates compared to ASIC-predicted declined rates
for claims that went to a final decision, by insurer (2016–17)
Insurer Actual percentage of finalised
claims declined
Predicted percentage of
finalised claims declined
AIA
16.1%
16.1%
AMP
15.1%
12.1%
Asteron
28.6%
16.0%
MLC
18.3%
23.5%
MetLife
12.4%
12.6%
TAL
8.7%
10.6%
Westpac
27.6%
18.0%
Note: This table shows the data contained in Figure 3.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 104
Table 26: Total life insurance premiums (millions of dollars), by cover
type (at 31 December 2018)
Life insurance cover type
Premium (millions)
Accident cover
$111 million
Consumer credit insurance
$322 million
Funeral cover
$478 million
Trauma cover
$1,469 million
TPD cover
$3,548 million
Income protection
$5,033 million
Death cover
$6,390 million
Note: This table shows the data contained in Figure 4.
Table 27: Total lives insured (in thousands), TPD and death cover
(at 31 December 2018)
Channel
Lives insured—TPD cover
Lives insured—Death cover
Group (outside
superannuation)
232,000 186,000
Direct
48,000
555,000
Retail (advised)
1,177,000
1,994,000
Group (in
superannuation)
11,999,000 13,299,000
Total (all channels)
13,456,000
16,034,000
Note: This table shows the data in Figure 5.
Table 28: Percentage of declined claims assessed under the ADL test
that went to a final decision, by insurer (2016–17)
Insurer
Percentage of ADL claims declined
AMP
15%
TAL
44%
Westpac
50%
All
60%
AIA
61%
MLC
70%
Asteron
79%
Note: This table shows the data in Figure 8.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 105
Table 29: Declined claim rates for claims that went to a final decision,
by age range (2016–17)
Age range of consumers Number of claims
declined
Percentage of claims
declined
16–20 years
76
21.1%
21–25 years
393
29.0%
26–30 years
1,001
22.7%
31–35 years
1,687
20.4%
36–40 years
2,475
16.8%
41–45 years
3,577
16.8%
46–50 years
4,048
14.5%
51–55 years
4,675
11.3%
56–60 years
4,118
9.1%
61–65 years
2,565
6.4%
Note: This table shows the data in Figure 9.
Table 30: Declined claim rates for claims that went to a final decision,
by age of policy (2016–17)
Age of policy Number of claims
finalised
Percentage of claims
declined
Less than 100 days
387
22.2%
101–200 days
417
20.6%
201–300 days
452
18.6%
301–400 days
477
15.7%
401–500 days
469
13.7%
501–600 days
417
11.0%
601–700 days
456
14.9%
701–800 days
442
16.1%
801–900 days
410
14.6%
901–1,000 days
392
13.3%
1,001–2,000 days
2869
12.8%

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 106
Age of policy Number of claims
finalised
Percentage of claims
declined
2,001–3,000 days
2073
9.9%
3,001–4,000 days
1773
9.6%
4,001–5,000 days
1470
7.2%
5,001–6,000 days
1053
10.2%
6,001–7,000 days
852
6.8%
7,001–8,000 days
548
9.7%
8,001–9,000 days
390
5.4%
9,001–10,000 days
200
5.5%
More than 10,000 days
215
7.4%
Note: This table shows the data in Figure 10.
Table 31: Declined claim rates for claims that went to a final decision,
by reporting delay (2016–17)
Time between loss event
and reporting date
Number of claims
finalised
Percentage of claims
declined
Less than -1,000 days
5
0.0%
-1,000 to -200 days
52
15.4%
-200 to 0 days
236
15.3%
0–100 days
2024
12.2%
101–200 days
2330
12.1%
201–300 days
2183
12.0%
301–400 days
2158
14.0%
401–500 days
1913
13.1%
501–600 days
1721
11.0%
601–700 days
1629
12.4%
701–800 days
1583
10.9%
801–900 days
1318
13.2%
901–1,000 days
1063
12.7%

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 107
Time between loss event
and reporting date
Number of claims
finalised
Percentage of claims
declined
1,001–1,100 days
849
16.7%
1,101–1,200 days
762
15.0%
1,201–1,300 days
601
11.2%
1,301–1,400 days
479
14.6%
1,401–1,500 days
468
18.0%
1,501–1,700 days
707
14.9%
1,701–2,000 days
809
17.6%
2,001–2,500 days
809
20.2%
2,501–3,000 days
434
24.4%
3,001–4,000 days
370
24.3%
4,001–5,000 days
135
17.8%
More than 5,000 days
135
26.7%
Note: This table shows the data in Figure 11.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 108
Key terms
Term
Meaning in this document
accident cover A life insurance policy that pays for medical and out-of-pocket
expenses that the policyholder may incur after an accidental injury
ADL Activities of daily living—a set of disability criteria comprising a
sub-definition of TPD under many insurance policies. Closely
related terms include ‘activities of daily working’ (ADW) and
‘everyday working activities’ (EWA)
advice provider A person to whom the obligations in Div 2 of Pt 7.7A of the
Corporations Act apply when providing personal advice to a client.
This is generally the individual who provides the personal advice.
However, if there is no individual that provides the advice, which
may be the case if advice is provided through a computer
program, the obligations in Div 2 of Pt 7.7A apply to the legal
person that provides the advice (e.g. a corporate licensee or
authorised representative)
AFS licence An Australian financial services licence under s913B of the
Corporations Act that authorises a person who carries on a
financial services business to provide financial services
AFS licensee A person who holds an AFS licence under s913B of the
Corporations Act
AIA
AIA Australia Limited
AMP
AMP Life Limited
APRA
Australian Prudential Regulation Authority
APRA-ASIC claims
data collection
Data on life insurance claims and claims-related disputes for the
period 1 January 2017 to 30 June 2017 published by APRA and
ASIC: see Media Release (18-150MR)
APRA and ASIC release
new life-claims data (24 May 2018)
ASIC Act
Australian Securities and Investments Commission Act 2001
Asteron
Asteron Life & Superannuation Limited
automatic insurance Cover provided through group insurance policies that is not
individually underwritten insurance cover
claim duration Measured as the waiting period plus the number of days between
the date the claim is finalised and the later of:
the claim reported date; and
the claim event date
common form TPD
definition
The insured becomes totally and permanently disabled and is
unable to work again (in either their own occupation or any
occupation)

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 109
Term
Meaning in this document
condition (primary) The original injury or illness which led to the claim. The categories
used in this review were:
disease;
injury or fracture;
musculoskeletal;
mental illness; and
other
condition (secondary) A subsequent injury or illness stemming from the underlying
primary condition
consumer credit
insurance
In the context of life insurance this means a type of policy that
provides a payout to meet the consumer’s liability under a credit
contract if they should die
consumer research Quantitative and qualitative research conducted by Newgate
Research for ASIC with consumers who had recently made a TPD
claim through an insurer that participated in our review
Corporations Act Corporations Act 2001, including regulations made for the
purposes of that Act
Corporations
Regulations
Corporations Regulations 2001
cross-subsidisation The practice of charging higher premiums to one group of
consumers to artificially lower premiums for another group
daily activity diary A tool intended to be used for activity monitoring during the claims
process
declined claim rate
(or declined rate)
The percentage of claims declined by an insurer out of total
claims made
direct policies A life insurance policy that is sold to consumers with general or no
advice and without a group intermediary like a superannuation
fund
disability income
insurance
Has the same meaning as income protection insurance
disability threshold
criteria
These define the conditions a person must meet to show that they
are totally and permanently disabled in accordance with the policy
ex gratia payment
A payment made on a goodwill or without liability basis
financial adviser
An advice provider
financial service
Has the meaning given in Div 4 of Pt 7.1 of the Corporations Act
FSC
Financial Services Council
general advice Financial product advice that is not personal advice
Note: This is a definition contained in s766B(4) of the Corporations Act.

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 110
Term
Meaning in this document
general obligations The obligations of an AFS licensee under s912A(1) of the
Corporations Act
GESB
Government Employees Superannuation Board
group policy A life insurance policy issued to a third party (e.g. a
superannuation trustee) that policyholders can access through
their membership of the third party’s fund
Insurance Contracts
Act
Insurance Contracts Act 1984
IME
Independent medical examination
income protection
insurance
A life insurance policy that replaces the income lost if the
policyholder is unable to work for a certain amount of time due to
injury and or sickness
Insurance in
Superannuation Code
The Insurance in Superannuation Voluntary Code of Practice—a
voluntary code of practice for the superannuation insurance
industry. The Code provides a framework to ensure that the
insurance cover that superannuation funds offer their members is
affordable and appropriate to their needs
insurer
The company that issues the life insurance policy
Life Code
The Life Insurance Code of Practice—developed by the FSC
life insurance An insurance policy that pays either a lump sum or income stream
payment in the event of death, illness or disability. Life insurance
policies can include cover for death, total and permanent
disablement, trauma and income protection
Life Insurance Act
Life Insurance Act 1995
life insurance policy
A life insurance contract as defined in s9 of the Life Insurance Act,
excluding investment or annuity-related contracts
member
(superannuation)
A member of a superannuation fund, and includes a prospective
member
mental illness A clinically diagnosable disorder that significantly interferes with
an individual’s cognitive, emotional and/or social abilities. The
diagnosis of mental illness is generally made according to the
classification systems of the Diagnostic and statistical manual of
mental disorders or the International classification of diseases and
related health problems
Note: See the definition of ‘mental illness’ in Australia’s National Mental
Health Policy 2008.
MetLife
MetLife Insurance Limited
MLC
MLC Limited
MySuper product A default superannuation product provided under Pt 2C of the SIS
Act

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 111
Term
Meaning in this document
non-advised policies Life insurance policies that are sold to consumers directly, without
an intermediary such as an adviser or superannuation fund
NULIS
NULIS Nominees (Australia) Limited
personal advice Financial product advice given or directed to a person (including
by electronic means) in circumstances where:
the person giving the advice has considered one or more of the
client’s objectives, financial situation and needs; or
a reasonable person might expect the person giving the advice
to have considered one or more of these matters
Note: This is a definition contained in s766B(3) of the Corporations Act.
pre-existing medical
condition (or pre-
existing condition)
Used in life insurance contracts, this typically means an illness,
medical condition or related symptom that:
was diagnosed or known about by the insured;
the insured had sought, or intended to seek, medical treatment
for; or
a reasonable person should have been aware of or would have
sought medical treatment for.
Definitions can vary across insurance contracts
Productivity
Commission report
Report 91, Superannuation: Assessing efficiency and
competitiveness, issued by the Productivity Commission on
21 December 2018. The Productivity Commission is the
Australian Government’s independent research and advisory body
on economic, social and environmental issues affecting the
welfare of Australians
rehabilitation Activities aimed at assisting individuals with incapacitating illness
and injuries to regain wellness
reinsurer An insurance company that insures the risks of other insurance
companies, usually based on a proportion or predetermined limit
of losses
REP 498 (for
example)
An ASIC report (in this example numbered 498)
retail policies
Life insurance policies that are sold to policyholders who have
sought financial product advice
Royal Commission The Royal Commission into Misconduct in the Banking,
Superannuation and Financial Services Industry
SIS Act Superannuation Industry (Supervision) Act 1993, including
regulations made for the purposes of that Act
SIS Regulations
Superannuation Industry (Supervision) Regulations 1994
sum insured The contractual benefit payable under the TPD policy, should the
insured event occur
Suncorp
Suncorp Life & Superannuation Limited

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 112
Term
Meaning in this document
superannuation fund
Has the meaning given in s10(1) of the SIS Act
TAL
TAL Life Limited
terminal illness cover A component of life cover that pays the lump sum benefit to the
policyholder when they are diagnosed with a terminal illness (a
further payment is not made when the policyholder dies)
TPD insurance
(cover)
A type of life insurance that pays a lump sum if the consumer
becomes totally and permanently disabled.
trustee
(superannuation)
A person or group of persons licensed by APRA under s29D of
the SIS Act to operate a registrable superannuation entity (e.g.
superannuation fund) (also known as an ‘RSE licensee’)
underwriting The process used by an insurer to decide whether or not to
accept a risk by entering into a contract of insurance, and, if the
risk is accepted, the terms and conditions to be applied and the
level of premium to be charged
universal terms The universal key definitions, terms and exclusions for default
MySuper group life policies referred to in Recommendation 4.13
of the Royal Commission. See paragraph 75, above.
waiting period A period during which the insured must be absent from work to
qualify for assessment as TPD (usually six months)
Westpac
Westpac Life Insurance Services Limited
withdrawal (active) When the consumer, their superannuation fund trustee or fund
administrator informs the insurer that the consumer will no longer
pursue the claim
withdrawal (passive) When the insurer withdraws a claim in circumstances where the
consumer has not responded to a request for information

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 113
Related information
Headnotes
Activities of daily living test, ADL, claims handling, conduct risk, consumer
harm, culture, data resources, design and distribution obligations, declined
claims, direct life insurance, DDOs, duty of utmost good faith, group
insurance, income protection, insurers, Life Code, life insurance, mental
illness, MySuper, product design, product intervention powers, Protecting
Your Super reforms, retail channel, Royal Commission, superannuation
trustees, total and permanent disability, TPD, trauma, withdrawn claims
Legislation
ASIC Act
Corporations Act, s912A(1)(d), 912A(1)(h), 912A(4), 912A(5)
Corporations Regulations, reg 7.1.33
Insurance Contracts Act
SIS Act, s52(7), 52(7)(d)
SIS Regulations, Sch 1AA
Treasury Laws Amendment (Design and Distribution Obligations and
Product Intervention Powers) Act 2019
Treasury Laws Amendment (Protecting Your Superannuation Package) Act
2019
Cases
Hellessey v MetLife Insurance Limited [2017] NSWSC 1284
Manglicmot v Commonwealth Bank Officers Superannuation Corporation
Pty Ltd [2011] NSWCA 204
MetLife Insurance Limited v Hellessey [2018] NSWCA 307
Consultation papers and reports
CP 317 Unsolicited telephone sales of direct life insurance and consumer
credit insurance
REP 498 Life insurance claims: An industry review

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 114
REP 587 The sale of direct life insurance
REP 591 Insurance in superannuation
REP 621 Roadblocks and roundabouts: A review of car insurance claim
investigations
Submissions of the Australian Securities and Investments Commission to the
Financial Services Royal Commission Round 6: Insurance
Media releases
18-150MR APRA and ASIC release new life-claims data (24 May 2018)
18-320MR APRA and ASIC empower consumers with new reporting
standard on life insurance claims (24 October 2018)
19-070MR APRA and ASIC publish world-leading life insurance data
(29 March 2019)
Other references
Actuaries Institute, Mental health and insurance (PDF 2.7 MB), green paper,
October 2017
APRA, Letter to all life insurers and friendly societies (PDF 328 KB), 24
October 2018
APRA, Life insurance claims and disputes statistics (PDF 700 KB), June
2018 (released 29 March 2019)
APRA, Life insurance claims and disputes statistics (PDF 623 KB),
December 2018 (released 27 June 2019)
APRA, Prudential Standard SPS 250 Insurance in superannuation
APRA, Quarterly life insurance performance statistics, 28 February 2019
APRA, Reporting Standard LRS 750 Claims and disputes, October 2018
APRA, Submission: Parliamentary Joint Committee on Corporations and
Financial Services—Inquiry into the life insurance industry, November 2016
APRA, Update on steps to implement a public reporting regime for life
insurance claims information (PDF 560 KB), November 2017
ASIC, ‘Lifting the bar’, Superfunds magazine, June 2019
Basel Committee on Banking Supervision, Principles for effective risk data
aggregation and risk reporting (PDF 130 KB), January 2013

REPORT 633: Holes in the safety net: A review of TPD insurance claims
© Australian Securities and Investments Commission October 2019 Page 115
Cbus, Insurance guide: Personal Super (PDF 2.5 MB), 5 October 2018
FSC, 2019–20 Federal Budget: Submission to Treasury (PDF 1.9 MB)
Life Code Compliance Committee, Life Insurance Code of Practice: Annual
industry data and compliance report 2017–18, March 2019
Local Government Super, Product Disclosure Statement: Accumulation
Scheme, 1 July 2019
Parliamentary Joint Committee on Corporations and Financial Services,
Options for greater involvement by private sector health insurers in worker
rehabilitation, report, October 2018
Productivity Commission, Superannuation: Assessing efficiency and
competitiveness, inquiry report no. 91, December 2018
Royal Commission, Final report, February 2019
Royal Commission, Round 6 hearings, 13 and 14 September 2018,
transcripts
Royal Commission, Round 6 hearings, TAL Group written submissions
Sparrow, Malcolm K, The regulatory craft: Controlling risks, solving
problems and managing compliance, Brookings Institution Press,
Washington DC, 2000
Suncorp, Completion of Australian life business sale
(PDF 22 KB), ASX
announcement, 28 February 2019
