
January 2024
4 - 1
Bloodstream Infection Event (Central Line-Associated Bloodstream
Infection and Non-central Line Associated Bloodstream Infection)
Table of Contents
Introduction ............................................................................................................................................................... 2
Settings ...................................................................................................................................................................... 2
Key Terms and Abbreviations .................................................................................................................................... 2
Definitions Specific to Bloodstream Infection (BSI) / Central Line Associated Bloodstream Infection (CLABSI)
Surveillance ............................................................................................................................................................... 3
Laboratory Confirmed Bloodstream Infection (LCBIs) Hierarchy; Types of LCBIs ..................................................... 3
Types of Central Lines for NHSN reporting purposes ................................................................................................ 5
Devices Not Considered Central Lines for NHSN Reporting Purposes ...................................................................... 6
Table 1: Laboratory-Confirmed Bloodstream Infection Criteria: .............................................................................. 6
Table 2: Mucosal Barrier Injury Laboratory-Confirmed Bloodstream Infection (MBI-LCBI) ................................... 10
Reporting Instructions: See below for a Summary of CLABSI Exclusions and Reporting Requirements. ............... 12
Reporting Instructions ............................................................................................................................................. 13
Blood Specimen Collection ...................................................................................................................................... 14
Table 3: Examples of Associating the Use of Central Lines to BSI Events (CLABSI) ................................................ 16
Pathogen Exclusions and Reporting Considerations ............................................................................................... 18
Table 4: Reporting Speciated and Unspeciated Organisms Identified from Blood Specimens ............................... 19
Table 5: Examples Illustrating the MBI-LCBI Criteria for Neutropenia .................................................................... 19
Monthly Summary Data .......................................................................................................................................... 20
Table 6: Examples of Denominator Day counts for Device Days ............................................................................ 21
Table 7: Denominator Data Collection Methods ..................................................................................................... 23
Data Analyses ................................................................................................................................................. ………26
Table 8: CLABSI Measures Available in NHSN ......................................................................................................... 29
References ............................................................................................................................................................... 30
Appendix: Secondary BSI Guide (not applicable to Ventilator-associated Events [VAE]) ....................................... 31
Table B1: Secondary BSI Guide: List of all NHSN primary site-specific definitions available for making secondary
BSI determinations using Scenario 1 or Scenario 2 ................................................................................................. 35
Secondary BSI Reporting Instructions ..................................................................................................................... 36
Pathogen Assignment .............................................................................................................................................. 38
Figure B1: Secondary BSI Guide for eligible organisms .......................................................................................... 46
Figure B2: VAE Guidance for Secondary BSI Determination .................................................................................. 47
Disclaimer: The appearance of any product or brand names in this training protocol is for educational purposes
only and is not meant to serve as an official endorsement of any such product or brand by the Centers for
Disease Control and Prevention (CDC) or the United States Government. CDC and the United States
Government, by mentioning any particular product or brand, is neither recommending that product or brand
nor recommending against the product’s or brand’s use.

January 2024 Device-associated Module
BSI
4 - 2
Bloodstream Infection Event (Central Line-Associated Bloodstream
Infection and Non-central Line Associated Bloodstream Infection)
Introduction
Although a 46% decrease in CLABSIs has occurred in hospitals across the U.S. from 2008-2013, an estimated
30,100 central line-associated bloodstream infections (CLABSI) still occur in intensive care units and wards of
U.S. acute care facilities each year.
1
CLABSIs are serious infections typically causing a prolongation of hospital
stay, increased cost, and risk of mortality.
CLABSIs can be prevented through proper insertion techniques and management of the central line which are
addressed in the CDC’s Healthcare Infection Control Practices Advisory Committee (CDC/HICPAC) Guidelines for
the Prevention of Intravascular Catheter-Related Infections, 2011.
2
Settings
Surveillance may occur in any inpatient location where denominator data can be collected, which can include
critical/intensive care units (ICU), specialty care areas (SCA), neonatal units including neonatal intensive care
units (NICUs), step down units, wards, and long-term acute care units. A complete listing of inpatient locations
and instructions for mapping can be found in the CDC Locations and Descriptions chapter.
Note: CLABSI surveillance after patient discharge from a facility is not required. However, if discovered, any
CLABSI with a date of event (DOE) on the day of or the day after discharge is attributed to the discharging
location and should be communicated to that facility to encourage appropriate NHSN reporting of CLABSIs.
(See Transfer Rule, Chapter 2). D
o not collect or report additional central line days after discharge.
Key Terms and Abbreviations
Refer to the NHSN Patient Safety Manual, Chapter 2 Identifying Healthcare Associated Infections in NHSN and
Chapter 16 NHSN Key Terms for definitions of the following universal concepts for conducting HAI surveillance.
I. Date of event (DOE)
II. Healthcare associated infection (HAI)
III. Infection window period (IWP)
IV. Present on admission (POA)
V. Repeat infection timeframe (RIT)
VI. Secondary BSI attribution period (SBAP)
VII. Location of Attribution (LOA)
VIII. Transfer rule

January 2024 Device-associated Module
BSI
4 - 3
Definitions Specific to Bloodstream Infection (BSI) / Central Line Associated
Bloodstream Infection (CLABSI) Surveillance:
Primary bloodstream infection (BSI): A Laboratory Confirmed Bloodstream Infection (LCBI) that is not secondary
to an infection at another body site (see Appendix: Secondary BSI Guide and CDC/NHSN Surveillance Definitions
for Specific Types of Infection [Ch-17], urinary tract infection (UTI) [Ch-7], pneumonia (PNEU) [Ch-6], and surgical
site infection (SSI) [Ch- 9].
Laboratory Confirmed Bloodstream Infection (LCBIs) Hierarchy; Types of LCBIs
(see Table 1 and Table 2):
Secondary BSI: A BSI that is thought to be seeded from a site-specific infection at another body site (see
Appendix: Secondary BSI Guide and CDC/NHSN Surveillance Definitions for Specific Types of Infection, UTI,
PNEU, and SSI).
Secondary BSI Attribution Period (SBAP): The period in which a blood specimen must be collected for a
secondary BSI to be attributed to a primary site of infection. This period includes the Infection Window Period
(IWP) combined with the Repeat Infection Timeframe (RIT). The SBAP is 14-17 days in length depending upon
the date of event (See Secondary BSI Attribution period, Chapter 2).
Infusion: The administration of any solution through the lumen of a catheter into a blood vessel. Infusions
include continuous infusion (for example, nutritional fluids or medications), intermittent infusion (for example,
IV flush), IV antimicrobial administration, and blood transfusion or hemodialysis treatment.
Access: The performance of any of the following activities during the current inpatient admission:
• Line placement
• Use of (entering the line with a needle or needleless device) any central line for:
o Infusion
o Withdrawal of blood
• Use for hemodynamic monitoring

January 2024 Device-associated Module
BSI
4 - 4
Notes:
1. If a patient is admitted to an inpatient location with a central line (CL) already in place, and it is the
patient’s only CL, the day of first access in an inpatient location begins the central line day count (CL Day
for making central line-associated determinations). De-accessing any type of central line (for example,
removal of port needle but port remains in body) does not remove the patient from CLABSI surveillance
or device day counts for reporting denominator summary data.
2. An inpatient location, for making determinations about central line access, includes but is not limited to,
any department or unit within the facility that provides service to inpatients [for example, inpatient
Dialysis, Operating Room (OR), Interventional Radiology, Gastroenterology Lab (GI), Cardiac
Catheterization lab (CC), wards, ICUs, etc.].
3. Include any inpatient receiving dialysis in CLABSI surveillance conducted in the patient’s assigned
inpatient location, regardless of whether the patient only has one CL and dialysis staff are the only
providers to access it during dialysis treatment.
Examples: CLABSIs in the following examples will be attributed to Unit A
• Patient on Unit A receives onsite dialysis by contracted dialysis staff
• Dialysis staff travels to Unit A to provide dialysis to an Unit A patient
• Patient in Unit A for inpatient care is transported to dialysis unit within the facility for
dialysis
Because CLABSI events cannot be attributed to a non-bedded inpatient location (inpatient
location where denominator data is not collected but inpatient care is provided, for example,
OR, IR, or inpatient dialysis), such events must be attributed to the inpatient location housing
the patient.
Central line (CL): An intravascular catheter that terminates at or close to the heart, or in one of the great vessels
AND is used for infusion, withdrawal of blood, or hemodynamic monitoring. Consider the following great
vessels when making determinations about CLABSI events and counting CL device days:
• Aorta
• Pulmonary artery
• Superior vena cava
• Inferior vena cava
• Brachiocephalic veins
• Internal jugular veins
• Subclavian veins
• External iliac veins
• Common iliac veins
• Femoral veins
• In neonates, the umbilical artery/vein.

January 2024 Device-associated Module
BSI
4 - 5
Notes:
1. Neither the type of device nor the insertion site is used to determine if a device is considered a central
line for NHSN reporting purposes.
2. At times, a CL may migrate from its original central location after confirmation of proper placement.
NHSN does not require ongoing verification of proper line placement. Therefore, once a line has been
designated a CL it remains a CL, regardless of migration, until removed from the body or patient
discharge, whichever comes first. CL days are included for any CLABSI surveillance conducted in that
location.
3. An introducer is an intravascular catheter, and depending on the location of the tip and its use, may be
considered a CL.
4. A non-lumened intravascular catheter that terminates at or close to the heart or in a great vessel that is
not used for infusion, withdrawal of blood or hemodynamic monitoring is not considered a CL for NHSN
reporting purposes (for example, non-lumened pacemaker wires.)
• There are some pacemaker wires that do have lumens, which may be considered a central line.
Types of Central Lines for NHSN reporting purposes:
1. Permanent central line: Includes:
a. Tunneled catheters, including tunneled dialysis catheters
b. Implanted catheters (including ports)
2. Temporary central line: A non-tunneled, non-implanted catheter
3. Umbilical catheter: A vascular catheter inserted through the umbilical artery or vein in a neonate. All
umbilical catheters are central lines
Eligible Central Line: A CL that has been in place for more than two consecutive calendar days (
on or after CL
day 3), following the first access of the central line, in an inpatient location, during the current admission. Such
lines are eligible for CLABSI events and remain eligible for CLABSI events until the day after removal from the
body or patient discharge, whichever comes first. (See Table 3 for examples).
Eligible BSI Organism: Any organism that is eligible for use to meet LCBI or MBI-LCBI criteria. In other words, an
organism that is not an excluded pathogen for use in meeting LCBI or MBI-LCBI criteria. These organisms may or
may not be included on the NHSN Organisms List accessed via the spreadsheet or refer to the new
NHSN
Terminology Browser. Contact NHSN for guidance regarding organisms that are not included on the NHSN
Organisms List.
Central line-associated BSI (CLABSI): A laboratory confirmed bloodstream infection where an eligible BSI
organism is identified, and an eligible central line is present on the LCBI DOE or the day before.
Central line days: The number of days a central line is accessed to determine if an LCBI is a CLABSI.
Denominator device days: The count of central lines on an inpatient unit that is recorded in the monthly
denominator summary data. This count begins on the first day the central line is present, regardless of access.

January 2024 Device-associated Module
BSI
4 - 6
Devices Not Considered Central Lines for NHSN Reporting Purposes:
• Arterial catheters unless in the pulmonary artery, aorta, or umbilical artery
• Arteriovenous fistula
• Arteriovenous graft
• Atrial catheters (also known as transthoracic intra-cardiac catheters, those catheters inserted directly
into the right or left atrium via the heart wall)
• Extracorporeal life support (ECMO)
• Hemodialysis reliable outflow (HERO) dialysis catheter
• Intra-aortic balloon pump (IABP) devices
• Peripheral IV or Midlines
• Ventricular Assist Device (VAD)
Table 1: Laboratory-Confirmed Bloodstream Infection Criteria:
Must meet one of the following LCBI criteria:
Criterion
Comments and reporting instructions that follow the site-specific criteria provide further
explanation and are integral to the correct application of the criteria.
Once an LCBI determination is made, proceed to the MBI-LCBI definitions, and determine if
the corresponding MBI-LCBI criteria are also met (for example, after meeting LCBI 2,
investigate for potential MBI-LCBI 2)
LCBI 1
If LCBI 1
criterion is
met,
consider
MBI-LCBI 1
Patient of any age has a recognized bacterial or fungal pathogen, not included on the NHSN
common commensal list:
1. Identified from one or more blood specimens obtained by a culture
OR
2. Identified to the genus or species level by non-culture based microbiologic testing
(NCT)* methods (for example, T2 Magnetic Resonance [T2MR] or next-generation
sequencing (NGS). Note: If blood is collected for culture within 2 days before, or 1
day after the NCT, disregard the result of the NCT and use only the result of the
CULTURE to make an LCBI surveillance determination. If no blood is collected for
culture within this time period, use the result of the NCT for LCBI surveillance
determination.
AND
Organism(s) identified in blood is not related to an infection at another site
(See Appendix: Secondary BSI Guide
).
*For the purposes of meeting LCBI 1, NCT is defined as a methodology that identifies an
organism directly from a blood specimen without inoculation of the blood specimen to any
culture media.

January 2024 Device-associated Module
BSI
4 - 7
Notes:
1. If a patient meets both LCBI 1 and LCBI 2 or LCBI 3 criteria, report LCBI 1 with the
recognized pathogen entered as pathogen #1 and the common commensal as
pathogen #2.
2. An eligible organism in the blood specimen is the only element needed to meet LCBI
1 criterion; therefore, the LCBI 1 DOE will always be the collection date of the first
positive blood specimen used to set the BSI IWP.
LCBI 2
If LCBI 2
criterion is
met,
consider
MBI-LCBI 2
Patient of any age has at least one of the following signs or symptoms: fever (>38.0
o
C), chills,
or hypotension
AND
Organism(s) identified in blood is not related to an infection at another site
(See Appendix: Secondary BSI Guide
).
AND
The same NHSN common commensal is identified by culture from two or more blood
specimens collected on separate occasions (see Blood Specimen Collection
).
For common commensal organisms, see the Common Commensal tab of the NHSN Organism
List accessed via the spreadsheet or refer to the new NHSN Terminology Browser
.
Notes:
1. Criterion elements must occur within the 7-day IWP (as defined in Chapter 2
) which
includes the collection date of the positive blood specimen, the 3 calendar days
before and the 3 calendar days after.
2. The two matching common commensal specimens represent a single element for use
in meeting LCBI 2 criterion, and the collection date of the first specimen is used to
determine the BSI IWP.
3. At least one element (specifically, a sign or symptom of fever, chills, or hypotension)
is required to meet LCBI 2 criterion; the LCBI 2 DOE will always be the date the first
element occurs for the first time during the BSI IWP, whether that be a sign or
symptom or the positive blood specimen.

January 2024 Device-associated Module
BSI
4 - 8
--
6/1
Fever > 38.0 °C
LCBI 2 DOE = 6/1
--
6/2
No LCBI element
--
--
6/3
No LCBI element
--
Single
element
6/4
S. epidermidis (1 of 2)
Date of 1st diagnostic
test = 6/4
6/5
S. epidermidis (2 of 2)
--
--
6/6
No LCBI element
--
--
6/7
No LCBI element
--
LCBI 3
If LCBI 3
criterion is
met,
consider
MBI-LCBI 3
Patient ≤ 1 year of age has at least one of the following signs or symptoms:
fever (>38.0
o
C), hypothermia (<36.0
o
C), apnea, or bradycardia
AND
Organism(s) identified in blood is not related to an infection at another site
(See Appendix: Secondary BSI Guide
).
AND
The same NHSN common commensal is identified by a culture from two or more blood
specimens collected on separate occasions (see Blood Specimen Collection
).
For common commensal organisms, see the Common Commensal tab of the NHSN Organism
List accessed via the spreadsheet or refer to the new NHSN Terminology Browser
.
Notes:
1. Criterion elements must occur within the 7-day IWP (as defined in Chapter 2
) which
includes the collection date of the positive blood specimen, the 3 calendar days
before and the 3 calendar days after.
2. The two matching common commensal specimens represent a single element for use
in meeting LCBI 3 criterion, and the date of the first is used to determine the BSI IWP.

January 2024 Device-associated Module
BSI
4 - 9
At least one element (specifically, a sign or symptom of fever, hypothermia, apnea, or
bradycardia) is required to meet LCBI 3 criterion; the LCBI 3 DOE will always be the date the
first element occurs for the first time during the BSI IWP whether that be a sign or symptom
or the positive blood specimen.
--
5/31
No LCBI element
--
-
6/1
No LCBI element
-
-
6/2
No LCBI element
-
Single
element
6/3
S. epidermidis (1 of 2)
Date of 1st diagnostic test = 6/3
LCBI DOE = 6/3
6/4
S. epidermidis (2 of 2)
-
-
6/5
Apnea documented
-
-
6/6
No LCBI element
-

January 2024 Device-associated Module
BSI
4 - 10
Table 2: Mucosal Barrier Injury Laboratory-Confirmed Bloodstream Infection (MBI-
LCBI)
An MBI-LCBI is a subset of the LCBI criteria; therefore, a BSI event must fully meet an LCBI criterion before
evaluating for the corresponding MBI-LCBI criterion.
The MBI-LCBI DOE will always be the date the prerequisite LCBI criteria are met. Abnormal ANC and WBC
values reflect risk factors for acquiring an MBI-LCBI, not symptoms of infection and therefore are not used in
DOE determinations.
Must meet one of the following MBI-LCBI criteria
MBI-LCBI 1
MBI-LCBI 2
MBI-LCBI 3
Patient of any age fully meets LCBI 1
criterion
Patient of any age fully meets
LCBI 2 criterion
Patient <1 year of age fully meets
LCBI 3 criterion
with at least one blood specimen with at least two matching blood specimens
with ONLY intestinal organisms from
the NHSN MBI organism list*
with ONLY Viridans Group Streptococcus and/or Rothia spp. alone
but no other organisms†
identified by culture or non-culture
based microbiologic testing method
identified by culture
AND
Patient meets at least one of the following:
1. Is an allogeneic hematopoietic stem cell transplant recipient within the past year with one of the
following documented during same hospitalization as positive blood specimen:
a. Grade III or IV gastrointestinal graft versus host disease [GI GVHD]
OR
b. ≥1-liter diarrhea in a 24-hour period (or ≥20 mL/kg in a 24-hour period for patients <18 years of age)
with onset on or within the 7 calendar days before the date the positive blood specimen was
collected.
OR
2. Is neutropenic, defined as at least two separate days with ANC
†
and/or WBC values <500 cells/mm
3
collected within a 7-day time period which includes the collection date of the positive blood specimen,
the 3 calendar days before and the 3 calendar days after (See Table 5).

January 2024 Device-associated Module
BSI
4 - 11
Notes:
1. If a patient meets both MBI-LCBI 1 and MBI-LCBI 2 or MBI-LCBI 3 criteria (specifically has Viridans Group
Streptococcus or Rothia spp. and only MBI organisms in the blood specimen), report organisms as MBI-
LCBI 1 with the recognized pathogen as pathogen #1 and the common commensal as pathogen #2.
2. Any combination of ANC and/or WBC values can be used to meet neutropenic criteria provided they are
collected on separate days within the 7-day period that includes the date of the positive blood
specimen, the 3 calendar days before and the 3 calendar days after.
3. When a blood specimen positive for an organism not included on the NHSN MBI organism list is
collected during the BSI RIT of an MBI-LCBI, the initial MBI-LCBI event is edited to an LCBI and the
identified non-MBI organism is added.
*See the MBI organism tab on the NHSN Organism List accessed via the spreadsheet or refer to the new
NHSN Terminology Browser for eligible MBI organisms.
†Eligible positive blood specimens must be collected on separate occasions and limited to the following:
• Viridans Group Streptococcus identified in at least two sets of blood specimens
• Rothia spp. identified in at least two sets of blood specimens
• Viridans Group Streptococcus and Rothia spp. identified in at least two sets of blood specimens
†
Formula for calculating ANC if not provided by your laboratory:
• The ANC is not always reported directly in the chart
• The WBC in the chart is usually reported in terms of a thousand
cells/mm
3
and can be used to calculate the ANC
ANC = Absolute Segs + Absolute Bands
OR
ANC = WBC X %Segs + %Bands ÷ 100
Example:
WBC
Segs
Bands
2 k/mm
3
20%
20%
ANC
=
2000 X (20
+
20)
÷
100
=
800 cells/mm
3

January 2024 Device-associated Module
BSI
4 - 12
Reporting Instructions: See below for a Summary of CLABSI Exclusions and
Reporting Requirements.
When a BSI event in the presence of a central line meets one of the CLABSI exclusions listed below the
following guidelines are applied:
• The event is reported to NHSN but is NOT considered central line associated.
• The Central Line field is marked “Yes” if an eligible central line was in place on the BSI DOE and is still in
place on the BSI DOE or the day before.
• The events do not contribute to the CLABSI SIR measure.
• In each instance where the date of event of subsequent positive blood specimens are outside of the
established BSI RIT, meeting the exclusion criteria, the subsequent positive blood must be investigated
as primary or secondary to another site-specific infection. The CLABSI exclusion criteria must be met
again in a new BSI IWP to determine if the positive blood specimen is central line associated.
Note: Meeting LCBI criteria in all situations noted below will result in setting a BSI RIT and any associated device
days should be included in the denominator summary data counts.
a. Extracorporeal life support (ECLS or ECMO): A BSI meeting LCBI criteria with an eligible central line
where extracorporeal life support (for example, extracorporeal membrane oxygenation [ECMO]) is
present for more than 2 days on the BSI DOE and is still in place on the DOE or the day before, is
considered an LCBI. Report such events, marking the ECMO field as “Yes.”
b. Ventricular Assist Device (VAD): A BSI meeting LCBI criteria with an eligible central line where a VAD is
present for more than 2 days on the BSI DOE and is still in place on the DOE or the day before, is
considered an LCBI. Report such events, marking the VAD field as “Yes.”
c. Patient Injection: A BSI meeting LCBI criteria that is accompanied by documentation of observed or
suspected patient injection into the vascular access line, within the BSI IWP, will be considered an LCBI
for NHSN reporting purposes. This exclusion is very specific to “INJECTION”. Manipulating or tampering
with the line (such as biting, picking at, sucking on, etc.) DOES NOT meet the intent of this exclusion.
The documentation must specifically state the patient was “observed injecting…” or “suspected of
injecting…” the device. Insinuations or descriptive events that suggest such behavior DO NOT meet the
intent of this exclusion. Report such events, marking the Patient Injection field as “Yes.”
d. Epidermolysis bullosa (EB): If during the current admission, there is documentation of a diagnosis of EB
report such an event, marking the EB field as “Yes.”
Note: The Epidermolysis bullosa (EB) CLABSI exclusion is limited to the genetic forms of EB in the
pediatric population.
e. Munchausen Syndrome by Proxy (MSBP): If during the current admission, there is documentation or a
diagnosis of known or suspected MSBP, also known as factitious disorder imposed on another (FDIA),
report such an event, marking the MSBP fields as “Yes.”

January 2024 Device-associated Module
BSI
4 - 13
f. Pus at the vascular access site: Occasionally, a patient with both an eligible central line and another
vascular access device will have pus at the other access site. If there is pus at the site of one of the
following vascular access devices and a specimen collected from that site has at least one matching
organism to an organism identified in the blood during the BSI IWP, report such events marking the “pus
at the vascular access site” field as “Yes.” Vascular access devices included in this exception are limited
to:
• Arterial catheters unless in the pulmonary artery, aorta or umbilical artery
• Arteriovenous fistulae
• Arteriovenous grafts
• Atrial catheters (also known as transthoracic intra-cardiac catheters, those catheters inserted
directly into the right or left atrium via the heart wall)
• Hemodialysis reliable outflow (HERO) dialysis catheters
• Intra-aortic balloon pump (IABP) devices
• Non-accessed CL (those neither inserted nor used during current admission)
• Peripheral IV or Midlines
Reporting Instructions:
1. Group B Streptococcus: Group B Streptococcus identified from blood, with a date of event during the
first 6 days of life, is not reported as a CLABSI. A BSI RIT is set, and any associated device days should be
included in the denominator summary data counts.
2. Do not report an LCBI that has a DOE within a BSI RIT. Any additional organisms identified meeting LCBI
criteria are added to the initial BSI event. See RIT guidance in Chapter 2
, Identifying Healthcare
associated Infections or Chapter 16, Key Terms.
3. Do not report an MBI-LCBI that has a DOE within a BSI RIT. Any additional organisms identified meeting
MBI-LCBI criteria are added to the initial BSI event. See RIT guidance in Chapter 2
, Identifying Healthcare
associated Infections.
4. Only primary BSIs create a 14-day BSI RIT:
Primary BSI example: Patient has a positive blood specimen identifying Staphylococcus aureus on
hospital day 6, which is not secondary to another site-specific source of infection. A subsequent positive
blood specimen is collected on hospital day 12 that identifies Pseudomonas aeruginosa. Because the
date of event is during the BSI RIT, no new BSI event is reported, and Pseudomonas is added to the initial
BSI event.
5. Secondary BSIs do not create a 14-day BSI RIT:
Secondary BSI example: A symptomatic urinary tract infection (SUTI) with Enterococcus faecalis is
identified and E. faecalis is also identified from a blood specimen on hospital day 11. Because the
positive blood culture is collected during the SUTI secondary BSI attribution period, the positive E.

January 2024 Device-associated Module
BSI
4 - 14
faecalis blood specimen is deemed secondary to the SUTI. Since the BSI is secondary to the SUTI, a SUTI
RIT is set, not a BSI RIT. On hospital day 15 (also within the SUTI RIT and secondary BSI attribution
period), a blood culture growing Staphylococcus aureus is collected. Because the blood growing S.
aureus does not have at least one organism that matches the organism used to meet the SUTI criterion,
the BSI cannot be attributed as secondary to the SUTI. Additionally, there is no BSI RIT established;
therefore, the BSI will need to be investigated as a new BSI event and either assigned as primary or
secondary to another site specific infection.
Note: The secondary BSI attribution period of a primary source of infection is not a “catch all” for
subsequent BSIs.
6. There is no expectation that positive blood specimens collected during the present on admission (POA)
time period are investigated. If identified, they are not reported to NHSN. However, if a subsequent
positive blood specimen is collected within 14 days of a positive blood specimen collected during the
POA time period, it is imperative that a determination is made for the original blood specimen in order
to make the correct determination about the subsequent blood specimen.
Example 1: A patient has a positive blood specimen with Escherichia coli (E. coli) that is a POA on 6/1.
On 6/10, a subsequent positive blood specimen with Klebsiella pneumonia is identified. The 6/1 blood
specimen is investigated and if determined a primary BSI, sets a 14-day BSI RIT (6/1-6/14). Therefore,
the 6/10 specimen is not a new BSI event and K. pneumonia is added to the POA BSI event if reported.
Example 2: A patient has a positive blood specimen that identifies Staphylococcus aureus present on
admission 6/1. On 6/10, a subsequent positive blood specimen with Klebsiella pneumonia is collected.
To make the correct determination about the second blood specimen, the initial POA BSI event must be
investigated to determine if it is primary or secondary to another site. In reviewing the chart, a right
elbow culture from 5/31, is also positive for S. aureus, plus the symptoms needed to meet Joint or Bursa
infection (JNT) criterion 3c are documented making the 6/1 BSI secondary to JNT. The POA primary JNT
infection creates a 14-day JNT RIT (6/1-6/14) during which no new JNT infections are reported.
Additionally, since the subsequent blood specimen does not contain at least one matching pathogen to
the specimen used to meet the JNT criterion, the positive blood with K. pneumonia cannot be
attributed to the original JNT event and must be investigated as a primary or secondary BSI.
Blood Specimen Collection
The “two or more blood specimens drawn on separate occasions” criterion is met if there is blood collected
from at least two separate blood draws on the same or consecutive calendar days.
AND
the blood cultures are assigned separate specimen numbers, processed individually, and are reported separately
in the final laboratory report.

January 2024 Device-associated Module
BSI
4 - 15
1. Specimen Collection Considerations: Blood specimens drawn through central lines can have a higher rate of
contamination than blood specimens collected through peripheral venipuncture.
3, 4
However, all positive
blood specimens, regardless of the site from which they are drawn or the purpose for which they are
collected, must be included when conducting in-plan CLABSI surveillance (for example, weekly blood
cultures performed in hematology and oncology locations).
2. Catheter tip cultures cannot be used in place of blood specimens for meeting LCBI criteria.
3. In MBI-LCBI 1, 2 and 3, “no other organisms” means there is no identification of a non-MBI-LCBI pathogen
(such as S. aureus) or 2 matching common commensals (such as coagulase-negative staphylococci) collected
from the blood on separate occasions that would otherwise meet LCBI criteria. If this occurs, the infection
does not meet MBI-LCBI criteria.
4. When a blood specimen positive for an organism not included on the NHSN MBI organism list is collected
during the BSI RIT of an MBI-LCBI, the initial MBI-LCBI event is edited to an LCBI and the identified non-MBI
organism is added.
MBI-RIT Exception: An MBI-LCBI designation will not change to an LCBI event if the following criteria are
met:
1. The blood culture with the non-MBI organism is collected during an existing BSI (MBI-LCBI) RIT
AND
2. The blood culture with the non-MBI organism is deemed secondary to an NHSN site-specific
infection
See Example 5 in the Secondary BSI Guide section of this protocol and Chapter 2
Pathogen Assignment
(Example 2b).

January 2024 Device-associated Module
BSI
4 - 16
Table 3: Examples of Associating the Use of Central Lines to BSI Events
(CLABSI):
This table provides examples that illustrate:
• Device association as determined by the presence of an eligible CL on the BSI DOE or the day
before.
• The goal of NHSN HAI surveillance is to identify risks to the patient that are the result of device
use in general; therefore, NHSN does not require association of a BSI with a specific device when
more than one line is present.
Note: The procedure for de-accessing a port involves ensuring patency of the line prior to removal
of the needle which involves blood withdrawal, an IV flush and injection of an anticoagulant.
Date
31-Mar
1-Apr
2-Apr
3-Apr
4-Apr
5-Apr
6-Apr
Patient A:
Port Status
Port in
Port in
Port in
Port in
Port in
Port in
Port in
Accessed
No No Yes Yes
Yes
De-accessed
No No
Eligible for
CLABSI
event
No No No No
Yes-eligible
CL
Yes-eligible CL
Yes-eligible
CL
- -
CL
Day 1
CL
Day 2
CL
Day 3
CL
Day 4
CL
Day 5
Patient A becomes eligible for a CLABSI on 4/4 because an accessed port is in place for some portion of > 2 consecutive
calendar days making it an eligible CL on 4/4 (CL Day 3). The port remains eligible for a CLABSI until it is removed, or the
patient is discharged, whichever comes first.
Date
31-Mar
1-Apr
2-Apr
3-Apr
4-Apr
5-Apr
6-Apr
Patient B:
CL/Port
Status
CL/Port in CL/Port in CL/Port in CL/Port in
CL/Port in
CL/Port out
No device No device
Accessed
No
No
Yes
Yes
Removed
-
-
Eligible for
CLABSI
event
No No No No
Yes-eligible
CL
Yes-eligible
CL
No
- -
CL
Day 1
CL
Day 2
CL
Day 3
- -
Patient B is eligible for a CLABSI on 4/4 (CL Day 3) through 4/5. An accessed device (CL or port) is in place > 2
consecutive calendar days making it an eligible CL on 4/4 (CL Day 3). A BSI with a DOE on the day of or the day after
device removal or patient discharge is considered device associated (CLABSI).

January 2024 Device-associated Module
BSI
4 - 17
BOLD = change in status
Date
31-Mar
1-Apr
2-Apr
3-Apr
4-Apr
5-Apr
6-Apr
Patient C:
CL Status
CL in CL in CL in/ CL out CL in CL in CL in/ CL out No device
Accessed
Yes
Yes
Removed
Placed
Yes
Removed
-
Eligible for
CLABSI
event
Yes-eligible
CL
Yes- eligible
CL
Yes- eligible
CL
Yes- eligible
CL
Yes- eligible
CL
Yes- eligible
CL
Yes-
eligible CL
CL
Day 3
CL
Day 4
CL
Day 5
CL
Day 6
CL
Day 7
CL
Day 8
-
Patient C is admitted to an inpatient location on 3/29 with a central line in place. Patient C is eligible for a CLABSI on 3/31
(CL Day 3) through 4/6 because an accessed CL is in place > 2 consecutive calendar days. A BSI with a DOE on the day of or
the day after device removal or patient discharge is considered a device-associated infection (CLABSI). The patient remains
eligible for a CLABSI event through 4/6 because a full calendar day did not pass without a CL in place, therefore, device
counts continue uninterrupted.
Date
31-Mar 1-Apr 2-Apr 3-Apr 4-Apr 5-Apr 6-Apr
Patient D:
CL Status
CL in CL in CL in/ CL out No device CL in CL in CL in
Accessed
Yes
Yes
Removed
-
Placed
Yes
Yes
Eligible for
CLABSI
event
Yes-eligible
CL
Yes-eligible
CL
Yes-eligible
CL
Yes-eligible
CL
No No
Yes-eligible
CL
CL
Day 3
CL
Day 4
CL
Day 5
-
CL
Day 1
CL
Day 2
CL
Day 3
Patient D is admitted to an inpatient location on 3/29 with a central line in place. Patient D is eligible for a CLABSI 3/31 (CL
Day 3) through 4/3. An accessed CL had been in place > 2 consecutive calendar days, however, a full calendar day passed
(4/3) with no CL in place, therefore, device day counts start over at CL day 1 when a new line is placed. After 4/3, the
patient will not be eligible for a CLABSI event again until 4/6 when the new CL becomes an eligible CL (CL Day 3).
Date
31-Mar
1-Apr
2-Apr
3-Apr
4-Apr
5-Apr
6-Apr
Patient E:
CL Status
No device CL in CL in CL in CL in CL in CL in
Accessed
-
Placed
Yes
Yes
Yes
Yes
Yes
Eligible for
CLABSI
event
- No No
Yes-eligible
CL
Yes-eligible
CL
Yes-eligible
CL
Yes-eligible
CL
-
CL
Day 1
CL
Day 2
CL
Day 3
CL
Day 4
CL
Day 5
CL
Day 6
Patient E is eligible for a CLABSI on 4/3 (CL Day 3) through 4/6. Line placement is considered access and begins device day
counts for making a CLABSI determination. An accessed device is in place > 2 consecutive calendar days making it an eligible
CL on 4/3 (CL Day 3).

January 2024 Device-associated Module
BSI
4 - 18
Pathogen Exclusions and Reporting Considerations:
The term “recognized pathogen” in LCBI 1 criterion refers to any organism that is not included on the
NHSN common commensal list (see the NHSN Organism List accessed via the spreadsheet
or refer to the
new NHSN Terminology Browser for common commensals used for NHSN reporting purposes).
Exceptions:
a. Organisms that are parasites and viruses are excluded as LCBI pathogens. This exclusion applies
to meeting a primary BSI only. Viruses and parasites are eligible for use in secondary BSI
determinations.
b. Organisms belonging to the following genera are excluded as LCBI pathogens: Campylobacter,
Salmonella, Shigella, Listeria, Vibrio and Yersinia as well as C. difficile, Enterohemorrhagic E. coli,
and Enteropathogenic E. coli. These organisms are eligible for use in secondary BSI
determinations but are not reported as the sole pathogen in a primary BSI.
c. Organisms belonging to the following genera cannot be used to meet any NHSN definition:
Blastomyces, Histoplasma, Coccidioides, Paracoccidioides, Cryptococcus, and Pneumocystis. These
organisms are excluded because they typically cause community-associated infections and are
rarely known to cause healthcare-associated infections.
1. Business rules written into the pathogen fields of the NHSN application prevent entry of a common
commensal as pathogen #1 when attempting to report both a recognized pathogen and common
commensal identified in an LCBI 1 or MBI-LCBI 1 event. To save the event successfully, enter the
recognized pathogen as pathogen # 1 and the common commensal as pathogen #2.
2. For LCBI criteria 2 and 3, if the common commensal is identified to the species level for one blood
specimen, and a companion blood specimen is identified with only a descriptive name, which is
complementary to the companion culture (in other words, to the genus level), then it is assumed the
organisms are the same.
• Colony morphology, biotype, and antibiogram comparisons should not be used to determine the
“sameness “of organisms because laboratory testing capabilities and protocols vary between
facilities.
• To reduce reporting variabilities due to differences in laboratory practice only genus and species
identification should be used, and they should only be reported once.
• An organism identified to the species level should be reported along with the antibiogram, if
available. If antibiograms are available and the sensitivities differ for the same organisms in
separate specimens, always report the more resistant panel (see Table 4
).
3. A common commensal identified in a single blood specimen is considered a contaminant. A single
common commensal organism is not used to meet LCBI 2 or 3 criteria or secondary BSI attribution.
Additionally, it does not prevent a case from meeting MBI-LCBI criteria when the organism
requirements call for “only” a specific organism or type of organism (for example, “only intestinal
organisms from the MBI list”).
January 2024 Device-associated Module
BSI
4 - 19
Table 4: Reporting Speciated and Unspeciated Organisms Identified from Blood
Specimens
Culture Report
Companion Culture Report
Report as…
Coagulase-positive staphylococci
S. aureus
S. aureus
S. epidermidis
Coagulase-negative staphylococci
S. epidermidis
Enterococcus spp.
E. faecium
E. faecium
Bacillus spp. (not anthracis)
B. cereus
B. cereus
S. salivarius
Strep viridans
S. salivarius
Note: When identification to the species level is not provided, the genus of the organism will be reported
to NHSN. When identification to the genus level is not provided, report the organism as available on the
NHSN organism list (for example, Gram-positive bacillus).
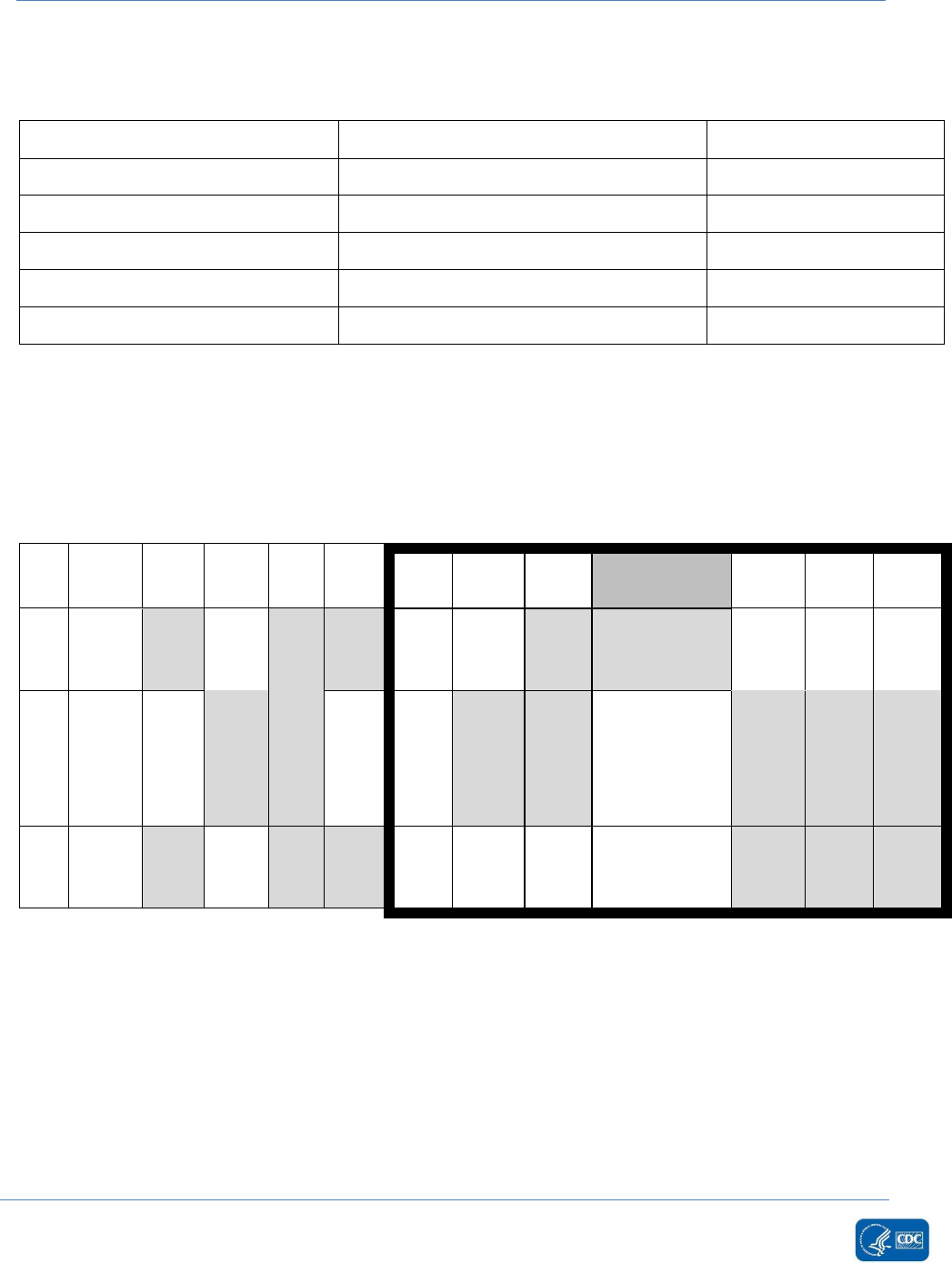
Table 5: Examples Illustrating the MBI-LCBI Criteria for Neutropenia
ND = not done; *Collection date of positive blood specimen; Italics = ANC/WBC < 500 cells/mm
3
; †
ANC/WBC < 500 cells/mm
3
used
to meet neutropenia for MBI-LCBI criteria
Rationale for Table 5:
Patient A meets MBI-LCBI 1 criterion with neutropenia: Positive blood specimen with intestinal organism
(Candida spp.) and neutropenia*. In this case, the WBC values on Day 1 = 400, and Day -1 = 320 are used.
Patient B meets MBI-LCBI 2 criterion with neutropenia: At least two positive blood specimens with
viridans group streptococci, fever >38°C and neutropenia*. In this case, the ANC values on day -1 = 110
and Day -2 = 120 are used.
-
-
Day
-7
Day
-6
Day
-5
Day
-4
Day
-3
Day
-2
Day
-1
Day
1*
Day
2
Day
3
Day
4
Pt.
A
WBC
100
800
400
300
ND
ND
320†
400†
+ BC* x 1
Candida
spp.
ND
550
600
Pt.
B
ANC
ND
410
130
ND
ND
120†
110†
ND
+BC* x 2
viridans strep
plus fever
>38°C
110
300
320
Pt.
C
WBC
100
800
400
300
ND
ND
ND
600
+ BC* x 1
Candida spp.
230†
ND
400†

January 2024 Device-associated Module
BSI
4 - 20
Note: Any two of Days -2, -1, 2, 3, and 4 could be used to meet this requirement since WBC and/or ANC
values of <500cells/mm
3
were present on those days.
Patient C meets MBI-LCBI 1 criterion with neutropenia: Positive blood specimen with intestinal organism
(Candida spp.) and neutropenia*. In this case, WBC values on Day 2 = 230 and Day 4 = 400 are used.
*Neutropenia is defined as: 2 separate days of ANC or WBC <500 cells/mm
3
occurring on the collection
date of the positive blood specimen (Day 1) or during the 3 days before or the 3 days after Day 1.
Monthly Summary Data
Numerator Data: The Primary Bloodstream Infection (BSI) form (CDC 57.108)
is used to collect and report
each CLABSI that is identified during the month selected for surveillance. For CLABSI surveillance, all LCBI
and MBI-LCBI that are identified as central-line associated must be included. The Instructions for
Completion of Primary Bloodstream Infection (BSI) form contains brief instructions for collection and
entry of each data element on the form. The Primary BSI form includes patient demographic information
and whether a central line was present, and, if so, the type of central line the patient had if appropriate to
the location; these data will be used to calculate line-specific infection rates. Additional data include the
specific criteria met for identifying the primary BSI, whether the patient died, organisms identified from
blood specimens, and the organisms’ antimicrobial susceptibilities.
Reporting Instruction:
During the month of surveillance, if no CLABSI events are identified, the “Report No Events” box must be
checked on the appropriate denominator summary screen, (for example, Denominators for Intensive Care
Unit [ICU]/other locations [not NICU or SCA], etc.

January 2024 Device-associated Module
BSI
4 - 21
Table 6: Examples of Denominator Day counts for Device Days
This table provides examples that illustrate:
• Denominator device day counts for a central line present on an inpatient location at the time of
the device day count.
Note: If the central line is in place at the time of the denominator device count, it is included in the daily
denominator device day count.
Date
31-Mar
1-Apr
2-Apr
3-Apr
4-Apr
5-Apr
6-Apr
Patient A:
Inpatient
Location ICU
CL inserted
ICU
CL in
ICU
CL in
ICU
CL in
ICU
CL in
ICU
CL in
ICU
CL in
Denominator
Day Counts
for Device
Days
Day 1 Day 2 Day 3 Day 4 Day 5 Day 6 Day 7
Patient A has a CL inserted in the ICU. Because the CL is inserted in an inpatient location, Day 1 begins the
denominator day count for device days. Patient A has 7 denominator device days for 3/31-4/6.
Date
31-Mar
1-Apr
2-Apr
3-Apr
4-Apr
5-Apr
6-Apr
Patient B:
ED
CL in place at
time of
admission
Patient
admitted to
inpatient
location ICU
CL in
ICU
CL in
ICU
CL in
ICU
CL in
Inpatient
Location
CL in
Inpatient
Location
CL in
Denominator
Day Counts
for Device
Days
- Day 1 Day 2 Day 3 Day 4 Day 5 Day 6
Patient B has a central line at the time of admission. Because Patient B is admitted to the emergency department
on 3/31, the denominator day count for device days does not begin until the patient is transferred to the inpatient
location on 4/1. Patient B has 6 denominator device days for 4/1-4/6.

January 2024 Device-associated Module
BSI
4 - 22
Date
31-Mar
1-Apr
2-Apr
3-Apr
4-Apr
5-Apr
6-Apr
Patient D:
Inpatient
Location ICU
No device
Inpatient
Location ICU
CL inserted
ICU
CL in
ICU
CL in
ICU
CL in
ICU
CL in
ICU
CL in
Denominator
Day Counts
for Device
Days
- Day 1 Day 2 Day 3 Day 4 Day 5 Day 6
Patient D does not have a central line in place at the time of admission to ICU. Because there is no central line in
place on admission, the denominator day count for device days does not begin until the central line is placed in
the inpatient location on 4/1. Patient D has 6 denominator device days for 4/1-4/6.
Date
31-Mar
1-Apr
2-Apr
3-Apr
4-Apr
5-Apr
6-Apr
Patient E:
Inpatient
Location ICU
Patient
admitted
with non-
accessed
port
Inpatient
Location ICU
Port not
accessed
ICU
Port not
accessed
ICU
Port
accessed
ICU
Port
accessed
ICU
Port
accessed
ICU
Port
accessed
Denominator
Day Counts
for Device
Days
Day 1 Day 2 Day 3 Day 4 Day 5 Day 6 Day 7
Patient E has a non-accessed port at the time of admission to ICU. The denominator device day count begins on
the date the patient is admitted to ICU (3/31). Accessing the port on 4/3 does not change the denominator day
count for device days. Patient E has 7 denominator device days for 3/31-4/6.
Date
31-Mar
1-Apr
2-Apr
3-Apr
4-Apr
5-Apr
6-Apr
Patient C:
Inpatient
Location ICU
CL in place at
time of
admission
ICU
CL in
ICU
CL in/ CL out
ICU
CL in
ICU
CL in
ICU
CL in/ CL out
ICU
No device
Denominator
Day Counts
for Device
Days
Day 1 Day 2 Day 3* Day 4 Day 5 Day 6* -
Patient C has a central at the time of admission to ICU. Because Patient C is admitted to ICU on 3/31, the
denominator day count for device days begins on the date of admission (3/31). Because there is no device on 4/6,
the denominator device day count will end on 4/5. Patient C has 6 denominator device days for 3/31-4/5.

January 2024 Device-associated Module
BSI
4 - 23
Table 7: Denominator Data Collection Methods
Denominator Data: Device days and patient days are used for denominator reporting. Device-day
denominator data that are collected differ according to the patient location. The following methods can
be used for the collection of denominator data:
Data Collection
Method
Details
Manual, Daily
Denominator data (patient days and device days) should be collected at the
same time, every day, for each location performing surveillance to ensure that
differing collection methods don’t inadvertently result in device days being
greater than patient days.
• For locations other than specialty care areas/oncology (SCA/ONC) and
NICUs, the number of patients with at least one central line, of any type, is
collected daily, at the same time each day during the month and is recorded
on the
Denominators for Intensive Care Unit (ICU)/Other Locations (Not NICU
or SCA/ONC) form (CDC 57.118). Only the totals for the month are entered
into NHSN.
Notes:
1. Only one central line per patient is counted per calendar day regardless
of the number of central lines present.
2. All central lines on inpatient units should be included in device day
counts regardless of access.
• For specialty care areas/oncology, the number of patients with at least one
central line are separated into those with permanent central lines and those
with temporary central lines. The number of patients with at least one
central line, of either or both type(s), is collected daily, at the same time
each day during the month and is recorded on the
Denominators for
Specialty Care Area (SCA)/Oncology (ONC) form (CDC 57.117). Only the
totals for the month are entered into NHSN. Temporary and permanent
lines are reported separately in this location because permanent lines are
more commonly used in this patient population and may be associated with
a lower BSI rate when compared to temporary central lines.
Notes:
1. Only one central line per patient is counted per calendar day regardless
of the number of central lines present.
2. All central lines on inpatient units should be included in device day
counts regardless of access.

January 2024 Device-associated Module
BSI
4 - 24
Data Collection
Method
Details
3. If a patient has both a temporary and a permanent central line, only
report the temporary line because it is associated with a higher risk of
bloodstream infection.
The Instructions for Completion of Denominators for Intensive Care Unit
(ICU)/Other Locations (Not NICU and SCA/ONC) and Instructions for
Completion of Denominators for Specialty Care Areas (SCA)/Oncology (ONC)
contain brief instructions for collection and entry of each data element on
the form.
• In
NICUs, the number of patients with at least one central line is stratified by
birth weight in five categories because the risk of BSI varies by birth weight.
These data are reported on the Denominators for Neonatal Intensive Care
Unit (NICU) form (CDC 57.116).
Note:
1. Report only birth weight when entering BSI denominator data. The
infant’s weight at the time of BSI identification is not used and should
not be reported. For example, a neonate weighs 1006 grams at birth but
remains in the NICU for two months and has a body weight of 1650
grams when a CLABSI develops; enter the birth weight of 1006 grams on
the BSI form.
2. All central lines on inpatient units should be included in device day
counts regardless of access. The
Instructions for Completion of
Denominators for Neonatal Intensive Care Unit (NICU) form contains
brief instructions for collection and entry of each data element on the
forms.
Manual, sampled
once/week (collected
at the same time on
the same designated
day, once per week)
• To reduce staff time spent collecting surveillance data, once weekly sampling
of denominator data to generate estimated central line days, may be used as
an alternative to daily collection in non-oncology ICUs and wards (see Notes
below). Sampling may not be used in SCA/ONC locations or NICUs. During
the month, the number of patients in the location (patient-days) and the
number of patients with at least one central line of any type (central line
days) is collected on a designated day each week (for example, every
Tuesday), and at the same time each day.
• Evaluations of this method have repeatedly shown the use of Saturday or
Sunday generate the least accurate estimates of denominator data;
therefore, weekend days should not be selected as the designated

January 2024 Device-associated Module
BSI
4 - 25
Data Collection
Method
Details
denominator data collection day.
6-8
If the designated day is missed, collect
the denominator data on the next available weekday.
• The following must be collected and entered into NHSN:
1. The monthly total for patient-days, collected daily
2. The sampled total for patient-days
3. The sampled total central line-days
When these data are entered, the NHSN application will calculate an
estimate of central line-days.
Notes:
1. To ensure the accuracy of estimated denominator data obtained by
sampling, only ICU and ward location types with an average of 75 or
more central line-days per month are eligible to use this method. A
review of each location’s central line denominator data for the past
twelve months in NHSN will help determine which locations are eligible.
2. The accuracy of estimated denominator data generated by sampling can
be heavily influenced by incorrect or missing data. Careful
implementation of data collection following the guidance in this protocol
is essential to avoid erroneous fluctuations in rates or standard infection
ratios (SIRs).
Electronic
For any location, denominator data from electronic sources (in other words,
central line days from electronic charting may be used only after a validation of a
minimum 3 consecutive months proves the data to be within 5% (+/-) of the
manually collected once-a-day counts.
When converting from one electronic counting system to another electronic
counting system, the new electronic system should be validated against manual
counts as above. If electronic counts for the new electronic system are not
within 5% of manual counts, resume manual counting and continue working with
IT staff to improve design of electronic denominator data extraction (while
reporting manual counts) until concurrent counts are within 5% for 3
consecutive months.
Notes: This guideline is important because validating a new electronic counting
system against an existing electronic system can magnify errors and result in
inaccurate denominator counts.
• Perform the validation of electronic counts separately for each location
conducting CLABSI surveillance.

January 2024 Device-associated Module
BSI
4 - 26
Data Analyses:
All data that are entered into NHSN can be analyzed at event or summary level. The data in NHSN can be
visualized and analyzed in various ways, for example, descriptive analysis reports for both the
denominator and numerator data.
Types of CLABSI Analysis Reports
Standardized Infection Ratio (SIR):
The standardized infection ratio (SIR) is calculated by dividing the number of observed events by the
number of predicted events. The number of predicted events is calculated using probabilities estimated
from statistical models constructed from national NHSN data, which represents the baseline population.
For more information on SIR and the CLABSI parameter estimates, please see the SIR guide:
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/nhsn-sir-guide.pdf
.
SIR =
(
)
(
)
While SIRs can be calculated for single locations, the measure also allows you to summarize your data
across multiple locations, adjusting for differences in the incidence of infection among the location types.
For example, you can obtain one CLABSI SIR adjusting for all locations reported. Similarly, you can obtain
one CLABSI SIR for all ICUs in your facility. In addition, IRF units within Acute Care Hospitals will be
separated from all other ACH locations.
For more information on using the CLABSI SIR reports, please see the troubleshooting guide:
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/clabsicauti_sirtroubleshooting.pdf
.
For further information regarding the p-value and 95% confidence interval, see the following guide:
https://www.cdc.gov/nhsn/ps-analysis-resources/keys-to-success.html
Note: The SIR will be calculated only if the number of predicted events (numPred) is ≥1 to help enforce a
minimum precision criterion.
Standardized Utilization Ratio (SUR):
The SUR, or standardized utilization ratio, is a summary measure used to track device use at a national,
state, local, or facility level over time. The SUR adjusts for various facility and/or location-level factors
that contribute to device use. The method of calculating an SUR is similar to the method used to calculate
the Standardized Infection Ratio (SIR), a summary statistic used in NHSN to track healthcare-associated
infections (HAIs). In device-associated HAI data analysis, the SUR compares the actual number of device
days reported to what would be predicted, given the standard population (specifically, the NHSN
baseline), adjusting for several factors that have been found to be significantly associated with differences
in device utilization.

January 2024 Device-associated Module
BSI
4 - 27
In other words, an SUR greater than 1.0 indicates that more device days were observed than predicted;
conversely, an SUR less than 1.0 indicates that fewer device days were observed than predicted. SURs are
currently calculated in NHSN for the following device types: central lines, urinary catheters, and
ventilators.
More information regarding the SUR calculations can be found at:
More information regarding the SUR calculations can be found at:
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/nhsn-sur-guide-508.pdf
https://www.cdc.gov/nhsn/pdfs/ps-analysis-resources/run-interpret-sur-reports.pdf
Rates and Ratios:
The CLABSI rate per 1000 central line days is calculated by dividing the number of CLABSIs by the number
of central line days and multiplying the result by 1000. The Central Line Utilization Ratio is calculated by
dividing the number of central line days by the number of patient days. These calculations will be
performed separately for different types of ICUs, specialty care areas, oncology units, and other locations
in the institution. Separate rates and ratios will also be calculated for different types of central lines in
specialty care areas/oncology locations and for birth weight categories in NICUs.
CLABSI Rate =
.
.
* 1000
Device Utilization Ratio
The Central Line Utilization Ratio is calculated by dividing the number of central line catheter days by the
number of patient days.
These calculations will be performed separately for the different types of ICUs, specialty care areas, and
other locations in the institution, except for neonatal locations. DURs are useful for the purposes of
tracking device use over shorter periods of time and for internal trend analyses.
DUR =
.
.
Descriptive analysis
Descriptive analysis output options of numerator and denominator data, such as line listings, frequency
tables, and bar and pie charts are available in the NHSN application. CLABSI SIRs, rates, and run charts are
also available. A line list, frequency table, and rate table are also available to analyze pathogens and
antimicrobial susceptibility data reported for CLABSIs. Guides on using NHSN analysis features are
available from: https://www.cdc.gov/nhsn/ps-analysis-resources/reference-guides.html
.
NHSN Group Analysis:
NHSN Group Users can perform the same analysis as facility level users in NHSN. A few helpful tools in
NHSN for groups are listed in the resources below. These tools are guides on how to start and join a
Group; how to create a template to request data from facilities; how to determine the level of access
granted by the facility following the previous steps, and how to analyze the facilities data.

January 2024 Device-associated Module
BSI
4 - 28
Group Analysis Resources:
NHSN Group Users Page: https://www.cdc.gov/nhsn/group-users/index.html
Group User’s Guide to the Membership Rights Report: https://www.cdc.gov/nhsn/pdfs/ps-analysis-
resources/GroupAnalysisWebinar.pdf
Group User’s Guide to the Line Listing- Participation Alerts: https://www.cdc.gov/nhsn/pdfs/ps-analysis-
resources/group-alerts.pdf
Data Quality Resources
Data Quality Website: https://www.cdc.gov/nhsn/ps-analysis-resources/data-quality/index.html
Data Quality Manual: https://www.cdc.gov/nhsn/pdfs/pscmanual/Instructions_DQ.pdf
Data Quality Training: https://www.cdc.gov/nhsn/training/analysis/index.html
Verifying BSI Events Contributing to CLABSI Numerator: https://www.cdc.gov/nhsn/pdfs/ps-analysis-
resources/bsi-excluded-linelist-508.pdf
Additional Resources
Analysis Resources: https://www.cdc.gov/nhsn/ps-analysis-resources/index.html
Analysis Reference Guides: https://www.cdc.gov/nhsn/PS-Analysis-resources/reference-guides.html
NHSN Training: https://www.cdc.gov/nhsn/training/index.html

January 2024 Device-associated Module
BSI
4 - 29
Table 8: CLABSI Measures Available in NHSN
Measure
Exclusions
Calculation
Application
CLABSI SIR
MBI-LCBIs, ECMO,
VAD, MSBP, EB,
Patient self-
injection, and Pus at
vascular site
The number of Observed CLABSIs
The number of Predicted CLABSIs
Both location
specific and
summarized
measure
MBI-LCBI
SIR
(ACH Only)
ECMO, VAD, MSBP,
EB, Patient self-
injection, and Pus at
vascular site
The number of Observed MBI LCBIs
The number of Predicted MBI LCBIs
Both location
specific and
summarized
measure
CLABSI
Rates
MBI-LCBIs, ECMO,
VAD, MSBP, EB,
Patient self-
injection, and Pus at
vascular site
× 1000
Location specific
measure only
MBI-LCBI
Rates
ECMO, VAD, MSBP,
EB, Patient self-
injection, and Pus at
vascular site
_
× 1000
Location specific
measure only
Central Line
SUR
The number of Observed Central Line Days
The number of Predicted Central Line Days
Both location
specific and
summarized
measure
DUR
Central Line Days for a location
The Patient Days for that location
Location specific
measure only

January 2024 Device-associated Module
BSI
4 - 30
References
1
CDC National and State Healthcare-Associated Infections Progress Report, published
October 2018, available at https://www.cdc.gov/hai/data/portal/progress-report.html
2
O’Grady, NP., Alexander, M., Burns, LA., Dellinger, EP., Garland, J., Heard, SO.,
Maki, DG., et al. “Guidelines for the Prevention of Intravascular Catheter-related Infections”.
Clinical Infectious Diseases 52 (a): (2011): 1087-99.
3
Boyce JM, Nadeau J, Dumigan D, Miller D, Dubowsky C, Reilly L, Hannon CV. Obtaining blood cultures by
venipuncture versus from central lines: impact on blood culture contamination rates and
potential effect on central line-associated bloodstream infection reporting. Infect Control Hosp
Epidemiol. 2013 Oct;34(10):1042-7. doi: 10.1086/673142. Epub 2013 Aug 21. PMID: 24018920.
4
Doern GV, Carroll KC, Diekema DJ, Garey KW, Rupp ME, Weinstein MP, Sexton DJ. Practical Guidance for
Clinical Microbiology Laboratories: A Comprehensive Update on the Problem of Blood Culture
Contamination and a Discussion of Methods for Addressing the Problem. Clin Microbiol Rev.
2019 Oct 30;33(1):e00009-19. doi: 10.1128/CMR.00009-19. PMID: 31666280; PMCID:
PMC6822992.
5
Lee, A., Mirrett, S., Reller, LB., Weinstein, MP. “Detection of Bloodstream Infections In
Adults: How Many Blood Cultures are Needed?” Journal of Clinical Microbiology, Nov; 45(11):
(2007): 3546-8.
6
Klevens, RM., et al. “Sampling for Collection of Central Line Day Denominators in
Surveillance for Healthcare-associated Bloodstream Infections”. Infection Control Hospital
Epidemiology. 27: (2006):338-42.
7
Thompson, ND., et al.” Evaluating the Accuracy of Sampling to Estimate Central Line–Days:
Simplification of NHSN Surveillance Methods”. Infection Control Hospital Epidemiology. 34(3):
(2013): 221-228.
8
See, I., et al. ID Week 2012 (Abstract #1284): Evaluation of Sampling Denominator Data to
Estimate Urinary Catheter- and Ventilator-Days for the NHSN. San Diego, California. October 19,
2012.

January 2024 Device-associated Module
BSI
4 - 31
Appendix: Secondary BSI Guide (not applicable to Ventilator-associated Events
[VAE])
The purpose of using the CDC/NHSN infection criteria is to identify and consistently categorize infections
that are healthcare-associated into major infection and site-specific infection types. LCBI criteria include
the caveat that organism(s) identified from the blood cannot be related to infection at another and must
be a primary BSI. One must be sure there is no other CDC/NHSN defined primary site-specific infection
that may have seeded the bloodstream secondarily; otherwise, the bloodstream infection may be
misclassified as a primary BSI and erroneously associated with the use of a central line, specifically called a
CLABSI. For locations performing in-plan VAE surveillance, refer to Figure B2
in this appendix, as well as
the VAE chapter for specific guidance on assigning a secondary BSI to a VAE. When conducting BSI
surveillance, the PNEU definitions as well as UTI, SSI and all definitions found in Chapter 17 are available
for attributing a secondary BSI for any patient in any location.
Example: A ventilated patient in an adult location where VAE surveillance is being conducted can
have a secondary BSI assigned to VAE or PNEU. A ventilated patient in a neonatal location where
in-plan PedVAP surveillance is not an option can have a secondary BSI assigned to PNEU.
Secondary BSI Scenarios: For the purposes of NHSN reporting, for a bloodstream infection to be
determined secondary to another site of infection, the following requirements must be met: *
An NHSN site-specific definition must be met; either one of the CDC/NHSN Surveillance Definitions for
Specific Types of Infections (defined in Chapter 17), or UTI, PNEU or SSI definitions.
AND
One of the following scenarios must be met:
Scenario 1: At least one organism from the blood specimen matches an organism identified from the site-
specific specimen that is used as an element to meet the NHSN site-specific infection criterion AND the
blood specimen is collected during the secondary BSI attribution period (infection window period + repeat
infection timeframe)
†
.
OR
Scenario 2: An organism identified in the blood specimen is an element that is used to meet a NHSN site-
specific infection criterion, and therefore is collected during the site-specific infection window period.
Exception to Scenarios 1 & 2: Necrotizing Enterocolitis (NEC)
The Necrotizing Enterocolitis (NEC) criteria include neither a site-specific specimen (to apply Scenario 1)
nor an organism identified from blood specimen (to apply Scenario 2)
. A BSI is considered secondary to
NEC if the patient meets one of the two NEC criterion below AND an organism identified from blood
specimen collected during the secondary BSI attribution period is an LCBI pathogen, or the same common
commensal is identified from two or more blood specimens drawn on separate occasions collected on the
same or consecutive calendar days.

January 2024 Device-associated Module
BSI
4 - 32
Necrotizing enterocolitis in infants (≤ 1 year of age) must meet one of the following criteria:
1. Infant has at least one of the clinical and one of the imaging test findings from the lists below:
At least one clinical sign:
a. bilious aspirate** (see Note)
b. vomiting
c. abdominal distention
d. occult or gross blood in stools (with no rectal fissure)
And at least one imaging test finding which if equivocal is supported by clinical correlation
(specifically, physician documentation or physician designee of antimicrobial treatment for NEC):
a. Pneumatosis intestinalis
b. Portal venous gas (Hepatobiliary gas)
c. Pneumoperitoneum
**Note: Bilious aspirate from a transpyloric feeding tube should be excluded
2. Surgical NEC: Infant has at least one of the following surgical findings:
a. surgical evidence of extensive bowel necrosis (>2 cm of bowel affected).
b. surgical evidence of pneumatosis intestinalis with or without intestinal perforation.
NEC Exception Notes:
• Pneumatosis is considered an equivocal abdominal imaging finding for Necrotizing
enterocolitis.
o Examples of abdominal imaging include KUB, ultrasound, or an abdominal x-ray.
• NEC criteria cannot be met in patients > 1 year of age. Review Gastrointestinal tract infection
(GIT) for eligibility.
Endocarditis Exception Note:
• The Endocarditis (ENDO) criteria have different rules for infection window period, RIT,
pathogen assignment and secondary BSI attribution period. (See ENDO criteria in Ch. 17).
Applying Secondary BSI Attribution Using Scenario 1 or Scenario 2
Below are examples with guidance on how to distinguish between a primary or secondary BSI. The
definition of “matching organisms”, important notes, and reporting instructions are also provided.
See Figure B1
: Secondary BSI Guide for algorithmic display of the following instructions.
Scenario 1: An organism identified from the site-specific infection is used as an element to meet the
site-specific infection criterion, AND the blood specimen contains at least one matching organism to
that site-specific specimen. The positive blood specimen must be collected during the site-specific
infection’s secondary BSI attribution period.

January 2024 Device-associated Module
BSI
4 - 33
For your convenience, a list of infection criteria that include a blood specimen with at least one
matching pathogen to the site-specific specimen that is used as an element to meet the definition are
included in Table B1
).
Example A: Patient meets NHSN criteria for a symptomatic urinary tract infection (suprapubic
tenderness and >10
5
CFU/ml of Escherichia. coli) and blood specimen collected during the
symptomatic urinary tract infection (SUTI) secondary BSI attribution period is positive for
Escherichia coli. This is a SUTI with a secondary BSI and the reported organism is Escherichia coli.
Example B: Patient meets NHSN criteria for a symptomatic urinary tract infection (suprapubic
tenderness and >10
5
CFU/ml of Escherichia coli) and blood specimen collected during the SUTI
secondary BSI attribution period grows E. coli and Pseudomonas aeruginosa. This is a SUTI with a
secondary BSI and the reported organisms are E. coli and P. aeruginosa since both site and blood
specimens are positive for at least one matching pathogen.
Example C: Patient meets NHSN criteria for a symptomatic urinary tract infection (suprapubic
tenderness and >10
5
CFU/ml of Escherichia coli) and a single blood specimen collected during the
SUTI secondary BSI attribution period is positive for E. coli and Staphylococcus epidermidis. This is
a SUTI with a secondary BSI and the reported organism is only E. coli since the single common
commensal S. epidermidis positive blood specimen does not meet BSI criteria.
Scenario 2: An organism identified from a blood specimen is an element used to meet the site-specific
infection criterion and is collected during the site-specific infection window period.
A list of site-specific infections that include a positive blood culture as an element are included in
Table B1
).
Example D: Patient becomes febrile (> 38.0 C) and complains of nausea and abdominal pain. CT
scan performed on the same day shows an intraabdominal abscess and a blood specimen
collected the same day results in the identification of Bacteroides fragilis. Because the patient
meets intraabdominal infection criterion 3b (IAB 3b), where identification of an organism from
the blood specimen is a required element, along with at least two signs and symptoms and a CT
scan showing an intraabdominal abscess, the BSI is considered secondary to an IAB 3b infection.
Example E: Patient is febrile, has a new onset of cough and has a positive chest imaging test
indicating the presence of an infiltrate. Blood specimens collected identified Pseudomonas
aeruginosa. Because the patient can meet the PNU2 definition using the identification of
organisms from a blood specimen as one of the elements of the infection criterion, and there is
an infiltrate on chest imaging test, fever, plus new onset of cough, the BSI is considered secondary
to PNEU (PNU2).
*Example F: Following a COLO procedure, on day 10 of the SSI surveillance period the patient
becomes febrile (>38.0°C) and complains of nausea and abdominal pain. A CT scan performed
indicates an abscess in the intraabdominal cavity definitive for infection. The following day
cultures are performed that showed Escherichia coli from a T-tube drainage specimen and
Bacteroides fragilis from a blood specimen. Although the organisms in the site-specific specimen
culture and blood culture do not match for at least one organism, the blood culture is considered

January 2024 Device-associated Module
BSI
4 - 34
secondary to IAB because the patient meets IAB criterion 3b with fever, nausea, and abdominal
pain. Also, the CT scan results are definitive for an intraabdominal infection, and there is an MBI
organism identified in the blood specimen . The organism identified in the blood specimen is
used as an element to meet the Organ/Space SSI site-specific infection criterion and is collected
during the SSI surveillance period. The patient also meets IAB criterion 3a with fever, nausea,
abdominal pain, and the organism (Escherichia coli) identified from the site-specific specimen
culture. Although the organism identified (Escherichia coli), differs from the organism used to
meet IAB criterion 3b (Bacteroides fragilis), the BSI is considered secondary to the organ/space SSI
IAB and both organisms (Escherichia coli and Bacteroides fragilis) would be listed as the IAB
infection pathogens.
*Example G: Patient is febrile with a new onset of cough, and has a positive chest imaging test
indicating the presence of an infiltrate. Blood and bronchoalveolar lavage (BAL) specimens are
collected that identifies Klebsiella pneumoniae > 10
4
CFU/ml from the BAL and Pseudomonas
aeruginosa from the blood. Although the organisms in the blood specimen and site-specific
specimen do not match for at least one organism, the patient can meet PNU2 using either the
identification of an organism from blood specimen or the BAL specimen as one of the elements of
the infection criterion. The positive blood culture or BAL specimen plus the infiltrate on chest
imaging test, fever, and new onset of cough are used to fully meet the PNU2 definition. The
blood culture is considered to be a secondary BSI to PNEU and both organisms are listed as PNEU
pathogens.
*In situations where an NHSN infection definition can be met using more than one criterion of the
infection definition, it is possible that identification of an organism from the blood and site-specific
specimens may not match, and a BSI may still be considered a secondary BSI.
Reporting Guidance - When Neither Scenario 1, 2, or the NEC Exception Can Be Applied:
If the organism identified from the blood specimen does not match the organism from the site-specific
specimen, and that blood specimen cannot be used to meet the site-specific infection criteria, that blood
specimen cannot be considered a secondary BSI, and in this scenario, the positive blood specimen is
considered a primary BSI.
Example 1: Patient has pustules on their abdomen along with tenderness and swelling. Purulent
material is obtained from the pustules and is positive for Streptococcus Group B. A blood
specimen collected the same day identifies methicillin resistant Staphylococcus aureus. Because
the organisms from the pustules and blood specimens do not match, and SKIN does not include a
positive blood specimen as an element, both a site-specific infection, SKIN (criterion 1 or 2a), and
a primary BSI is reported.
Example 2: A patient has an abscess in the soft tissue around a percutaneous endoscopic
gastrostomy (PEG) tube, identified by CT scan, and there is purulent drainage noted from the site.
There is no site-specific specimen collected or other sites of infection identified, however, a blood
specimen is positive for Staphylococcus aureus. Since there are no site-specific cultures collected,
ST criterion 1 is not met which means a blood specimen cannot deemed secondary. Therefore,
the positive blood specimen must be investigated as primary BSI. The patient has an ST infection
(criterion 2), and a primary BSI with the pathogen Staphylococcus aureus.

January 2024 Device-associated Module
BSI
4 - 35
Table B1: Secondary BSI Guide: List of all NHSN primary site-specific definitions
available for making secondary BSI determinations using Scenario 1 or Scenario 2
Scenario 1
Scenario 2
A positive blood specimen must contain at least one
eligible matching organism to the site-specific
specimen
Positive blood specimen must be an element of the
site-specific definition
And the blood specimen is collected in the site-
specific secondary BSI attribution period
And blood specimen is collected in the site-specific
infection window period
And an eligible organism identified from the site-
specific specimen is used as an element to meet the
site-specific definition
And an eligible organism identified in a blood
specimen is used as an element to meet the site-
specific definition
Site
Criterion
ABUTI
ABUTI
BONE
1
BRST
1
CARD
1
CIRC
2 or 3
CONJ
1a
DECU
1
DISC
1
EAR
1, 3, 5 or 7
EMET
1
ENDO
1
EYE
1
GE
2a
GIT
2a, 2b (only yeast)
IAB
1 or 3a
IC
1
JNT
1
LUNG
1
MED
1
MEN
1
ORAL
1, 3a, 3d (only
yeast)
OREP
1
PJI
1 or 3e
PNEU
2 or 3
SA
1
SINU
1
SSI
SI, DI or OS
SKIN
2a
ST
1
UMB
1a
UR
1a or 3a
USI
1
SUTI
1a, 1b or 2
VASC only as SSI
1
VCUF
3
Site
Criterion
ABUTI
ABUTI
BONE
3a
BURN
1
DISC
3a
ENDO
4a, 4b, 5a or 5b
(specific organisms)
6e or 7e plus other
criteria as listed
GIT
1b or 2c
IAB
2b or 3b
JNT
3c
MEN
2c or 3c
OREP
3a
PNEU
2 or 3
SA
3a
UMB
1b
USI
3b or 4b

January 2024 Device-associated Module
BSI
4 - 36
Secondary BSI Reporting Instructions:
• For reporting secondary BSI for possible VAP (PVAP), see Figure B2 and Chapter 10
.
• Do not report secondary bloodstream infection for vascular (VASC) infections, ventilator-
associated conditions (VAC), infection-related ventilator-associated complications (IVAC), or
pneumonia 1 (PNU1).
• When a BSI is suspected to be secondary to a lower respiratory tract infection, the BSI can be
determined secondary to VAE or PNEU definitions. (See Figure B2
).
• Site-specific organism exclusions apply to secondary BSI attribution as well.
A matching organism is defined as one of the following:
1. If genus and species are identified in both specimens, they must be the same.
a. Example: An intraabdominal specimen is used as an element to meet an IAB definition and is
growing Enterobacter cloacae. A blood specimen with a collection date in the IAB secondary
BSI attribution period is growing Enterobacter cloacae. These are considered matching
organisms.
b. Example: An intraabdominal specimen is used as an element to meet an IAB definition and is
growing Enterobacter aerogenes. A blood specimen with a collection date during the IAB
secondary BSI attribution period is growing Enterobacter cloacae. These are NOT considered
matching organisms as the species, aerogenes and cloacae, are different.
2. Organisms must at least match to the genus level and at that level the organisms must be the same.
a. Example: A surgical wound growing Pseudomonas species is used to meet deep incisional SSI
criteria and a blood specimen growing Pseudomonas aeruginosa is collected in the SSI
secondary BSI attribution period. The organisms are considered matching at the genus level,
and therefore the BSI is secondary to the SSI.
b. Example: A PCR identifying Enterococcus faecalis in CSF meets the MEN definition. A
subsequent blood culture collected in the MEN secondary BSI attribution period is identified
as Enterococcus species. The organisms are considered matching at the genus level
Enterococcus, and therefore the BSI is secondary to MEN.
3. There are two exceptions to the matching organisms definition:
a. Infections meeting LCBI 2 criterion with Staphylococcus or Streptococcus
Example (Staphylococcus): A patient has a fever and a previous chest tube site that is
reddened and swollen, and a culture is collected from the soft tissue site. A culture of the
chest tube site is positive for Staphylococcus species therefore, the ST definition is met.
The next day, two blood culture sets are collected and both blood cultures are positive for
coagulase-negative Staphylococcus. The site-specific and blood organisms are NOT
considered matching, because Staphylococcus species could be a coagulase-negative or a

January 2024 Device-associated Module
BSI
4 - 37
coagulase-positive Staphylococcus. Therefore, the BSI is not considered secondary to the
ST.
Example (Streptococcus): A patient has a fever and a previous chest tube site that is
reddened and swollen, and a culture is collected from the soft tissue site. The chest tube
site culture is reported positive for Streptococcus species therefore, the ST definition is
met. The next day, two blood culture sets are collected and both blood cultures are
positive for Streptococcus, viridans group. The site-specific and blood organisms are NOT
considered matching, because Streptococcus species could represent a Streptococcus,
viridans group or non- Streptococcus, viridans group. Therefore, the BSI is not considered
secondary to the ST.
b. In cases where an organism is identified only as “yeast” or “yeast not otherwise specified”,
the organism can be considered a match to other yeasts, when the yeast is collected during
the required timeframe, whether more fully identified or not.
Example: A tissue culture from the ulcer margin of a decubiti that reported positive for
yeast is used as an element to meet the DECU definition. A blood specimen collected in
the secondary BSI attribution period of the DECU is reported as Candida albicans. In this
example the two organisms are considered matching organisms as the organisms are
complementary (specifically, Candida is a type of yeast).
Note: This exception is limited to yeast and does not apply to identification of organisms
identified as Gram positive cocci, Gram negative rods, etc.
Yeasts isolated from non-sterile sites are commonly not identified to the genus or genus
and species level.
Example: A culture of tissue from the ulcer margin of a decubiti reported positive for a
Gram-negative rod is used as an element to meet DECU definition. A blood specimen
collected in the secondary BSI attribution period of the DECU is reported as E. coli. In this
example the two organisms are NOT considered matching organisms.
Notes:
1. Antibiograms of the blood and potential primary site isolates do not have to match.
2. If the blood specimen alone does not meet BSI criteria (for example, only one blood specimen positive
for a common commensal), that specimen may not be used to meet secondary BSI criteria (see
Scenario 1c
).

January 2024 Device-associated Module
BSI
4 - 38
Pathogen Assignment
• Additional pathogens identified from secondary BSIs, should be added to the pathogens reported for
the primary infection type. The Secondary BSI data collection field should be checked yes.
MBI-RIT Exception: An MBI-LCBI designation will not change to an LCBI event if the following
criteria are met:
1. The blood culture with the non-MBI organism is collected during an existing BSI (MBI-LCBI)
RIT
AND
2. The blood culture with the non-MBI organism is deemed secondary to an NHSN site-
specific infection
See Example 5 in the Secondary BSI Guide section of this protocol and Chapter 2
Pathogen
Assignment (Example 2b)
• If at least one BSI pathogen with a collection date in the secondary BSI attribution period matches an
organism from a specimen that was used to meet a site-specific infection criterion (either a site-
specific specimen or a blood specimen) the BSI is considered secondary to the event. However, if no
matching pathogen is identified, the subsequent BSI pathogen must be evaluated and deemed
primary or secondary to another site-specific infection.
Example: A patient with a primary UTI with Escherichia coli and a secondary BSI with Escherichia. coli
has a subsequent positive blood specimen with yeast. Yeast is an excluded pathogen for meeting UTI
criteria; therefore, the subsequent blood must be evaluated as primary or secondary to another site-
specific infection.
• A secondary BSI pathogen may be assigned to two different primary sites of infection (for example,
UTI and an IAB infection). In Example 1 below, two primary sites of infection have been identified and
a blood culture is collected within both the SUTI and the IAB secondary BSI attribution period. The
blood culture pathogen matches the pathogens for both primary sites of infection (SUTI and IAB).
Therefore, the pathogen is reported for both primary sites of infection as a secondary bloodstream
infection.

January 2024 Device-associated Module
BSI
4 - 39
Example 1: Pathogen Assignment
Hospital
Day (HD)
UTI
SBAP
UTI
RIT
UTI Infection
Window Period
IAB Infection
Window Period
IAB
RIT
IAB
SBAP
1
2
3
4
1
Urine culture:
>100,000 cfu/ml
K. pneumoniae
5
2
Fever > 38.0 C
6
3
7
4
8
5
Fever >38.0 C,
Abdominal pain
9
6
CT Scan:
Abdominal
abscess
10
7
Blood culture:
K. pneumoniae
Blood culture:
K. pneumoniae
11
8
12
9
13
10
14
11
15
12
16
13
17
14
18
19
20
21
22
23
SUTI &
Secondary BSI
DOE = HD 4
Pathogen: K.
pneumoniae
IAB & Secondary
BSI
DOE = HD 8
Pathogen: K.
pneumoniae
Secondary BSI Attribution
Period (SBAP) (Infection Window
Period + RIT)
Infection Window Period
(First positive diagnostic test, 3 days
before and 3 days after)
Date of Event (DOE)
Date the first element occurs for the
first time within the infection window
Repeat Infection Timeframe
(RIT)
(date of event = day 1)

January 2024 Device-associated Module
BSI
4 - 40
Example 2: Pathogen Assignment (continued)
Pathogens excluded from specific infection definitions (for example, yeast in UTI, or Enterococcus spp. for
PNEU) are also excluded as pathogens for BSIs secondary to that type of infection (they cannot be added
as a pathogen based on the infection type). In example 2 below, the excluded organism must be
accounted for as either 1) a primary bloodstream infection (BSI/CLABSI) or, 2) a secondary bloodstream
infection attributed to another primary infection (for example, IAB, SINU).
A blood culture with yeast and E. faecalis is collected during the SUTI RIT. A BSI secondary to a SUTI (E.
faecalis) is identified. E. faecalis is already documented as the SUTI pathogen, however, the yeast cannot
be reported as a secondary BSI pathogen, because yeasts are excluded organisms in the UTI definition.
Since there is no other primary source of infection for which the yeast BSI can be assigned as secondary, a
primary BSI with yeast is identified.
Note: The Enterococcus faecalis is not reported as a pathogen for the primary BSI because if an excluded
UTI organism, yeast, had not been identified, a primary BSI would not have been reported.

January 2024 Device-associated Module
BSI
4 - 41
Hospital
Day (HD)
UTI
SBAP
UTI
RIT
UTI Infection
Window Period
BSI Infection
Window Period
BSI
RIT
1
2
3
1
Dysuria
4
2
Urine culture:
> 100,000 cfu/ml
E. faecalis
5
3
6
4
7
5
8
6
9
7
10
8
11
9
Blood culture:
E. Faecalis /
Yeast
Blood culture:
E. faecalis /
Yeast
1
12
10
2
13
11
3
14
12
4
15
13
5
16
14
6
17
7
18
8
19
9
20
10
21
11
22
12
23
13
24
14
25
UTI & Secondary
BSI
DOE = HD 3
Pathogen: E.
faecalis
Primary BSI
DOE = HD 11
Pathogen: Yeast
Infection Window Period
(First positive diagnostic test, 3 days
before and 3 days after)
Repeat Infection Timeframe
(RIT)
(date of event = day 1)
Secondary BSI Attribution Period
(SBAP)
(Infection Window Period + RIT)
Date of Event (DOE)
Date the first element occurs for the first
time within the infection window period

January 2024 Device-associated Module
BSI
4 - 42
Example 3: Pathogen Assignment (continued)
Only one infection of a specific type (or major type: BSI, UTI and PNEU) is reported during an RIT for that
specific type of event. However, a new event of the same specific type (or major type: BSI, UTI and PNEU)
can be identified during a RIT if all required elements of the new event occur within a new IWP; the DOE
of the new event must be within the RIT of the initial event. In example 3, IAB criteria 1 is met on hospital
day 4 using organisms identified from purulent fluid. During the IAB RIT (hospital day 4-hospital day 17),
IAB criteria 3b is met (on hospital day 10) using two symptoms, positive imaging evidence of an abscess
and a positive blood specimen. Because the positive blood specimen was used to re-meet an IAB criterion
during the IAB RIT, the blood specimen is considered secondary to IAB. The pathogens, in this case, do
not have to match because another definition (IAB 3b) is fully met within a new IAB IWP (hospital day 8-
hospital day 14). Because the DOE (hospital day 10) occurs within the RIT of the initial IAB 1, a new event
is not reported. The DOE, RIT, and device association are not changed. Any additional organisms
identified (C. glabrata and L. casei) are added to the initial IAB event if reported.
Hospital
Day (HD)
IAB
SBAP
IAB
RIT
IAB Infection Window
Period
IAB Infection Window
Period
1
Admit
Abdominal pain &
distention
2
PICC
placed
3
4
US guided drainage-5L
purulent peritoneal fluid:
Klebsiella pneumoniae
and E. coli
5
6
7
8
9
10
Abdominal pain
11
CTS multiple liver
abscesses
Blood culture:
C. glabrata, L. casei
12
13
jaundice, fever
14
15
IAB 1 DOE = HD 4
Pathogens: K.
pneumoniae, E. coli
IAB 3b & Secondary BSI
DOE = HD 4
Pathogens:
C. glabrata, L. casei
Infection Window Period
(First positive diagnostic test, 3 days
before and 3 days after)
Repeat Infection Timeframe
(RIT)
(date of event = day 1)
Secondary BSI Attribution Period
(SBAP)
(Infection Window Period + RIT)
Date of Event (DOE)
Date the first element occurs for the first
time within the infection window period

January 2024 Device-associated Module
BSI
4 - 43
Example 4: Pathogen Assignment (continued)
Only one infection of a specific type (or major type for BSI, UTI and PNEU) is reported during an RIT for that
type of event. However, a new event of the same specific type (or major type for BSI, UTI and PNEU) can be
identified during an RIT if all required elements occur within a new IWP and the DOE is within the RIT of the
initial event. In example 4, GIT criterion 2c is met on hospital day-1 using two symptoms, positive imaging,
evidence of an abscess, and a positive blood specimen for Enterococcus faecalis. GIT 2a is met during the GIT
RIT (two symptoms and positive abscess). The positive blood specimen occurs within the GIT secondary BSI
attribution period and matches the organism identified from the abscess culture, Candida glabrata. Therefore,
the positive blood culture is considered secondary to the GIT infection. The pathogens, in this case, do not
have to match because another definition (GIT 2a) is fully met within a new GIT IWP (hospital day 8-hospital
day 14). Because the DOE (hospital day 11) occurs within the RIT of the initial GIT 2c, a new event is not
reported. The DOE, RIT, and device association are not changed but any additional organism identified (C.
glabrata) is added to the initial GIT event if reported. This scenario is applicable to any site-specific infection
definition from Chapter 17 or major infection type including BSI, UTI or PNEU.
Hospital
Day (HD)
GIT
SBAP
GIT RIT
GIT Infection
Window Period
GIT Infection Window
Period
1
Admit
Fever & vomiting
2
PICC
placed
3
4
CT bowel abscess
5
6
Blood culture:
Enterococcus faecalis
X2
7
8
9
10
11
Blood culture:
Candida glabrata
12
13
Abscess drainage:
Candida glabrata
Abdominal pain and
nausea
14
15
GIT-2c & Secondary
BSI DOE= HD 1
Pathogen:
E. faecalis
GIT-2a & Secondary BSI
DOE = HD 1
Pathogen: C. glabrata
Infection Window Period
(First positive diagnostic test, 3 days
before and 3 days after)
Repeat Infection Timeframe (RIT)
(date of event = day 1)
Secondary BSI Attribution Period
(SBAP)
(Infection Window Period + RIT)
Date of Event (DOE)
Date the first element occurs for the first
time within the infection window period

January 2024 Device-associated Module
BSI
4 - 44
Example 5: Pathogen Assignment (continued)
A non-MBI organism is NOT assigned to an MBI-LCBI (primary BSI) event when a blood culture with a non-
MBI organism is collected during a BSI (MBI-LCBI)-RIT and deemed secondary to an NHSN site-specific
infection. The MBI-LCBI designation will not change to an LCBI event. On day 7 of hospital admission,
Enterococcus faecalis is identified in a blood culture meeting MBI-LCBI 1 criteria. During the BSI RIT of the
Hospital
Day
RIT
Infection Window
Period
Infection Window
Period
RIT
SBAP
1
2
3
4
5
WBC –
400 cells/mm
3
6
7
1
Blood culture:
E. faecalis
8
2
9
3
10
4
WBC –
300 cells/mm
3
Erythema, Pain
1
11
5
Skin culture:
Staphylococcus aureus
2
12
6
3
13
7
4
14
8
5
15
9
6
16
10
7
17
11
8
18
12
9
19
13
Blood culture:
Staphylococcus aureus
10
20
14
11
21
12
22
13
23
14
24
25
26
MBI-LCBI 1
Date of Event = HD 7
Pathogen: E. faecalis
SKIN 2a & Secondary BSI
Date of Event = HD 10
Pathogen: Staphylococcus
aureus
Infection Window Period
(First positive diagnostic test, 3 days
before and 3 days after)
Repeat Infection Timeframe
(RIT)
(date of event = day 1)
Date of Event (DOE)
Date the first element occurs for the first
time within the infection window period
Secondary BSI Attribution
Period (SBAP)
(Infection Window Period + RIT)

January 2024 Device-associated Module
BSI
4 - 45
MBI-LCBI 1 event, a blood culture with a non-MBI organism (Staphylococcus aureus) is collected but is
deemed secondary to a SKIN 2a. Because the Staphylococcus aureus (a non-MBI organism) is secondary
to SKIN 2a, the MBI-LCBI 1 designation will not change to an LCBI 1.

January 2024 Device-associated Module
BSI
4 - 46
Figure B1: Secondary BSI Guide for eligible organisms*‡
(Not applicable to Ventilator-associated Events [VAE], See Figure B2)
*
Exception: The necrotizing enterocolitis (NEC) definition does not include criteria for a matching
site-specific specimen, nor an organism identified from a blood specimen, however an exception
for assigning a BSI secondary to NEC is provided. A BSI is considered secondary to NEC if the
patient meets one of the two NEC criteria AND an organism identified from a blood specimen,
collected during the secondary BSI attribution period, is an LCBI pathogen or the same common
commensal is identified from 2 or more blood specimens drawn on separate occasions on the
same or consecutive days.

January 2024 Device-associated Module
BSI
4 - 47
Figure B2: VAE Guidance for Secondary BSI Determination
*Secondary BSIs may be reported for possible VAP (PVAP) events, provided that at least one organism
identified from the blood specimen matches an organism identified from an appropriate respiratory tract
specimen (including respiratory secretions, pleural fluid, and lung tissue). The respiratory tract specimen
must have been collected on or after the 3rd day of mechanical ventilation and within 2 calendar days
before or after the day of onset of worsening oxygenation to be considered as a criterion for meeting the
PVAP definition. In addition, the blood specimen must have been collected during the 14-day event
period, where day 1 is the day of onset of worsening oxygenation.
• In cases where PVAP is met with only the histopathology criterion and no culture or non-culture
based testing is performed on an eligible respiratory specimen, and there is also a positive blood
specimen, a secondary BSI to VAE is not reported.
• In cases where a culture or non-culture based testing of respiratory secretions, pleural fluid, or
lung tissue is performed and does not identify an organism that matches an organism identified
from blood, a secondary BSI to VAE is not reported.
Note: Any Candida species or yeast not otherwise specified, any coagulase-negative Staphylococcus
species, and any Enterococcus species identified from blood cannot be deemed secondary to a PVAP,
unless the organism was also identified from pleural fluid or lung tissue.
