
Medicare Claims Processing Manual
Chapter 26 - Completing and Processing
Form CMS-1500 Data Set
Table of Contents
(Rev. 12671; Issued: 06-06-24)
Transmittals for Chapter 26
10 - Health Insurance Claim Form CMS-1500
10.1 - Claims That Are Incomplete or Contain Invalid Information
10.2 - Items 1-11 - Patient and Insured Information
10.3 - Items 11a - 13 - Patient and Insured Information
10.4 - Items 14-33 - Provider of Service or Supplier Information
10.5 - Place of Service Codes (POS) and Definitions
10.6 - A/B Medicare Administrative Contractor (MAC) (B) Instructions for Place
of Service (POS) Codes
10.7 - Type of Service (TOS)
10.8 - Requirements for Specialty Codes
10.8.1 - Assigning Specialty Codes by A/B MACs (B) and DME MACs
10.8.2 - Physician Specialty Codes
10.8.3 - Nonphysician Practitioner, Supplier, and Provider Specialty
Codes
10.9 - Miles/Times/Units/Services (MTUS)
10.9.1 - Methodology for Coding Number of Services, MTUS Count and
MTUS Indicator Fields
20 - Patient’s Request for Medical Payment Form CMS-1490S
30 - Printing Standards and Print File Specifications Form CMS-1500
Exhibit 1 - Form CMS-1500 (08/05) User Print File Specifications (Formerly Exhibit 2)
10 - Health Insurance Claim Form CMS-1500
(Rev. 3083, Issued: 10-02-14, Effective: CMS-1500: 01-06-14, ICD-10 - Upon
Implementation of ICD-10, Implementation: CMS-1500: 01-06-14, ICD-10 - Upon
Implementation of ICD-10)
The Administrative Simplification Compliance Act (ASCA) requires that Medicare
claims be sent electronically unless certain exceptions are met. Providers meeting an
ASCA exception may send their claims to Medicare on a paper claim form. (For more
information regarding ASCA exceptions, refer to Chapter 24.)
Providers sending professional and supplier claims to Medicare on paper must use Form
CMS-1500 in a valid version. This form is maintained by the National Uniform Claim
Committee (NUCC), an industry organization in which CMS participates. Any new
version of the form must be approved by the White House Office of Management and
Budget (OMB) before it can be used for submitting Medicare claims. When the NUCC
changes the form, CMS coordinates its review, any changes, and approval with the OMB.
The NUCC has recently changed the Form CMS-1500, and the revised form received
OMB approval on June 10, 2013. The revised form is version 02/12, OMB control
number 0938-1197.
The revised form will replace the previous version of the form 08/05, OMB control
number 0938-0999.
Throughout this chapter, the terms, “Form CMS-1500,” “Form 1500,” and “CMS-1500
claim form” may be used to describe this form depending upon the context and version.
The term, “CMS-1500 claim form” refers to the form generically, independent of a given
version.
Medicare will conduct a dual-use period during which providers can send Medicare
claims on either the old or the revised forms. When the dual-use period is over, Medicare
will accept paper claims on only the revised Form 1500, version 02/12.
For the implementation and dual-use dates, contractors shall consult the appropriate
implementation change requests for the revised Form 1500. Providers and other
interested parties may obtain the implementation dates on the CMS web site @
www.cms.gov.
Reminder: Regardless of the paper claim form version in effect: Providers cannot
submit ICD-10-CM codes for claims with dates of service prior to implementation of
ICD-10.
Medicare A/B MACS (B), DME MACS, physicians, and suppliers are responsible for
purchasing their own CMS-1500 claim forms. Forms can be obtained from printers or
printed in-house as long as they follow the specifications developed by the NUCC.
Photocopies of the CMS-1500 claim form are NOT acceptable. Medicare will accept any

type (i.e., single sheet, snap-out, continuous feed, etc.) of the CMS-1500 claim form for
processing. To purchase forms from the U.S. Government Printing Office, call (202)
512-1800.
The following instructions are required for a Medicare claim. They apply to both the
08/05 and 02/12 versions of the form except where noted. A/B MACs (B) and DME
MACs should provide information on completing the CMS-1500 claim form to all
physicians and suppliers in their area at least once a year.
These instructions represent the minimum requirements for using this form to submit a
Medicare claim. However, depending on a given Medicare policy, there may be other
data that should also be included on the CMS-1500 claim form; if so, these additional
requirements are addressed in the instructions you received for such policies (e.g., other
chapters of this manual).
Providers may use these instructions to complete this form. The CMS-1500 claim form
has space for physicians and suppliers to provide information on other health insurance.
This information can be used by A/B MACs (B) to determine whether the Medicare
patient has other coverage that must be billed prior to Medicare payment, or whether
there is another insurer to which Medicare can forward billing and payment data
following adjudication if the provider is a physician or supplier that participates in
Medicare. (See Pub. 100-05, Medicare Secondary Payer Manual, chapter 3, and chapter
28 of this manual).
Providers and suppliers must report 8-digit dates in all date of birth fields (items 3, 9b,
and 11a), and either 6-digit or 8-digit dates in all other date fields (items 11b, 12, 14, 16,
18, 19, 24a, and 31).
Providers and suppliers have the option of entering either a 6 or 8-digit date in items 11b,
14, 16, 18, 19, or 24a. However, if a provider of service or supplier chooses to enter 8-
digit dates for items 11b, 14, 16, 18, 19, or 24a, he or she must enter 8-digit dates for all
these fields. For instance, a provider of service or supplier will not be permitted to enter
8-digit dates for items 11b, 14, 16, 18, 19 and a 6-digit date for item 24a. The same
applies to providers of service and suppliers who choose to submit 6-digit dates too.
Items 12 and 31 are exempt from this requirement.
Legend
Description
MM
Month (e.g., December = 12)
DD
Day (e.g., Dec15 = 15)
YY
2 position Year (e.g., 1998 = 98)
CCYY
4 position Year (e.g., 1998 = 1998)
(MM | DD | YY) or (MM | DD | CCYY)
A space must be reported between month,
day, and year (e.g., 12 | 15 | 98 or 12 | 15 |
1998). This space is delineated by a dotted
vertical line on the Form CMS-1500)

Legend
Description
(MMDDYY) or (MMDDCCYY)
No space must be reported between month,
day, and year (e.g., 121598 or 12151998).
The date must be recorded as one
continuous number.
10.1 - Claims That are Incomplete or Contain Invalid Information
(Rev. 145, 04-23-04)
If a claim is submitted with incomplete or invalid information, it may be returned to the
submitter as unprocessable. See Chapter 1 for definitions and instructions concerning the
handling of incomplete or invalid claims.
10.2 - Items 1-11 - Patient and Insured Information
(Rev. 4232, Issued: 02-08-19, Effective: 03-12-19, Implementation: 03-12-19)
The term Medicare beneficiary identifier (Mbi) is a general term describing a
beneficiary's Medicare identification number. For purposes of this manual, Medicare
beneficiary identifier references both the Health Insurance Claim Number (HICN) and
the Medicare Beneficiary Identifier (MBI) during the new Medicare card transition
period and after for certain business areas that will continue to use the HICN as part of
their processes.
Item 1 - Shows the type of health insurance coverage applicable to this claim by the
appropriately checked box; check the Medicare box.
Item 1a - Enter the patient's Medicare beneficiary identifier whether Medicare is the
primary or secondary payer. This is a required field.
Item 2 - Enter the patient's last name, first name, and middle initial, if any, as shown on
the patient's Medicare card. This is a required field.
Item 3 - Enter the patient's 8-digit birth date (MM | DD | CCYY) and sex.
Item 4 - If there is insurance primary to Medicare, either through the patient's or spouse's
employment or any other source, list the name of the insured here. When the insured and
the patient are the same, enter the word SAME. If Medicare is primary, leave blank.
Item 5 - Enter the patient's mailing address and telephone number. On the first line enter
the street address; the second line, the city and state; the third line, the ZIP code and
phone number.
Item 6 - Check the appropriate box for patient's relationship to insured when item 4 is
completed.
Item 7 - Enter the insured's address and telephone number. When the address is the same
as the patient's, enter the word SAME. Complete this item only when items 4, 6, and 11
are completed.
Item 8 - Form version 08/05: Check the appropriate box for the patient's marital status
and whether employed or a student.
Form version 02/12: Leave blank.
Item 9 - Enter the last name, first name, and middle initial of the enrollee in a Medigap
policy if it is different from that shown in item 2. Otherwise, enter the word SAME. If
no Medigap benefits are assigned, leave blank. This field may be used in the future for
supplemental insurance plans.
NOTE: Only participating physicians and suppliers are to complete item 9 and its
subdivisions and only when the beneficiary wishes to assign his/her benefits under a
MEDIGAP policy to the participating physician or supplier.
Participating physicians and suppliers must enter information required in item 9 and its
subdivisions if requested by the beneficiary. Participating physicians/suppliers sign an
agreement with Medicare to accept assignment of Medicare benefits for all Medicare
patients. A claim for which a beneficiary elects to assign his/her benefits under a
Medigap policy to a participating physician/supplier is called a mandated Medigap
transfer. (See chapter 28.)
Medigap - Medigap policy meets the statutory definition of a "Medicare supplemental
policy" contained in §1882(g)(1) of title XVIII of the Social Security Act (the Act) and
the definition contained in the NAIC Model Regulation that is incorporated by reference
to the statute. It is a health insurance policy or other health benefit plan offered by a
private entity to those persons entitled to Medicare benefits and is specifically designed
to supplement Medicare benefits. It fills in some of the "gaps" in Medicare coverage by
providing payment for some of the charges for which Medicare does not have
responsibility due to the applicability of deductibles, coinsurance amounts, or other
limitations imposed by Medicare. It does not include limited benefit coverage available
to Medicare beneficiaries such as "specified disease" or "hospital indemnity" coverage.
Also, it explicitly excludes a policy or plan offered by an employer to employees or
former employees, as well as that offered by a labor organization to members or former
members.
Do not list other supplemental coverage in item 9 and its subdivisions at the time a
Medicare claim is filed. Other supplemental claims are forwarded automatically to the
private insurer if the private insurer contracts with the A/B MAC (B) or DME MAC to
send Medicare claim information electronically. If there is no such contract, the
beneficiary must file his/her own supplemental claim.
Item 9a - Enter the policy and/or group number of the Medigap insured preceded by
MEDIGAP, MG, or MGAP.
NOTE: Item 9d must be completed, even when the provider enters a policy and/or group
number in item 9a.
Item 9b - Form version 08/05: Enter the Medigap insured's 8-digit birth date (MM | DD |
CCYY) and sex.
Form version 02/12: Leave blank.
Item 9c - Leave blank if item 9d is completed. Otherwise, enter the claims processing
address of the Medigap insurer. Use an abbreviated street address, two-letter postal code,
and ZIP code copied from the Medigap insured's Medigap identification card. For
example:
1257 Anywhere Street
Baltimore, MD 21204
is shown as "1257 Anywhere St. MD 21204."
Item 9d - Enter the Coordination of Benefits Agreement (COBA) Medigap-based
Identifier (ID). Refer to chapter 28, section 70.6.4, of this manual for more information.
Items 10a through 10c - Check "YES" or "NO" to indicate whether employment, auto
liability, or other accident involvement applies to one or more of the services described in
item 24. Enter the State postal code. Any item checked "YES" indicates there may be
other insurance primary to Medicare. Identify primary insurance information in item 11.
Item 10d - Use this item exclusively for Medicaid (MCD) information. If the patient is
entitled to Medicaid, enter the patient's Medicaid number preceded by MCD.
Item 11 - THIS ITEM MUST BE COMPLETED, IT IS A REQUIRED FIELD. BY
COMPLETING THIS ITEM, THE PHYSICIAN/SUPPLIER ACKNOWLEDGES
HAVING MADE A GOOD FAITH EFFORT TO DETERMINE WHETHER
MEDICARE IS THE PRIMARY OR SECONDARY PAYER.
If there is insurance primary to Medicare, enter the insured's policy or group number and
proceed to items 11a - 11c. Items 4, 6, and 7 must also be completed.
NOTE: Enter the appropriate information in item 11c if insurance primary to Medicare
is indicated in item 11.
If there is no insurance primary to Medicare, enter the word "NONE" and proceed to item
12.
If the insured reports a terminating event with regard to insurance which had been
primary to Medicare (e.g., insured retired), enter the word "NONE" and proceed to item
11b.
If a lab has collected previously and retained Medicare Secondary Payer (MSP)
information for a beneficiary, the lab may use that information for billing purposes of the
non-face-to-face lab service. If the lab has no MSP information for the beneficiary, the
lab will enter the word “None” in Block 11, when submitting a claim for payment of a
reference lab service. Where there has been no face-to-face encounter with the
beneficiary, the claim will then follow the normal claims process. When a lab has a face-
to-face encounter with a beneficiary, the lab is expected to collect the MSP information
and bill accordingly.
Insurance Primary to Medicare - Circumstances under which Medicare payment may
be secondary to other insurance include:
• Group Health Plan Coverage
o Working Aged;
o Disability (Large Group Health Plan); and
o End Stage Renal Disease;
• No Fault and/or Other Liability; and
• Work-Related Illness/Injury:
o Workers' Compensation;
o Black Lung; and
o Veterans Benefits.
NOTE: For a paper claim to be considered for MSP benefits, a copy of the primary
payer's explanation of benefits (EOB) notice must be forwarded along with the claim
form. (See Pub. 100-05, Medicare Secondary Payer Manual, chapter 3.)
10.3 - Items 11a - 13 - Patient and Insured Information
(Rev. 3083, Issued: 10-02-14, Effective: CMS-1500: 01-06-14, ICD-10 – Upon
Implementation of ICD-10, Implementation: CMS-1500: 01-06-14, ICD-10 - Upon
Implementation of ICD-10)
Item 11a - Enter the insured's 8-digit birth date (MM | DD | CCYY) and sex if different
from item 3.
Item 11b - Form version 08/05: Enter employer's name, if applicable. If there is a
change in the insured's insurance status, e.g., retired, enter either a 6-digit (MM | DD |
YY) or 8-digit (MM | DD | CCYY) retirement date preceded by the word, "RETIRED."
Form version 02/12: provide this information to the right of the vertical dotted line.
Item 11c - Enter the 9-digit PAYERID number of the primary insurer. If no PAYERID
number exists, then enter the complete primary payer's program or plan name. If the
primary payer's EOB does not contain the claims processing address, record the primary
payer's claims processing address directly on the EOB. This is required if there is
insurance primary to Medicare that is indicated in item 11.
Item 11d - Leave blank. Not required by Medicare.
Item 12 - The patient or authorized representative must sign and enter either a 6-digit
date (MM | DD | YY), 8-digit date (MM | DD | CCYY), or an alpha-numeric date (e.g.,
January 1, 1998) unless the signature is on file. In lieu of signing the claim, the patient
may sign a statement to be retained in the provider, physician, or supplier file in
accordance with Chapter 1, “General Billing Requirements.” If the patient is physically
or mentally unable to sign, a representative specified in chapter 1, may sign on the
patient's behalf. In this event, the statement's signature line must indicate the patient's
name followed by “by” the representative's name, relationship to the patient, and the
reason the patient cannot sign. The authorization is effective indefinitely unless the
patient or the patient's representative revokes this arrangement.
NOTE: This can be "Signature on File" and/or a computer generated signature.
The patient's signature authorizes release of medical information necessary to process the
claim. It also authorizes payment of benefits to the provider of service or supplier when
the provider of service or supplier accepts assignment on the claim.
Signature by Mark (X) - When an illiterate or physically handicapped enrollee signs by
mark, a witness must enter his/her name and address next to the mark.
Item 13 - The patient’s signature or the statement “signature on file” in this item
authorizes payment of medical benefits to the physician or supplier. The patient or
his/her authorized representative signs this item or the signature must be on file
separately with the provider as an authorization. However, note that when payment
under the Act can only be made on an assignment-related basis or when payment is for
services furnished by a participating physician or supplier, a patient’s signature or a
“signature on file” is not required in order for Medicare payment to be made directly to
the physician or supplier.
The presence of or lack of a signature or “signature on file” in this field will be indicated
as such to any downstream coordination of benefits trading partners (supplemental
insurers) with whom CMS has a payer-to-payer coordination of benefits relationship.
Medicare has no control over how supplemental claims are processed, so it is important
that providers accurately address this field as it may affect supplemental payments to
providers and/or their patients.

In addition, the signature in this item authorizes payment of mandated Medigap benefits
to the participating physician or supplier if required Medigap information is included in
item 9 and its subdivisions. The patient or his/her authorized representative signs this
item or the signature must be on file as a separate Medigap authorization. The Medigap
assignment on file in the participating provider of service/supplier's office must be
insurer specific. It may state that the authorization applies to all occasions of service
until it is revoked.
NOTE: This can be "Signature on File" signature and/or a computer generated signature.
10.4 - Items 14-33 - Provider of Service or Supplier Information
(Rev.10341, Issued: 09-04-2020; Effective: 10-06-20; Implementation: 10- 06-20)
Reminder: For date fields other than date of birth, all fields shall be one or the
other format, 6-digit: (MM | DD | YY) or 8-digit: (MM | DD | CCYY). Intermixing
the two formats on the claim is not allowed.
Item 14 - Enter either an 8-digit (MM | DD | CCYY) or 6-digit (MM | DD | YY) date of
current illness, injury, or pregnancy. For chiropractic services, enter an 8-digit (MM |
DD | CCYY) or 6-digit (MM | DD | YY) date of the initiation of the course of treatment
and enter an 8-digit (MM | DD | CCYY) or 6-digit (MM | DD | YY) date in item 19.
Additional information for form version 02/12: Although this version of the form
includes space for a qualifier, Medicare does not use this information; do not enter a
qualifier in item 14.
Item 15 - Leave blank.
Item 16 - If the patient is employed and is unable to work in his/her current occupation,
enter an 8-digit (MM | DD | CCYY) or 6-digit (MM | DD | YY) date when patient is
unable to work. An entry in this field may indicate employment related insurance
coverage.
Item 17 - Enter the name of the referring or ordering physician if the service or item was
ordered or referred by a physician. All physicians who order services or refer Medicare
beneficiaries must report this data. Similarly, if Medicare policy requires you to report a
supervising physician, enter this information in item 17. When a claim involves multiple
referring, ordering, or supervising physicians, use a separate CMS-1500 claim form for
each ordering, referring, or supervising physician.
Additional instructions for form version 02/12: Enter one of the following qualifiers as
appropriate to identify the role that this physician (or non-physician practitioner) is
performing:
Qualifier
Provider Role
DN
Referring Provider

Qualifier
Provider Role
DK
Ordering Provider
DQ
Supervising Provider
Enter the qualifier to the left of the dotted vertical line on item 17.
NOTE: Under certain circumstances, Medicare permits a non-physician practitioner to
perform these roles. Refer to Pub 100-02, Medicare Benefit Policy Manual, chapter 15
for non-physician practitioner rules. Enter non-physician practitioner information
according to the rules above for physicians.
The term "physician" when used within the meaning of §1861(r) of the Act and used in
connection with performing any function or action refers to:
1. A doctor of medicine or osteopathy legally authorized to practice medicine and
surgery by the State in which he/she performs such function or action;
2. A doctor of dental surgery or dental medicine who is legally authorized to practice
dentistry by the State in which he/she performs such functions and who is acting
within the scope of his/her license when performing such functions;
3. A doctor of podiatric medicine for purposes of §§(k), (m), (p)(1), and (s) and
§§1814(a), 1832(a)(2)(F)(ii), and 1835 of the Act, but only with respect to functions
which he/she is legally authorized to perform as such by the State in which he/she
performs them;
4. A doctor of optometry, but only with respect to the provision of items or services
described in §1861(s) of the Act which he/she is legally authorized to perform as a
doctor of optometry by the State in which he/she performs them; or
5. A chiropractor who is licensed as such by a State (or in a State which does not
license chiropractors as such), and is legally authorized to perform the services of a
chiropractor in the jurisdiction in which he/she performs such services, and who
meets uniform minimum standards specified by the Secretary, but only for purposes
of §§1861(s)(1) and 1861(s)(2)(A) of the Act, and only with respect to treatment by
means of manual manipulation of the spine (to correct a subluxation). For the
purposes of §1862(a)(4) of the Act and subject to the limitations and conditions
provided above, chiropractor includes a doctor of one of the arts specified in the
statute and legally authorized to practice such art in the country in which the inpatient
hospital services (referred to in §1862(a)(4) of the Act) are furnished.
Referring physician - is a physician who requests an item or service for the beneficiary
for which payment may be made under the Medicare program.
Ordering physician - is a physician or, when appropriate, a non-physician practitioner
who orders non-physician services for the patient. See Pub. 100-02, Medicare Benefit
Policy Manual, chapter 15 for non-physician practitioner rules. Examples of services that
might be ordered include diagnostic laboratory tests, clinical laboratory tests,
pharmaceutical services, durable medical equipment, and services incident to that
physician’s or non-physician practitioner’s service.
The ordering/referring requirement became effective January 1, 1992, and is required by
§1833(q) of the Act. All claims for Medicare covered services and items that are the
result of a physician's order or referral shall include the ordering/referring physician's
name. The following services/situations require the submission of the referring/ordering
provider information:
• Medicare covered services and items that are the result of a physician's order
or referral;
• Parenteral and enteral nutrition;
• Immunosuppressive drug claims;
• Hepatitis B claims;
• Diagnostic laboratory services;
• Diagnostic radiology services;
• Portable x-ray services;
• Consultative services;
• Durable medical equipment;
• When the ordering physician is also the performing physician (as often is the
case with in-office clinical laboratory tests);
• When a service is incident to the service of a physician or non-physician
practitioner, the name of the physician or non-physician practitioner who
performs the initial service and orders the non-physician service must appear in
item 17;
• When a physician extender or other limited licensed practitioner refers a patient
for consultative service, submit the name of the physician who is supervising the
limited licensed practitioner;
• Effective for claims with dates of service on or after October 1, 2012, all claims
for physical therapy, occupational therapy, or speech-language pathology
services, including those furnished incident to a physician or nonphysician
practitioner, require that the name and NPI of the certifying physician or

nonphysician practitioner of the therapy plan of care be entered as the referring
physician in Items 17 and 17b.
Item 17a - Leave blank.
Item 17b - Enter the NPI of the referring, ordering, or supervising physician or non-
physician practitioner listed in item 17. All physicians and non-physician practitioners
who order services or refer Medicare beneficiaries must report this data.
NOTE: Effective May 23, 2008, 17a is not to be reported but 17b MUST be reported
when a service was ordered or referred by a physician.
Item 18 - Enter either an 8-digit (MM | DD | CCYY) or a 6-digit (MM | DD | YY) date
when a medical service is furnished as a result of, or subsequent to, a related
hospitalization.
Item 19 - Enter either a 6-digit (MM | DD | YY) or an 8-digit (MM | DD | CCYY) date
patient was last seen and the NPI of his/her attending physician when a physician
providing routine foot care submits claims.
NOTE: Effective May 23, 2008, all provider identifiers submitted on the CMS-1500
claim form MUST be in the form of an NPI.
Enter either a 6-digit (MM | DD | YY) or an 8-digit (MM | DD | CCYY) x-ray date for
chiropractor services (if an x-ray, rather than a physical examination was the method used
to demonstrate the subluxation). By entering an x-ray date and the initiation date for
course of chiropractic treatment in item 14, the chiropractor is certifying that all the
relevant information requirements (including level of subluxation) of Pub. 100-02,
Medicare Benefit Policy Manual, chapter 15, is on file, along with the appropriate x-ray
and all are available for A/B MAC (B) review.
Instructions for Not Otherwise Classified (NOC) Codes – Any unlisted services or
procedure code. Note: When reporting NOC codes, this field must be populated as
specified below.
Enter the drug's name and dosage when submitting a claim for NOC drugs.
Enter a concise description of an "unlisted procedure code" or a NOC code if one can be
given within the confines of this box. Otherwise an attachment shall be submitted with
the claim.
When billing for unlisted laboratory tests using a NOC code, this field MUST include the
specific name of the laboratory test(s) and/or a short descriptor of the test(s). Claims for
unlisted laboratory tests that are received without this information shall be treated
according to the requirements found in Pub. 100-04, Medicare Claims Processing
Manual, Chapter 1, Section 80.3.2 and “returned as unprocessable.” Section 216(a) of the
Protecting Access to Medicare Act of 2014 (PAMA) requires reporting entities to report
private payor payment rates for laboratory tests and the corresponding volumes of
tests. In compliance with PAMA, CMS must collect private payor data on unique tests
currently being paid as a NOC code, Not Otherwise Specified (NOS) code, or unlisted
service or procedure code.
Enter all applicable modifiers when modifier -99 (multiple modifiers) is entered in item
24d. If modifier -99 is entered on multiple line items of a single claim form, all
applicable modifiers for each line item containing a -99 modifier should be listed as
follows: 1=(mod), where the number 1 represents the line item and "mod" represents all
modifiers applicable to the referenced line item.
Enter the statement "Homebound" when an independent laboratory obtains a specimen
from a homebound or institutionalized patient. (See Pub. 100-02, Medicare Benefit
Policy Manual, Chapter 15, "Covered Medical and Other Health Services," and Pub. 100-
04, Medicare Claims Processing Manual, Chapter 16, "Laboratory Services,” and Pub.
100-01, Medicare General Information, Eligibility, and Entitlement Manual, Chapter 5,
"Definitions," respectively, for the definition of "homebound" and a more complete
definition of a medically necessary laboratory service to a homebound or an institutional
patient.)
Enter the statement, "Patient refuses to assign benefits," when the beneficiary absolutely
refuses to assign benefits to a non-participating physician/supplier who accepts
assignment on a claim. In this case, payment can only be made directly to the
beneficiary.
Enter the statement, "Testing for hearing aid" when billing services involving the testing
of a hearing aid(s) is used to obtain intentional denials when other payers are involved.
When dental examinations are billed, enter the specific surgery for which the exam is
being performed.
Enter the specific name and dosage amount when low osmolar contrast material is billed,
but only if HCPCS codes do not cover them.
Enter a 6-digit (MM | DD | YY) or an 8-digit (MM | DD | CCYY) assumed and/or
relinquished date for a global surgery claim when providers share post-operative care.
Enter demonstration ID number "30" for all national emphysema treatment trial claims.
Enter demonstration ID number “56” for all national Laboratory Affordable Care Act
Section 113 Demonstration Claims.
Enter the NPI of the physician who is performing the technical or professional
component of a diagnostic test that is subject to the anti-markup payment limitation. (See
Pub. 100-04, chapter 1, section 30.2.9 for additional information.)
NOTE: Effective May 23, 2008, all provider identifiers submitted on the CMS-1500
claim form MUST be in the form of an NPI.
Method II suppliers shall enter the most current HCT value for the injection of Aranesp
for ESRD beneficiaries on dialysis. (See Pub. 100-04, chapter 8, section 60.7.2.)
Individuals and entities who bill A/B MACs (B) for administrations of ESAs or Part B
anti-anemia drugs not self-administered (other than ESAs) in the treatment of cancer
must enter the most current hemoglobin or hematocrit test results. The test results shall
be entered as follows: TR= test results (backslash), R1=hemoglobin, or R2=hematocrit
(backslash), and the most current numeric test result figure up to 3 numerics and a
decimal point [xx.x]). Example for hemoglobin tests: TR/R1/9.0, Example for
Hematocrit tests: TR/R2/27.0.
Item 20 - Complete this item when billing for diagnostic tests subject to the anti-markup
payment limitation. Enter the acquisition price under charges if the "yes" block is
checked. A "yes" check indicates that an entity other than the entity billing for the
service performed the diagnostic test. A "no" check indicates "no anti-markup tests are
included on the claim." When "yes" is annotated, item 32 shall be completed. When
billing for multiple anti-markup tests, each test shall be submitted on a separate claim
form CMS-1500. Multiple anti-markup tests may be submitted on the ASC X12 837
electronic format as long as appropriate line level information is submitted when services
are rendered at different service facility locations. See chapter 1.
NOTE: This is a required field when billing for diagnostic tests subject to the anti-
markup payment limitation.
Item 21 - Enter the patient's diagnosis/condition. With the exception of claims submitted
by ambulance suppliers (specialty type 59), all physician and nonphysician specialties
(i.e., PA, NP, CNS, CRNA) use diagnosis codes to the highest level of specificity for the
date of service. Enter the diagnoses in priority order. All narrative diagnoses for
nonphysician specialties shall be submitted on an attachment.
Reminder: Do not report ICD-10-CM codes for claims with dates of service prior to
implementation of ICD-10-CM, on either the old or revised version of the CMS-1500
claim form.
For form version 08/05, report a valid ICD-9-CM code. Enter up to four diagnosis codes.
For form version 02/12, it may be appropriate to report either ICD-9-CM or ICD-10-CM
codes depending upon the dates of service (i.e., according to the effective dates of the
given code set).
• The “ICD Indicator” identifies the ICD code set being reported. Enter the
applicable ICD indicator according to the following:

Indicator
Code Set
9
ICD-9-CM diagnosis
0
ICD-10-CM diagnosis
Enter the indicator as a single digit between the vertical, dotted lines.
• Do not report both ICD-9-CM and ICD-10-CM codes on the same claim form. If
there are services you wish to report that occurred on dates when ICD-9-CM
codes were in effect, and others that occurred on dates when ICD-10-CM codes
were in effect, then send separate claims such that you report only ICD-9-CM or
only ICD-10-CM codes on the claim. (See special considerations for spans of
dates below.)
• If you are submitting a claim with a span of dates for a service, use the “from”
date to determine which ICD code set to use.
• Enter up to 12 diagnosis codes. Note that this information appears opposite lines
with letters A-L. Relate lines A- L to the lines of service in 24E by the letter of
the line. Use the highest level of specificity. Do not provide narrative description
in this field.
• Do not insert a period in the ICD-9-CM or ICD-10-CM code.
Item 22 - Leave blank. Not required by Medicare.
Item 23 - Enter the Quality Improvement Organization (QIO) prior authorization number
for those procedures requiring QIO prior approval.
Enter the Investigational Device Exemption (IDE) number when an investigational
device is used in an FDA-approved clinical trial. Post Market Approval number should
also be placed here when applicable.
For physicians performing care plan oversight services, enter the NPI of the home health
agency (HHA) or hospice when CPT code G0181 (HH) or G0182 (Hospice) is billed.
Enter the 10-digit Clinical Laboratory Improvement Act (CLIA) certification number for
laboratory services billed by an entity performing CLIA covered procedures.
For ambulance claims, enter the ZIP code of the loaded ambulance trip’s point-of-pickup.
NOTE: Item 23 can contain only one condition. Any additional conditions should be
reported on a separate CMS-1500 claim form.
Item 24 - The six service lines in section 24 have been divided horizontally to
accommodate submission of supplemental information to support the billed service. The
top portion in each of the six service lines is shaded and is the location for reporting
supplemental information. It is not intended to allow the billing of 12 service lines.
When required to submit NDC drug and quantity information for Medicaid rebates,
submit the NDC code in the red shaded portion of the detail line item in positions 01
through position 13. The NDC is to be preceded with the qualifier N4 and followed
immediately by the 11 digit NDC code (e.g. N499999999999). Report the NDC quantity
in positions 17 through 24 of the same red shaded portion. The quantity is to be preceded
by the appropriate qualifier: UN (units), F2 (international units), GR (gram) or ML
(milliliter). There are six bytes available for quantity. If the quantity is less than six
bytes, left justify and space-fill the remaining positions (e.g., UN2 or F2999999).
Item 24A - Enter a 6-digit or 8-digit (MMDDCCYY) date for each procedure, service, or
supply. When "from" and "to" dates are shown for a series of identical services, enter the
number of days or units in column G. This is a required field. Return as unprocessable if
a date of service extends more than 1 day, and a valid "to" date is not present.
Item 24B - Enter the appropriate place of service code(s) from the list provided in section
10.5. Identify the setting, using a place of service code, for each item used or service
performed. This is a required field.
NOTE: When a service is rendered to a patient who is a registered inpatient or an
outpatient (off campus or on campus) of a hospital, use the inpatient hospital POS code
21, Off Campus-Outpatient Hospital POS code 19, or On Campus-Outpatient Hospital
POS code 22, respectively, as discussed in section 10.5 of this chapter.
Item 24C - Medicare providers are not required to complete this item.
Item 24D - Enter the procedures, services, or supplies using the CMS Healthcare
Common Procedure Coding System (HCPCS) code. When applicable, show HCPCS
code modifiers with the HCPCS code. The CMS-1500 claim form has the capacity to
capture up to four modifiers.
Enter the specific procedure code without a narrative description. However, when
reporting an "unlisted procedure code" or a "not otherwise classified" (NOC) code,
include a narrative description in item 19 if a coherent description can be given within the
confines of that box. Otherwise, an attachment shall be submitted with the claim. This is
a required field.
Return as unprocessable if an "unlisted procedure code" or a NOC code is indicated in
item 24d, but an accompanying narrative is not present in item 19 or on an attachment.
Item 24E - This is a required field. Enter the diagnosis code reference number or letter
(as appropriate, per form version) as shown in item 21 to relate the date of service and the
procedures performed to the primary diagnosis. Enter only one reference number/letter
per line item. When multiple services are performed, enter the primary reference
number/letter for each service.
When using form version 08/05, this reference will be either a 1, or a 2, or a 3, or a 4.
When using form version 02/12, the reference to supply in 24E will be a letter from A-L.
Otherwise, the instructions above apply.
If a situation arises where two or more diagnoses are required for a procedure code (e.g.,
pap smears), the provider shall reference only one of the diagnoses in item 21.
Item 24F- Enter the charge for each listed service.
Item 24G - Enter the number of days or units. This field is most commonly used for
multiple visits, units of supplies, anesthesia minutes, or oxygen volume. If only one
service is performed, the numeral 1 must be entered.
Some services require that the actual number or quantity billed be clearly indicated on the
claim form (e.g., multiple ostomy or urinary supplies, medication dosages, or allergy
testing procedures). When multiple services are provided, enter the actual number
provided.
For anesthesia, show the elapsed time (minutes) in item 24g. Convert hours into minutes
and enter the total minutes required for this procedure.
For instructions on submitting units for oxygen claims, see chapter 20, section 130.6 of
this manual.
Beginning with dates of service on and after January 1, 2011, for ambulance mileage,
enter the number of loaded miles traveled rounded up to the nearest tenth of a mile up to
100 miles. For mileage totaling 100 miles and greater, enter the number of covered miles
rounded up to the nearest whole number miles. If the total mileage is less than 1 whole
mile, enter a “0” before the decimal (e.g. 0.9). See Pub. 100-04, chapter 15, §20.2 for
more information on loaded mileage and §30.1.2 for more information on reporting
fractional mileage.
NOTE: This field should contain an appropriate numerical value. The A/B MAC (B)
should program their system to automatically default "1" unit when the information in
this field is missing to avoid returning as unprocessable, except on claims for ambulance
mileage. For ambulance mileage claims, contractors shall automatically default “0.1”
unit when total mileage units are missing in this field.
Item 24H - Leave blank. Not required by Medicare.
Item 24I - Leave Blank. Not required by Medicare.
Item 24J - Enter the rendering provider’s NPI number in the lower unshaded portion. In
the case of a service provided incident to the service of a physician or non-physician
practitioner, when the person who ordered the service is not supervising, enter the NPI of
the supervisor in the lower unshaded portion.
This unprocessable instruction does not apply to influenza virus and pneumococcal
vaccine claims submitted on roster bills as they do not require a rendering provider NPI.
NOTE: Effective May 23, 2008, the shaded portion of 24J is not to be reported.
Item 25 - Enter the provider of service or supplier Federal Tax ID (Employer
Identification Number or Social Security Number) and check the appropriate check box.
Medicare providers are not required to complete this item for crossover purposes since
the Medicare contractor will retrieve the tax identification information from their internal
provider file for inclusion on the COB outbound claim. However, tax identification
information is used in the determination of accurate National Provider Identifier
reimbursement. Reimbursement of claims submitted without tax identification
information will/may be delayed.
Item 26 - Enter the patient's account number assigned by the provider's of service or
supplier's accounting system. This field is optional to assist the provider in patient
identification. As a service, any account numbers entered here will be returned to the
provider.
Item 27 - Check the appropriate block to indicate whether the provider of service or
supplier accepts assignment of Medicare benefits. If Medigap is indicated in item 9 and
Medigap payment authorization is given in item 13, the provider of service or supplier
shall also be a Medicare participating provider of service or supplier and accept
assignment of Medicare benefits for all covered charges for all patients.
The following providers of service/suppliers and claims can only be paid on an
assignment basis:
• Clinical diagnostic laboratory services;
• Physician services to individuals dually entitled to Medicare and Medicaid;
• Participating physician/supplier services;
• Services of physician assistants, nurse practitioners, clinical nurse specialists,
nurse midwives, certified registered nurse anesthetists, clinical psychologists, and
clinical social workers;
• Ambulatory surgical center services for covered ASC procedures;
• Home dialysis supplies and equipment paid under Method II;
• Ambulance services;
• Drugs and biologicals; and
• Simplified Billing Roster for influenza virus vaccine and pneumococcal vaccine.
Item 28 - Enter total charges for the services (i.e., total of all charges in item 24f).
Item 29 - Enter the total amount the patient paid on the covered services only.
Item 30 - Leave blank. Not required by Medicare.
Item 31 - Enter the signature of provider of service or supplier, or his/her representative,
and either the 6-digit date (MM | DD | YY), 8-digit date (MM | DD | CCYY), or alpha-
numeric date (e.g., January 1, 1998) the form was signed.
In the case of a service that is provided incident to the service of a physician or non-
physician practitioner, when the ordering physician or non-physician practitioner is
directly supervising the service as in 42 CFR 410.32, the signature of the ordering
physician or non-physician practitioner shall be entered in item 31. When the ordering
physician or non-physician practitioner is not supervising the service, then enter the
signature of the physician or non-physician practitioner providing the direct supervision
in item 31.
NOTE: This is a required field; however, the claim can be processed if the following is
true: if a physician, supplier, or authorized person's signature is missing, but the
signature is on file; or if any authorization is attached to the claim or if the signature field
has "Signature on File" and/or a computer generated signature.
Item 32 - For services payable under the physician fee schedule and anesthesia services,
enter the name and address, and ZIP code of the facility if the services were furnished in
a hospital, clinic, laboratory, or facility other than the patient's home or physician's office.
Effective for claims received on or after April 1, 2004, enter the name, address, and ZIP
code of the service location for all services other than those furnished in place of service
home - 12. Effective for claims received on or after April 1, 2004, only one name,
address and ZIP code may be entered in the block. If additional entries are needed,
separate claim forms shall be submitted. Effective January 1, 2011, for claims processed
on or after January 1, 2011, submission of the location where the service was rendered
will be required for all POS codes.
Providers of service (namely physicians) shall identify the supplier's name, address, and
ZIP code when billing for anti-markup tests. When more than one supplier is used, a
separate CMS-1500 claim form shall be used to bill for each supplier. (See Pub. 100-04,
chapter 1, §10.1.1.2 for more information on payment jurisdiction for claims subject to
the anti-markup limitation.)
For foreign claims, only the enrollee can file for Part B benefits rendered outside of the
United States. These claims will not include a valid ZIP code. When a claim is received
for these services on a beneficiary submitted Form CMS-1490S, before the claim is
entered in the system, it should be determined if it is a foreign claim. If it is a foreign
claim, follow instructions in chapter 1 for disposition of the claim. The A/B MAC (B)
processing the foreign claim will have to make necessary accommodations to verify that
the claim is not returned as unprocessable due to the lack of a ZIP code.
For durable medical, orthotic, and prosthetic claims, the name and address of the location
where the order was accepted must be entered (DME MAC only). This field is required.
When more than one supplier is used, a separate CMS-1500 claim form shall be used to
bill for each supplier. This item is completed whether the supplier's personnel performs
the work at the physician's office or at another location.
If the supplier is a certified mammography screening center, enter the 6-digit FDA
approved certification number.
Complete this item for all laboratory work performed outside a physician's office. If an
independent laboratory is billing, enter the place where the test was performed.
Item 32a - If required by Medicare claims processing policy, enter the NPI of the service
facility.
Effective for claims submitted with a receipt date on and after October 1, 2015, the
billing physician or supplier must report the name, address, and NPI of the performing
physician or supplier on the claim on reference laboratory claims, even if the performing
physician or supplier is enrolled in a different A/B MAC (B) jurisdiction. See Pub. 100-
04, Chapter 1, §10.1.1 for more information regarding claims filing jurisdiction.
Item 32b - Effective May 23, 2008, Item 32b is not to be reported.
Item 33 - Enter the provider of service/supplier's billing name, address, ZIP code, and
telephone number. This is a required field.
Item 33a - Enter the NPI of the billing provider or group. This is a required field.
Item 33b - Item 33b is not generally reported. However, for some Medicare policies you
may be instructed to use this item; direction as to how to use this item will be in the
instructions you received regarding the specific policy, if applicable.
10.5 - Place of Service Codes (POS) and Definitions
(Rev. 12671, Issued: 06-06-24, Effective: 01-01-24, Implementation Date: 07-08-24)
o
HIPAA
o
The Health Insurance Portability and Accountability Act of 1996
(HIPAA) became effective October 16, 2003, for all covered entities.
Medicare is a covered entity under HIPAA.
o
The final rule, “Health Insurance Reform: Standards for Electronic
Transactions,” published in the Federal Register, August 17, 2000,
adopts the standards to be used under HIPAA and names the
implementation guides to be used for these standards. The ASC X12N
837 professional is the standard to be used for transmitting health care
claims electronically, and its implementation guide requires the use of
POS codes from the National POS code set, currently maintained by
CMS.
o
As a covered entity, Medicare must use the POS codes from the
National POS code set for processing its electronically submitted
claims. Medicare must also recognize as valid POS codes from the POS
code set when these codes appear on such a claim.
o
Medicare must recognize and accept POS codes from the
national POS code set in terms of HIPAA compliance. Note
special considerations for Homeless Shelter (code 04), Indian
Health Service (codes 05, 06), Tribal 638 (codes 07, 08), and
09 Prison/Correctional Facility settings, describe below.
Where there is no national policy for a given POS code, local
contractors may work with their medical directors to develop
local policy regarding the services payable in a given setting,
and this could include creating a crosswalk to an existing
setting if desired. However, local contractors must pay for the
services at either the facility or the nonfacility rate as
designated below. In addition, local contractors, when
developing policy, must ensure that they continue to pay
appropriate rates for services rendered in the new setting; if
they choose to create a crosswalk from one setting to another,
they must crosswalk a facility rate designated code to another
facility rate designated code, and a nonfacility rate designated
code to another nonfacility rate designated code. For
previously issued POS codes for which a crosswalk was
mandated, and for which no other national Medicare directive
has been issued, local contractors may elect to continue to use
the crosswalk or develop local policy regarding the services
payable in the setting, including another crosswalk, if
appropriate. If a local contractor develops local policy for
these settings, but later receives specific national instructions
for these codes, the local contractors shall defer to and
comply with the newer instructions. (Note: While, effective
January 1, 2003, codes 03 School, 04 Homeless Shelter, and

20 Urgent Care became part of the National POS code set and
were to be crosswalked to 11 Office, this mandate to
crosswalk has since been lifted, as indicated above).
o
National policy in the form of “Special Considerations” for
Off Campus- Outpatient Hospital (POS 19), Inpatient
Hospital (POS code 21), On Campus-Outpatient Hospital
(POS code 22), Ambulatory Surgical Center (POS code 24)
and Hospice (POS code 34) are included below.
• The National POS Code Set and Instructions for Using It
The following is the current national POS code set, with facility and
nonfacility designations noted for Medicare payment for services on
the Physician Fee Schedule. As a new POS code is established, the
health care industry is permitted to use this code from the date that it
is posted on the Medicare Place of Service Code Set Web page at
http://www.cms.gov/Medicare/Coding/place-of-service-
codes/Place_of_Service_Code_Set.html which is typically expected to
be some months ahead of the final effective date for Medicare use.
The code set is annotated with the effective dates for this and all
other codes added on and after January 1, 2003. Codes without
effective dates annotated are long-standing and in effect on and
before January 1, 2003.
POS Code and Name (effective date)
Description
Payment
Rate
Facility=F
Nonfacility=NF
01 Pharmacy (October 1, 2005)
A facility or location where drugs and other medically related items and
services are sold, dispensed, or otherwise provided directly to patients.
NF
02 Telehealth Provided Other than in Patient’s Home (January 1, 2017)
The location where health services and health related services are provided
or received, through telecommunication technology. Patient is not located in
their home when receiving health services or health related services through
telecommunication technology.
(See “Special Considerations” below.)
F
03 School (January 1, 2003)
A facility whose primary purpose is education.
NF

POS Code and Name (effective date)
Description
Payment
Rate
Facility=F
Nonfacility=NF
04 Homeless Shelter (January 1, 2003)
A facility or location whose primary purpose is to provide temporary
housing to homeless individuals (e.g., emergency shelters, individual or
family shelters).
(See “Special Considerations” below.)
NF
05 Indian Health Service Free-standing Facility (January 1, 2003)
A facility or location, owned and operated by the Indian Health Service,
which provides diagnostic, therapeutic (surgical and nonsurgical), and
rehabilitation services to American Indians and Alaska Natives who do not
require hospitalization.
(See “Special Considerations” below.)
Not applicable
for
adjudication of
Medicare
claims;
systems must
recognize for
HIPAA
06 Indian Health Service Provider-based Facility (January 1, 2003)
A facility or location, owned and operated by the Indian Health Service,
which provides diagnostic, therapeutic (surgical and nonsurgical), and
rehabilitation services rendered by, or under the supervision of, physicians
to American Indians and Alaska Natives admitted as inpatients or
outpatients.
(See “Special Considerations” below.)
Not applicable
for
adjudication of
Medicare
claims;
systems must
recognize for
HIPAA
07 Tribal 638 Free-Standing Facility (January 1, 2003)
A facility or location owned and operated by a federally recognized
American Indian or Alaska Native tribe or tribal organization under a 638
agreement, which provides diagnostic, therapeutic (surgical and
nonsurgical), and rehabilitation services to tribal members who do not
require hospitalization.
(See “Special Considerations” below.)
Not applicable
for
adjudication of
Medicare
claims;
systems must
recognize for
HIPAA

POS Code and Name (effective date)
Description
Payment
Rate
Facility=F
Nonfacility=NF
08 Tribal 638 Provider-Based Facility (January 1, 2003)
A facility or location owned and operated by a federally recognized
American Indian or Alaska Native tribe or tribal organization under a 638
agreement, which provides diagnostic, therapeutic (surgical and
nonsurgical), and rehabilitation services to tribal members admitted as
inpatients or outpatients.
(See “Special Considerations” below.)
Not applicable
for
adjudication of
Medicare
claims;
systems must
recognize for
HIPAA
09 Prison/Correctional Facility (July 1, 2006)
A prison, jail, reformatory, work farm, detention center, or any other similar
facility maintained by either Federal, State or local authorities for the
purpose of confinement or rehabilitation of adult or juvenile criminal
offenders.
(See “Special Considerations” below.)
NF
10 Telehealth Provided in Patient’s Home (January 1, 2022)
The location where health services and health related services are provided or
received, through telecommunication technology. Patient is located in their
home (which is a location other than a hospital or other facility where the
patient receives care in
a private residence) when receiving health services or
health related services through telecommunication technology.
(See “Special
Considerations” below.)
NF
11 Office
Location, other than a hospital, skilled nursing facility (SNF), military
treatment facility, community health center, State or local public health
clinic, or intermediate care facility (ICF), where the health professional
routinely provides health examinations, diagnosis, and treatment of illness
or injury on an ambulatory basis.
NF
12 Home
Location, other than a hospital or other facility, where the patient receives
care in a private residence.
NF

POS Code and Name (effective date)
Description
Payment
Rate
Facility=F
Nonfacility=NF
13 Assisted Living Facility (October 1, 2003)
Congregate residential facility with self-contained living units providing
assessment of each resident’s needs and on-site support 24 hours a day, 7
days a week, with the capacity to deliver or arrange for services including
some health care and other services.
NF
14 Group Home (Code effective, October 1, 2003; description revised,
effective April 1, 2004)
A residence, with shared living areas, where clients receive supervision and
other services such as social and/or behavioral services, custodial service,
and minimal services (e.g., medication administration).
NF
15 Mobile Unit (January 1, 2003)
A facility/unit that moves from place-to-place equipped to provide
preventive, screening, diagnostic, and/or treatment services.
(See “Special Considerations” below.)
NF
16 Temporary Lodging (April 1, 2008)
A short-term accommodation such as a hotel, camp ground, hostel, cruise
ship or resort where the patient receives care, and which is not identified by
any other POS code.
NF
17 Walk-in Retail Health Clinic (No later than May 1, 2010)
A walk-in health clinic, other than an office, urgent care facility, pharmacy
or independent clinic and not described by any other Place of Service code,
that is located within a retail operation and provides, on an ambulatory
basis, preventive and primary care services.
(See “Special Considerations” below.)
NF
18 Place of Employment/Worksite (No later than May 1, 2013)
A location, not described by any other POS code, owned or operated by a
public or private entity where the patient is employed, and where a health
professional provides on-going or episodic occupational medical, therapeutic
or rehabilitative services to the individual.
Not applicable
for
adjudication of
Medicare
claims;
systems must
recognize for
HIPAA

POS Code and Name (effective date)
Description
Payment
Rate
Facility=F
Nonfacility=NF
19 Off Campus-Outpatient Hospital (January 1, 2016)
A portion of an off-campus hospital provider based department which
provides diagnostic, therapeutic (both surgical and nonsurgical), and
rehabilitation services to sick or injured persons who do not require
hospitalization or institutionalization.
(See “Special Considerations” below.)
F
20 Urgent Care Facility (January 1, 2003)
Location, distinct from a hospital emergency room, an office, or a clinic,
whose purpose is to diagnose and treat illness or injury for unscheduled,
ambulatory patients seeking immediate medical attention.
NF
21 Inpatient Hospital
A facility, other than psychiatric, which primarily provides diagnostic,
therapeutic (both surgical and nonsurgical), and rehabilitation services by,
or under, the supervision of physicians to patients admitted for a variety of
medical conditions.
F
22 On Campus-Outpatient Hospital (description revised January 1, 2016)
A portion of a hospital’s main campus which provides diagnostic,
therapeutic (both surgical and nonsurgical), and rehabilitation services to
sick or injured persons who do not require hospitalization or
institutionalization.
(See “Special Considerations” below.)
F
23 Emergency Room-Hospital
A portion of a hospital where emergency diagnosis and treatment of illness
or injury is provided.
F
24 Ambulatory Surgical Center
A freestanding facility, other than a physician's office, where surgical and
diagnostic services are provided on an ambulatory basis.
F

POS Code and Name (effective date)
Description
Payment
Rate
Facility=F
Nonfacility=NF
25 Birthing Center
A facility, other than a hospital's maternity facilities or a physician's office,
which provides a setting for labor, delivery, and immediate postpartum care
as well as immediate care of newborn infants.
NF
26 Military Treatment Facility
A medical facility operated by one or more of the Uniformed Services.
Military Treatment Facility (MTF) also refers to certain former U.S. Public
Health Service (USPHS) facilities now designated as Uniformed Service
Treatment Facilities (USTF).
F
27 Outreach Site/Street (October 1, 2023)
A non
-
permanent location on the street or found environment, not described by
any other POS code, where health professionals provide preventive, screening,
diagnostic, and/or treatment services to unsheltered homeless individuals.
NF
28-30 Unassigned
--
31 Skilled Nursing Facility
A facility which primarily provides inpatient skilled nursing care and
related services to patients who require medical, nursing, or rehabilitative
services but does not provide the level of care or treatment available in a
hospital.
F
32 Nursing Facility
A facility which primarily provides to residents skilled nursing care and
related services for the rehabilitation of injured, disabled, or sick persons,
or, on a regular basis, health-related care services above the level of
custodial care to other than individuals with intellectual disabilities.
NF
33 Custodial Care Facility
A facility which provides room, board and other personal assistance
services, generally on a long term basis, and which does not include a
medical component.
NF

POS Code and Name (effective date)
Description
Payment
Rate
Facility=F
Nonfacility=NF
34 Hospice
A facility, other than a patient's home, in which palliative and supportive
care for terminally ill patients and their families are provided.
F
35-40 Unassigned
--
41 Ambulance—Land
A land vehicle specifically designed, equipped and staffed for lifesaving
and transporting the sick or injured.
F
42 Ambulance—Air or Water
An air or water vehicle specifically designed, equipped and staffed for
lifesaving and transporting the sick or injured.
F
43-48 Unassigned
--
49 Independent Clinic (October 1, 2003)
A location, not part of a hospital and not described by any other Place of
Service code, that is organized and operated to provide preventive,
diagnostic, therapeutic, rehabilitative, or palliative services to outpatients
only.
NF
50 Federally Qualified Health Center
A facility located in a medically underserved area that provides Medicare
beneficiaries preventive primary medical care under the general direction of
a physician.
NF
51 Inpatient Psychiatric Facility
A facility that provides inpatient psychiatric services for the diagnosis and
treatment of mental illness on a 24-hour basis, by or under the supervision
of a physician.
F
52 Psychiatric Facility-Partial Hospitalization
A facility for the diagnosis and treatment of mental illness that provides a
planned therapeutic program for patients who do not require full time
hospitalization, but who need broader programs than are possible from
outpatient visits to a hospital-based or hospital-affiliated facility.
F

POS Code and Name (effective date)
Description
Payment
Rate
Facility=F
Nonfacility=NF
53 Community Mental Health Center
A facility that provides the following services: outpatient services, including
specialized outpatient services for children, the elderly, individuals who are
chronically ill, and residents of the CMHC’s mental health services area
who have been discharged from inpatient treatment at a mental health
facility; 24 hour a day emergency care services; day treatment, other partial
hospitalization services, or psychosocial rehabilitation services; screening
for patients being considered for admission to State mental health facilities
to determine the appropriateness of such admission; and consultation and
education services.
F
54 Intermediate Care Facility/Individuals with Intellectual Disabilities
A facility which primarily provides health-related care and services above
the level of custodial care to individuals but does not provide the level of
care or treatment available in a hospital or SNF.
NF
55 Residential Substance Abuse Treatment Facility
A facility which provides treatment for substance (alcohol and drug) abuse to
live-in residents who do not require acute medical care. Services include
individual and group therapy and counseling, family counseling, laboratory
tests, drugs and supplies, psychological testing, and room and board.
NF
56 Psychiatric Residential Treatment Center
A facility or distinct part of a facility for psychiatric care which provides a
total 24-hour therapeutically planned and professionally staffed group living
and learning environment.
F
57 Non-residential Substance Abuse Treatment Facility (October 1,
2003)
A location which provides treatment for substance (alcohol and drug) abuse
on an ambulatory basis. Services include individual and group therapy and
counseling, family counseling, laboratory tests, drugs and supplies, and
psychological testing.
NF

POS Code and Name (effective date)
Description
Payment
Rate
Facility=F
Nonfacility=NF
58 Non-residential Opioid Treatment Facility (January 1, 2020)
A location that provides treatment for opioid use disorder on an ambulatory
basis. Services include methadone and other forms of Medication Assisted
Treatment (MAT).
(See “Special Considerations” below.)
NF
59 Unassigned
--
60 Mass Immunization Center
A location where providers administer pneumococcal pneumonia and
influenza virus vaccinations and submit these services as electronic media
claims, paper claims, or using the roster billing method. This generally takes
place in a mass immunization setting, such as, a public health center,
pharmacy, or mall but may include a physician office setting.
NF
61 Comprehensive Inpatient Rehabilitation Facility
A facility that provides comprehensive rehabilitation services under the
supervision of a physician to inpatients with physical disabilities. Services
include physical therapy, occupational therapy, speech pathology, social or
psychological services, and orthotics and prosthetics services.
F
62 Comprehensive Outpatient Rehabilitation Facility
A facility that provides comprehensive rehabilitation services under the
supervision of a physician to outpatients with physical disabilities. Services
include physical therapy, occupational therapy, and speech pathology
services.
NF
63-64 Unassigned
--
65 End-Stage Renal Disease Treatment Facility
A facility other than a hospital, which provides dialysis treatment,
maintenance, and/or training to patients or caregivers on an ambulatory or
home-care basis.
NF
66-70 Unassigned
--
71 State or Local Public Health Clinic
A facility maintained by either State or local health departments that
provides ambulatory primary medical care under the general direction of a
physician.
NF

POS Code and Name (effective date)
Description
Payment
Rate
Facility=F
Nonfacility=NF
72 Rural Health Clinic
A certified facility which is located in a rural medically underserved area
that provides ambulatory primary medical care under the general direction
of a physician.
NF
73-80 Unassigned
--
81 Independent Laboratory
A laboratory certified to perform diagnostic and/or clinical tests independent
of an institution or a physician's office.
NF
82-98 Unassigned
--
99 Other Place of Service
Other place of service not identified above.
NF
The Medicare contractor can provide guidance regarding which code
applies in cases where the appropriate POS code may be unclear.
• Special Considerations for Telehealth Claims (Codes 02, 10)
Beginning in CY 2024, practitioners may receive either the facility or the
non-facility payment rate for an otherwise eligible Medicare telehealth
service, depending on whether the billing practitioner selects POS code 02 or
POS code 10. The only two valid POS codes for Medicare telehealth billing
in CY 2024 are POS 02 and POS 10. As appropriate, POS 02 or POS 10 may
be used and must be paired with the appropriate telehealth modifier
(modifier 93 for audio-only and modifier 95 for audio/video). The payment
rate for POS 02 is the facility payment rate (F); the payment rate for POS 10
is the non-facility rate (NF). Use of audio-only (93) or audio-video (95) does
not change rate of payment, only the POS code determines the non-facility or
facility payment rate.
• Special Considerations for Homeless Shelter (Code 04)
Note that for the purposes of receiving durable medical equipment
(DME), a homeless shelter is considered the beneficiary’s home.
Because DME is payable in the beneficiary’s home, the crosswalk
for Homeless Shelter (code 04) to Office (code 11) that was
mandated effective January 1, 2003, may need to be adjusted or local
policy developed so that HCPCS codes for DME are covered when
other conditions are met and the beneficiary is in a homeless shelter.
If desired, local contractors are permitted to work with their medical
directors to determine a new crosswalk such as from Homeless
Shelter (code 04) to Home (code 12) or Custodial Care Facility
(code 33) for DME provided in a homeless shelter setting. If a local
contractor is currently paying claims correctly, however, it is not
necessary to change the current crosswalk.
• Special Considerations for Indian Health Service (Codes 05, 06) and
Tribal 638 Settings (Codes 07, 08)
Medicare does not currently use the POS codes designated for these settings.
Follow the instructions you have received regarding how to process claims for
services rendered in IHS and Tribal 638 settings. If you receive claims with
these codes, you must initially accept them in terms of HIPAA compliance.
However, follow your “return as unprocessable” procedures after this initial
compliance check. Follow your “return as unprocessable" procedures when you
receive paper claims with these codes. (Note that while these codes became part
of the National POS code set effective January 1, 2003, Medicare contractors
received instructions regarding how to process claims with these codes effective
October 1, 2003, so that Medicare could be HIPAA compliant by October 16,
2003).
• Special Considerations for Mobile Unit Settings (Code 15)
When services are furnished in a mobile unit, they are often provided to serve
an entity for which another POS code exists. For example, a mobile unit may be
sent to a physician’s office or a skilled nursing facility. If the mobile unit is
serving an entity for which another POS code already exists, providers should
use the POS code for that entity. However, if the mobile unit is not serving an
entity which could be described by an existing POS code, the providers are to
use the Mobile Unit POS code 15. Apply the nonfacility rate to payments for
services designated as being furnished in POS code 15; apply the appropriate
facility or nonfacility rate for the POS code designated when a code other than
the mobile unit code is indicated.
A physician or practitioner's office, even if mobile, qualifies to serve as a
telehealth originating site. Assuming such an office also fulfills the requirement
that it be located in either a rural health professional shortage area as defined
under section 332(a)(1)(A) of the Public Health Service Act (42 U.S.C.
254e(a)(1)(A)) or in a county that is not included in a Metropolitan Statistical
Area as defined in section 1886(d)(2)(D) of the Act, the originating physician's
office should use POS code 11 (Office) in order to ensure appropriate payment
for services on the list of Medicare Telehealth Services.
• Special Considerations for Prison/Correctional Facility Settings (Code 09)
The addition of code 09 to the POS code set and Medicare claims processing
reflects Medicare’s compliance with HIPAA laws and regulations. Local
contractors must continue to comply with CMS current policy that does not
allow payment for Medicare services in a penal institution in most cases. The
addition of a POS code for a prison/correctional facility setting does not
supersede this policy. (See Pub. 100-04, Medicare Claims Processing, section
10.4, chapter 1.)
• Special Considerations for Walk-In Retail Health Clinic (Code 17)
(Effective no later than May 1, 2010)
It should be noted that, while some entities in the industry may elect to use POS
code 17 to track the setting of immunizations, Medicare continues to require its
billing rules for immunizations claims, which are found in chapter 18, section
10 of this manual. Contractors are to instruct providers and suppliers of
immunizations to continue to follow these Medicare billing rules. However,
Medicare contractors are to accept and adjudicate claims containing POS code
17, even if its presence on a claim is contrary to these billing instructions.
• Special Considerations for Services Furnished to Registered Inpatients
When a physician/practitioner furnishes services to a registered inpatient,
payment is made under the PFS at the facility rate. To that end, a
physician/practitioner/supplier furnishing services to a patient who is a
registered inpatient, shall, at a minimum, report the inpatient hospital POS code
21 irrespective of the setting where the patient actually receives the face-to-face
encounter. In other words, reporting the inpatient hospital POS code 21 is a
minimum requirement for purposes of triggering the facility payment under the
PFS when services are provided to a registered inpatient. If the
physician/practitioner is aware of the exact setting the beneficiary is a
registered inpatient, the appropriate inpatient POS code may be reported
consistent with the code list annotated in this section (instead of POS 21). For
example, a physician/practitioner may use POS 31, for a patient in a SNF
receiving inpatient skilled nursing care, POS 51, for a patient registered in a
Psychiatric Inpatient Facility, and POS 61 for patients registered in a
Comprehensive Inpatient Rehabilitation Facility.
• Special Considerations for Outpatient Hospital Departments
The place of service (POS) code for “Outpatient Hospital” has been expanded.
The description of POS 22 has been revised from “Outpatient Hospital” to “On
Campus-Outpatient Hospital” and POS 19 has been created for the “Off
Campus- Outpatient Hospital” setting. Throughout this Internet Only Manual
(IOM) you may find references to “Outpatient Hospital” that do not
differentiate between the “On Campus” or “Off Campus” setting; however, any
reference to POS 22 (formerly “Outpatient Hospital”) found anywhere within
the IOM is now defined as “On Campus-Outpatient Hospital.” In addition, POS
19 will also apply in the majority of situations describing an outpatient hospital
setting. When a physician/practitioner furnishes services to an outpatient of a
hospital, payment is made under the PFS at the facility rate.
Physicians/practitioners who furnish services to a hospital outpatient, including
in a hospital outpatient department (including in a provider-based department
of that hospital) or under arrangement to a hospital shall, at a minimum, report
the off campus-outpatient hospital POS code 19 or on campus-outpatient
hospital POS code 22 irrespective of the setting where the patient actually
receives the face-to-face encounter. In other words, reporting the outpatient
hospital POS code 19 or 22 is a minimum requirement for purposes of
triggering the facility payment amount under the PFS when services are
provided to a registered outpatient. If the physician/practitioner is aware of the
exact setting where the beneficiary is a registered hospital outpatient, the
appropriate outpatient facility POS code may be reported consistent with the
code list annotated in this section (instead of POS 19 or 22).
For example, physicians/practitioners may use POS code 23 for services
furnished to a patient registered in the emergency room, POS 24 for patients
registered in an ambulatory surgical center, and POS 56 for patients registered
in a psychiatric residential treatment center.
NOTE: Physicians/practitioners who perform services in a hospital
outpatient department shall use, at a minimum, POS code 19 (Off
Campus- Outpatient Hospital) or POS code 22 (On Campus-Outpatient
Hospital).
Code 19 or 22 (or other appropriate outpatient department POS code as
described above) shall be used unless the physician maintains separate office
space in the hospital or on the hospital campus and that physician office space
is not considered a provider-based department of the hospital as defined in 42.
C.F.R.
413.65. Physicians shall use POS code 11 (office) when services are performed
in a separately maintained physician office space in the hospital or on the
hospital campus and that physician office space is not considered a provider-
based department of the hospital. Use of POS code 11(office) in the hospital
outpatient department or on hospital campus is subject to the physician self-
referral provisions set forth in 42 C.F.R 411.353 through 411.357.
• Special Consideration for Ambulatory Surgical Centers (Code 24)
When a physician/practitioner furnishes services to a patient in a Medicare-
participating ambulatory surgical center (ASC), the POS code 24 (ASC) shall
be used.
NOTE: Physicians/practitioners who perform services in an ASC shall use

POS code 24 (ASC). Physicians/practitioners are not to use POS code 11
(office) for ASC based services unless the physician has an office at the same
physical location of the ASC, which meets all other requirements for operating
as a physician office at the same physical location as the ASC – including
meeting the “distinct entity” criteria defined in the ASC State Operations
Manual that precludes the ASC and an adjacent physician office from being
open at the same time -- and the physician service was actually performed in the
office suite portion of the facility.
See Pub 100-07, Medicare State Operations Manual, Appendix L - Guidance
for Surveyors: Ambulatory Surgical Centers for a complete set of applicable
ASC definitions, basic requirements, and conditions of coverage. It is
available at the following link:
http://www.cms.gov/manuals/Downloads/som107ap_l_ambulatory.pdf
• Special Considerations for Hospice (Code 34)
When a physician/practitioner furnishes services to a patient under the
hospice benefit, use the following guidelines to identify the appropriate
POS.
When a beneficiary is in an “inpatient” respite or general “inpatient” care stay,
the POS code 34 (hospice) shall be used. When a beneficiary who has elected
coverage under the Hospice benefit is receiving inpatient hospice care in a
hospital, SNF, or hospice inpatient facility, POS code 34 (Hospice) shall be
used to designate the POS on the claim.
For services provided to a hospice beneficiary in an outpatient setting, such as
the physician/nonphysician practitioner’s office (POS 11); the beneficiary’s
home (POS 12), i.e., not operated by the hospice; or other outpatient setting
(e.g., off campus-outpatient hospital (POS 19) or on campus-outpatient hospital
(POS 22)), the patient’s physician or nonphysician practitioner or hospice
independent attending physician or nurse practitioner, shall assign the POS
code that represents that setting, as appropriate.
There may be use of nursing homes as the hospice patient’s “home,” where the
patient resides in the facility but is receiving a home level of care. In addition,
hospices are also operating “houses” or hospice residential entities where
hospice patients receive a home level of care. In these cases, physicians and
nonphysician practitioners, including the patient’s independent attending
physician or nurse practitioner, shall use the appropriate POS code representing
the particular setting, e.g., POS code 32 for nursing home, POS code 13 for an
assisted living facility, or POS code 14 for group home.
• Special Considerations for Non-residential Opioid Treatment Facility (Code
58)
NOTE: OUD treatment services furnished at Opioid Treatment Programs are not
considered physician services and are separately paid under the bundled payment
established under sections 1833(a)(1)(CC) and 1834(w) of the Social Security
Act.
• Paper Claims
Adjudicate paper claims with codes from the National POS code set as you
would for electronic claims.
10.6 - A/B Medicare Administrative Contractor (MAC) (B) Instructions
for Place of Service (POS) Codes
(Rev. 3490, Issued: 04-01-16, Effective: 04-25-16, Implementation: 04-25-16)
For purposes of payment under the Medicare Physician Fee Schedule (MPFS), the POS
code is generally used to reflect the actual setting where the beneficiary receives the face-
to-face service. For example, if the physician’s face-to-face encounter with a patient
occurs in the office, the correct POS code on the claim, in general, reflects the 2-digit
POS code 11 for office. In these instances, the 2-digit POS code (Item 24B on the claim
Form CMS-1500) will match the address and ZIP entered in the service location (Item 32
on the 1500 Form) – the physical/geographical location of the physician. However, there
are two exceptions to this general rule – these are for a service rendered to a patient who
is a registered inpatient or an outpatient of a hospital. In these cases, the correct POS
code -- regardless of where the face-to-face service occurs -- is that of the appropriate
inpatient POS code (at a minimum POS code 21) or that of the appropriate outpatient
hospital POS code (at a minimum POS code 19 or 22, for outpatient services performed
off campus or on campus) as discussed in section 10.5 of this chapter. So, if in the above
example, the patient seen in the physician’s office is actually an inpatient of the hospital,
POS code 21, for inpatient hospital, is correct. In this example, the POS code reflects a
different setting than the address and ZIP code of the practice location (the physician’s
office).
For MPFS payment purposes the determinant of payment is the locality where the
physician or supplier furnished the service. Medicare has both facility and non-facility
designations for services paid under the physician fee schedule. In accordance with
Chapter 1, Section 10.1.1 (Payment Jurisdiction Among Local Medicare Administrative
Contractors (MACs) for Services Paid Under the Physician Fee Schedule and Anesthesia
Services) of this manual, the jurisdiction for processing a request for payment for services
paid under the MPFS is governed by the payment locality where the physician or supplier
furnished the service and will be based on the ZIP code. CMS requires that the address
and ZIP code of the physician’s practice location be placed on the claim form in order to
determine the appropriate locality -- item 32 on the paper claim Form CMS 1500 or in the
corresponding loop on its electronic equivalent.
For specific POS instructions and determination of the applicable payment locality for the
PC (professional interpretation) and the TC of diagnostic tests see chapter 13, section 150
of this manual. For general policy on POS code assignment, see chapter 12, section
20.4.2 of this manual regarding the site of service payment differential under MPFS.
If the physician bills for lab services performed in his/her office, the POS code for
"Office" is shown. If the physician bills for a lab test furnished by another physician,
who maintains a lab in his/her office, the code for "Other" is shown. If the physician bills
for a lab service furnished by an independent lab, the code for "Independent Laboratory"
is used. Items 21 and 22 on the Form CMS-1500 must be completed for all laboratory
work performed outside a physician's office. If an independent lab bills, the place where
the sample was taken is shown. An independent laboratory taking a sample in its
laboratory shows "81" as place of service. If an independent laboratory bills for a test on
a sample drawn on an inpatient or outpatient of a hospital, it uses the code for the
inpatient (POS code 21), off campus-outpatient hospital (POS code 19), or on campus-
outpatient hospital (POS code 22), respectively.
For hospital visits by physicians, presume, in the absence of evidence to the contrary, that
visits billed for were made. However, review a sample of physician's records when there
are questionable patterns of utilization. Confirm these visits where the medical facts do
not support the frequency of the physician's visits or in cases of beneficiary complaints.
If questioning whether the visit had been made, ascertain whether the physician's own
entry is in the patient's record at the provider. Accept an entry where the nurses' notes
indicate that the physician saw the patient on a given day. A statement by the beneficiary
is also acceptable documentation if it was made close to the alleged date of the visit.
Entries in the physician's records represent possible secondary evidence. However, these
are of less value since they are self-serving statements. Exercise judgment regarding
their authenticity. The policy requiring daily physician visits is not conclusive if, in the
individual case, the facts did not support a finding that daily visits were made.
If a claim lacks a valid place of service (POS) code in item 24b, or contains an invalid
POS in item 24b, return the claim as unprocessable to the provider or supplier, using
Group Code CO, Claim Adjustment Remark Code (CARC) 16, and Remittance Advice
Remark Code (RARC) M77. Effective for claims received on or after April 1, 2004, only
one POS may be submitted on the Form CMS-1500 for services paid under the MPFS
and anesthesia services. If the place of service is missing and the MAC cannot infer the
place of service from the procedure code billed (e.g., a procedure code for which the
definition is not site specific or which can be performed in more than one setting), then
return services as unprocessable.
If place of service is inconsistent with procedure code billed, then edit for consistency or
compatibility between the place of service and site-specific procedure codes. If the place
of service is valid but inconsistent or incompatible with the procedure billed (e.g., the
place of service is inpatient hospital and the procedure code billed is office visit), then
return services as unprocessable since the MAC typically will not know whether the
procedure code or the place of service is incorrect in such instances. If place of service is
invalid, then edit for the validity of the place of service coding. If the place of service
code is not valid (e.g., the number designation has not been assigned or defined by CMS),
then return services as unprocessable.
10.7 - Type of Service (TOS)
(Rev. 2814, Issued: 11-15-13, Effective: 01-01-14, Implementation: 01-06-14)
Medicare Administrative Contractors (MACs) must assign the proper TOS using the
annual HCPCS update from the CMS mainframe. Changes to this list are issued annually
via a Recurring Update Notification. Some procedures may have more than one
applicable TOS. For claims received on or after April 3, 1995, CWF produced alerts on
codes with incorrect TOS designations. Effective July 3, 1995, CWF began rejecting
codes with incorrect TOS designations.
The only exceptions to this annual update are:
• Surgical services billed for dates of service through December 31, 2007,
containing the ASC facility service modifier SG must be reported as TOS F.
Effective for services on or after January 1, 2008, the SG modifier is no longer
applicable for Medicare services. ASC providers should discontinue applying the
SG modifier on ASC facility claims. The indicator ‘F’ does not appear in the
TOS table because its use depends upon claims submitted with POS 24 (ASC
Facility) from an ASC (specialty 49). This became effective for dates of service
January 1, 2008 and after.
• Surgical services billed with an assistant-at-surgery modifier (80-82, AS) must be
reported with TOS 8. The 8 indicator does not appear on the TOS table because
its use is dependent upon the use of the appropriate modifier. (See Pub. 100-04,
Medicare Claims Processing Manual, Chapter 12, "Physician/Nonphysician
Practitioner," for instructions on when assistant-at-surgery is allowable.)
• TOS H appears in the list of descriptors. However, it does not appear in the table.
In CWF, "H" is used only as an indicator for hospice. The contractor should not
submit TOS H to CWF at this time.
• For outpatient services, when a transfusion medicine code appears on a claim that
also contains a blood product, the service is paid under reasonable charge at 80%,
coinsurance and deductible apply. When transfusion medicine codes are paid
under the clinical laboratory fee schedule pay at 100%, coinsurance and
deductible do not apply.
NOTE: For injection codes with more than one possible TOS designation, use the
following guidelines when assigning the TOS:
When the choice is L or 1,
• Use TOS L when the drug is used related to ESRD; or
• Use TOS 1 when the drug is not related to ESRD and is administered in the
office.
When the choice is G or 1:
• Use TOS G when the drug is an immunosuppressive drug; or
• Use TOS 1 when the drug is used for other than immunosuppression.
When the choice is P or 1,
• Use TOS P if the drug is administered through durable medical equipment
(DME); or
• Use TOS 1 if the drug is administered in the office.
The place of service or diagnosis may be considered when determining the appropriate
TOS. The descriptors for each of the TOS codes listed in the annual HCPCS update are:
Type of Service Indicators
Code
Description
0
Whole Blood
1
Medical Care
2
Surgery
3
Consultation
4
Diagnostic Radiology
5
Diagnostic Laboratory
6
Therapeutic Radiology
7
Anesthesia
8
Assistant at Surgery
9
Other Medical Items or Services
A
Used DME
B
High Risk Screening Mammography
C
Low Risk Screening Mammography
D
Ambulance
E
Enteral/Parenteral Nutrients/Supplies
F
Ambulatory Surgical Center (Facility Usage for Surgical Services)
G
Immunosuppressive Drugs
H
Hospice
J
Diabetic Shoes
K
Hearing Items and Services
L
ESRD Supplies
Code
Description
M
Monthly Capitation Payment for Dialysis
N
Kidney Donor
P
Lump Sum Purchase of DME, Prosthetics, Orthotics
Q
Vision Items or Services
R
Rental of DME
S
Surgical Dressings or Other Medical Supplies
T
Outpatient Mental Health Treatment Limitation
U
Occupational Therapy
V
Pneumococcal/Flu Vaccine
W
Physical Therapy
10.8 - Requirements for Specialty Codes
(Rev. 1725, Issued: 05-01-09, Effective: 07-01-09, Implementation: 07-06-09)
Medicare physician/non-physician practitioner specialty codes describe the
specific/unique types of medicine that physicians and non-physician practitioners (and
certain other suppliers) practice. Physicians self-designate their Medicare physician
specialty on their Medicare enrollment application (CMS-855I) or on the Internet-based
Provider Enrollment, Chain and Ownership System. Non-physician practitioners are
assigned a Medicare specialty code when they enroll based on their profession. Specialty
codes are used by CMS for programmatic and claims processing purposes.
A. A physician specialty association will submit a specialty code request to the Director,
Division of Practitioner Services, Center for Medicare Management, Centers for
Medicare & Medicaid Services, Mail Stop C4-01-26, 7500 Security Blvd., Baltimore,
MD 21244.
Medicare contractors shall not add any specialty codes to the list. They must send all
requests for expansion of the specialty code list to the Director, Division of Practitioner
Services, at the address above.
B. When considering a request for expanding the specialty code list for physician and
non-physician practitioners, CMS will take into consideration the following:
• Whether the requested specialty has the authority to bill Medicare independently;
• The requester’s stated reason or purpose for the code;
• Evidence that the practice pattern of the specialty is markedly different from that
of the dominant parent specialty;
• Evidence of any specialized training and/or certification required;
• Whether the specialty treats a significant volume of the Medicare population;
• Whether the specialty is recognized by another organization, such as the
American Board of Medical Specialties; and
• Whether the specialty has a corresponding Healthcare Provider Taxonomy Code.
Physicians may not have a specialty code of 70 (single or multi-specialty Clinic or Group
Practice.) Contractors must contact physicians whose records indicate specialty code 70
and require the physicians to update their enrollment records by submitting a CMS-8551
with a specialty that is valid for a physician.
10.8.1 - Assigning Specialty Codes by A/B MACs (B) and DME MACs
Physicians are allowed to choose a primary and a secondary specialty code. If the A/B
MAC (B) and DME MAC provider file can accommodate only one specialty code, the
A/B MAC (B) or DME MAC assigns the code that corresponds to the greater amount of
allowed charges. For example, if the practice is 50 percent ophthalmology and 50
percent otolaryngology, the A/B MAC (B)/DME MAC compares the total allowed
charges for the previous year for ophthalmology and otolaryngology services. They
assign the code that corresponds to the greater amount of the allowed charges.
10.8.2 - Physician Specialty Codes
(Rev. 12456; Issued:01-11-24; Effective:07-01-24; Implementation:07-01-24)
Code
Physician Specialty
01
General Practice
02
General Surgery
03
Allergy/Immunology
04
Otolaryngology
05
Anesthesiology
06
Cardiology
07
Dermatology
08
Family Practice
09
Interventional Pain Management
10
Gastroenterology
11
Internal Medicine
12
Osteopathic Manipulative Medicine
13
Neurology
14
Neurosurgery
16
Obstetrics/Gynecology
17
Hospice and Palliative Care
18
Ophthalmology
19
Oral Surgery (dentists only)
20
Orthopedic Surgery
21
Cardiac Electrophysiology
22
Pathology
23
Sports Medicine
Code
Physician Specialty
24
Plastic and Reconstructive Surgery
25
Physical Medicine and Rehabilitation
26
Psychiatry
27
Geriatric Psychiatry
28
Colorectal Surgery (formerly proctology)
29
Pulmonary Disease
30
Diagnostic Radiology
33
Thoracic Surgery
34
Urology
35
Chiropractic
36
Nuclear Medicine
37
Pediatric Medicine
38
Geriatric Medicine
39
Nephrology
40
Hand Surgery
41
Optometry
44
Infectious Disease
46
Endocrinology
48
Podiatry
66
Rheumatology
70
Single or Multispecialty Clinic or Group Practice
72
Pain Management
76
Peripheral Vascular Disease
77
Vascular Surgery
78
Cardiac Surgery
79
Addiction Medicine
81
Critical Care (Intensivists)
82
Hematology
83
Hematology/Oncology
84
Preventive Medicine
85
Maxillofacial Surgery
86
Neuropsychiatry
90
Medical Oncology
91
Surgical Oncology
92
Radiation Oncology
93
Emergency Medicine
94
Interventional Radiology
98
Gynecological/Oncology
99
Unknown Physician Specialty
C0
Sleep Medicine
C3
Interventional Cardiology
C5
C6
C7
C8
Dentist
Hospitalist
Advanced Heart Failure and Transplant Cardiology
Medical Toxicology

Code
Physician Specialty
C9
Hematopoietic Cell Transplantation and Cellular
Therapy
D3
Medical Genetics and Genomics
D4
Undersea and Hyperbaric Medicine
D7 Micrographic Dermatologic Surgery
D8 Adult Congenital Heart Disease
E1 Marriage and Family Therapist
E2 Mental Health Counselors
E3 Dental Anesthesiology
E4 Dental Public Health
E5 Endodontics
E6 Oral and Maxillofacial Pathology
E7 Oral and Maxillofacial Radiology
E9 Oral Medicine
F1 Orofacial Pain
F2 Orthodontics and Dentofacial Orthopedics
F3 Pediatric Dentistry
F4 Periodontics
F5 Prosthodontics
F6 Epileptologists
10.8.3 - Nonphysician Practitioner, Supplier, and Provider Specialty
Codes
(Rev. 10124, Issued: 05-08-2020, Effective: 10-01-2020, Implementation:10-05-2020)
The following list of 2-digit codes and narrative describe the kind of medicine non-
physician practitioners or other healthcare providers/suppliers practice.
Code
Non-physician Practitioner/Supplier/Provider Specialty
15
Speech Language Pathologists
31
Intensive Cardiac Rehabilitation
32
Anesthesiologist Assistant
42
Certified Nurse Midwife (effective July 1, 1988)
43
Certified Registered Nurse Anesthetist (CRNA)
45
Mammography Screening Center
47
Independent Diagnostic Testing Facility (IDTF)
49
Ambulatory Surgical Center
50
Nurse Practitioner
51
Medical supply company with orthotic personnel certified by an
accrediting organization
52
Medical supply company with prosthetic personnel certified by an
accrediting organization
53
Medical supply company with prosthetic/orthotic personnel certified by an
accrediting organization
54
Medical supply company not included in 51, 52, or 53
55
Individual orthotic personnel certified by an accrediting organization

Code
Non-physician Practitioner/Supplier/Provider Specialty
56
Individual prosthetic personnel certified by an accrediting organization
57
Individual prosthetic/orthotic personnel certified by an accrediting
organization
58
Medical Supply Company with registered pharmacist
59
Ambulance Service Supplier, e.g., private ambulance companies, funeral
homes
60
Public Health or Welfare Agencies (Federal, State, and local)
61
Voluntary Health or Charitable Agencies (e.g., National Cancer Society,
National Heart Association, Catholic Charities)
62
Psychologist (Billing Independently)
63
Portable X-Ray Supplier (Billing Independently)
64
Audiologist (Billing Independently)
65
Physical Therapist in Private Practice
67
Occupational Therapist in Private Practice
68
Clinical Psychologist
69
Clinical Laboratory (Billing Independently)
71
Registered Dietician/Nutrition Professional
73
Mass Immunization Roster Billers (Mass Immunizers have to roster bill
assigned claims and can only bill for immunizations)
74
Radiation Therapy Centers
75
Slide Preparation Facilities
80
Licensed Clinical Social Worker
87
All other suppliers, e.g., Drug Stores
88
Unknown Provider
89
Certified Clinical Nurse Specialist
95
Unknown Supplier
96
Optician
97
Physician Assistant
A0
Hospital
A1
Skilled Nursing Facility
A2
Intermediate Care Nursing Facility
A3
Nursing Facility, Other
A4
Home Health Agency
A5
Pharmacy
A6
Medical Supply Company with Respiratory Therapist
A7
Department Store
A8
Grocery Store
B1
Oxygen/Oxygen Related Equipment
B2
Pedorthic Personnel
B3
Medical Supply Company with Pedorthic Personnel
B4
Rehabilitation Agency
B5
Ocularist
C1
Centralized Flu
C2
Indirect Payment Procedure

Code
Non-physician Practitioner/Supplier/Provider Specialty
C4
Restricted Use
D1
Medicare Diabetes Preventive Program
D2
Restricted Use
D5
Opioid Treatment Program
D6
Home Infusion Therapy Services
NOTE: Specialty Code Use for Service in an Independent Laboratory. For services
performed in an independent laboratory, show the specialty code of the physician
ordering the x-rays and requesting payment. If the independent laboratory requests
payment, use type of supplier code "69".
10.9 - Miles/Times/Units/Services (MTUS)
(Rev. 1970, Issued: 05-21-10, Effective: 10-01-2010, Implementation: 10-04-10)
Miles/Times/Units/Services (MTUS) count and MTUS indicator fields are on Part B
Physician/Supplier Claims. These fields are documented in the CMS National Claims
History Data Dictionary.
Shared systems are to put MTUS count and MTUS indicators on all claims at the line
item level.
The purpose of the MTUS Count Field on the line item is to document additional
information reflecting certain volumes related to indicators. In most cases, the value in
this field will be the same as in the Service Count Field on the line item; however, for
services such as anesthesia the field values will differ. In this case, the service count field
will likely contain a value of 1 for the occurrence of the surgery while the MTUS Count
Field will contain the actual time units that the anesthesiologist spent with the patient in
15 minute increments or a fraction thereof.
The purpose of the MTUS Indicator Field is to indicate what the value entered into the
MTUS Count Field means. There are 6 indicator values, as follows:
Indicator
Description
0
No allowed services
1
Ambulance transportation miles
2
Anesthesia Time Units
3
Services
4
Oxygen units
5
Units of Blood
Examples of how to code these fields are specified in §10.9.1 below.
10.9.1 - Methodology for Coding Number of Services, MTUS Count and
MTUS Indicator Fields
(Rev. 1970, Issued: 05-21-10, Effective: 10-01-2010, Implementation: 10-04-10)

The following instructions should be used as a guide for coding the number of services,
MTUS Count and MTUS Indicator fields on the Part B Physician/Supplier Claim. These
fields are documented in the CMS National Claims History Data Dictionary as
CWFB_SRVC_CNT, CWFB_MTUS_CNT, and CWFB_MTUS_IND_CD, respectively.
Services not falling into examples B, C, E, or F should be coded as shown in example D
(services/pricing units).
A. No Allowed Services - (CWFB_MTUS_IND_CD = 0)
For claims reporting no allowed services, the following example should be used to code
the line item:
A total of 2 visits was reported for HCPCS code 99211: Office or other outpatient visit
for the management of an established patient. Both services were denied.
Number of services:
2 (furnished)
MTUS (services):
0 (allowed)
MTUS indicator:
0
B. Ambulance Miles - (CWFB_MTUS_IND_CD = 1)
For claims reporting ambulance miles, the following example should be used to code the
line item:
Mileage Reporting: A total of 10 miles (1 trip) was reported for HCPCS code A0425:
Ground mileage, per statute mile.
Number of services:
10
MTUS (miles):
10
MTUS indicator:
1
C. Anesthesia Time Units - (CWFB_MTUS_IND_CD = 2)
For claims reporting anesthesia time units in 15-minute periods or fractions of 15-
minute periods, the following example should be used to code the line item:
A total of 1 allowed service is reported for HCPCS code 00142: Anesthesia for
procedures on eye; lens surgery. The anesthesiologist attended the patient for 35
minutes.
Number of services:
1
MTUS (time units):
23 (one decimal point implied) *
MTUS indicator:
2
*Two 15-minute periods + 1/3 of a 15-minute period equals 2.3

D. Services/Pricing Units - (CWFB_MTUS_IND_CD = 3)
For claims reporting a service or pricing unit, the following examples should be
used to code the line item:
Example 1: A total of 2 visits was reported for HCPCS code 99211: Office or other
outpatient visit for the management of an established patient.
Number of services:
2
MTUS (services):
2
MTUS indicator:
3
Example 2: A total of 500 milligrams was administered for HCPCS code J0120:
Injection, Tetracycline, up to 250 mg.
NOTE: The number of milligrams should not be reported in the service or MTUS fields.
Instead, report the number of pricing units. In this case, up to 250 mg equals 1
unit/service. Thus, 500 mg equals 2 units/services.
Number of services:
2
MTUS (services):
2
MTUS indicator:
3
Example 3: A total of 24 cans was purchased, each containing 300 calories for HCPCS
code B4150: Enteral Formulae, 100 calories.
NOTE: Neither number of cans nor the number of calories should be reported in
the services or MTUS fields. Instead, report the number of pricing units. In this
case, 100 calories equals 1 unit/service. Thus, 24 cans * 300 calories / 100
calories equals 72 units/services.
Number of services:
72
MTUS (services):
72
MTUS indicator:
3
E. Oxygen Services - (CWFB_MTUS_IND_CD = 4)
For claims reporting oxygen units, the following example should be used
to code the line item:
A total of 2 allowed services was reported for HCPCS code E0441:
Oxygen contents, gaseous, 1 month’s supply = 1 unit. The claim reported
a 2 month’s supply of oxygen.
Number of services:
2
MTUS:
2
MTUS indicator:
4
F. Blood Services - (CWFB_MTUS_IND_CD = 5)
For claims reporting blood units, the following example should be used to
code the line item:
A total of 6 units of blood (services) was furnished for HCPCS code
P9010: Blood (whole), for transfusion, per unit. Two units were denied.
Number of services:
6 (furnished)
MTUS (units):
4 (allowed)
MTUS indicator:
5
20 - Patient’s Request for Medical Payment Form CMS-1490S
(Rev.: 4388; Issued: 09-06-19; Effective: 10-07-19; Implementation: 10-07-19)
The CMS implemented a new version of the Form CMS-1490S effective January 1,
2019. The revised form is version 01/18, OMB control number 0938-1197. The revised
form will replace the previous version of the form 01/05, OMB control number 0938-
0999.
The term, “Form CMS-1490S” refers to the form generically, independent of a given
version.
Medicare will conduct a dual-use period (January 1, 2019 through March 31, 2019)
during which Beneficiaries (or their representatives) can send Medicare claims on either
the old or the revised form. When the dual-use period is over, Medicare will accept
beneficiary paper claims on only the revised Form CMS-1490S, version 01/18.
This form is used only by beneficiaries (or their representatives) who complete and file
their own claims. It contains the patient’s comparable items of data that are on the Form
CMS-1500. When the Form CMS-1490S is used, an itemized bill must be submitted
with the claim. Some enrollees may want to keep the original itemized physician and
supplier bills for income tax or complementary insurance purposes. Photocopies of
itemized bills are acceptable for Medicare deductible and payment purposes if there is no
evidence of alteration. Social Security offices use the Form CMS-1490S when assisting
beneficiaries in filing Part B Medicare claims.
Although §1848(g)(4) of the Act requires physicians and suppliers to submit Part B
Medicare claims for services furnished on or after September 1, 1990, contractors
continue to accept, process, and pay for covered services submitted by beneficiaries on a
Form CMS-1490S if there is no clear indication that the service provider intends to file a
claim. An itemized bill for services on or after September 1, 1990, which clearly
indicates the physician or supplier intends to file a Part B claim for the patient, may be
returned to the beneficiary.
For Medicare covered services received on or after September 1, 1990, the Form CMS-
1490S is used by beneficiaries to submit Part B claims only if the service provider refuses
to do so or if one of the following situations applies:
• DME purchases from private sources;
• Cases in which a physician/supplier does not possess information essential for
filing an MSP claim. Assume this is the case if the beneficiary files an MSP
claim and encloses the primary insurer's payment determination notice and there
is no indication that the service provider was asked to file but refused to do so;
• Services paid under the indirect payment procedure;
• Foreign claims;
• Services furnished by sanctioned physicians and suppliers which are approved for
payment to the beneficiary per the Program Integrity Manual (PIM); and
• Other unusual or unique situations that are evaluated on a case-by-case basis.
If the contractor approves 11 or more Form CMS-1490S claims in a calendar month for
services performed on or after September 1, 1990, by the same physician or supplier,
monitor the provider's claims submissions and take appropriate action.
The contractor continues to stock Form CMS-1490S and, upon request, furnish
beneficiaries with these forms. (Beneficiaries need these forms to file claims for services
that physicians/suppliers are not required to submit (e.g., services prior to September 1,
1990), or refuse to submit to Part B on their behalf.)
30 - Printing Standards and Print File Specifications Form CMS-1500
(Rev. 899, Issued: 03-31-06; Effective: 10-01-06; Implementation: 10-02-06)
The National Uniform Claims Committee (NUCC) has approved the printing standards
for Form CMS-1500 (08-05) paper claim. These standards are as follows:
The Form CMS-1500 (08-05) is designed to accommodate 10-pitch Pica type, 6 lines per
inch vertical and 10 characters per inch (cpi) horizontal. Once adjusted to the left and
right, PICA Alignment blocks in the first print line and characters appear within form
lines as shown in the print file matrix.
Also provided on the Form CMS-1500 (08-05) is a position bar. This is a thick
horizontal line that is at the base of the PICA alignment Boxes.

The Form CMS-1500 (08-05) is used in four different styles. Any one of these four
styles may be printed from two negatives in concurrence with the layout that was
approved by the NUCC. The face/back negative furnished must be used for all parts.
Compliance with these standards is required to facilitate the use of image processing
technology such as Optical Character Recognition (OCR), facsimile transmission, and
image storing.
Cut Sheet:
Size - 8.5 by 11 inches (plus or minus .0625 inch) or 217mm by 279mm (plus or minus
2mm).
Print - Face and back, head to head.
Margins -
Face - The top margin from the top edge of the form to the first print position is 1.33
inches or 34mm. The left margin is 0.3 inches to the left end of the first print position.
Back - 0.25 inch head and foot, 0.25 inch left and right or 6.35 mm head and foot, 6.35
mm left and right.
Offset - The X and Y offset for margins must not vary by more than +/-0.1 inch or 2.54
mm from sheet to sheet.
The X offset refers to the horizontal distance from the left edge of the paper to the
beginning of the printing. The Y offset refers to the vertical distance between the top of
the paper and the beginning of the printing.
Askewity - The askewity of the printed image must be no greater than 0.15mm in
100mm.
Paper Stock - Basis weight 20# recycled 30% postconsumer waste, White Environmental
Paper Alliance (EPA) or approved paper stock. Smoothness: FS to be (140-160), or
equivalent stock.
Ink color -
Face - (OCR-Red Ink) must be in Flint J-6983 Red OCR “dropout” ink or an exact
match, formerly known as Sinclair Valentine). There is to be no contamination with
“Black” ink or pigment. Printer must maintain proper ink reflections limits of the OCR
reader specified by the purchaser.
Back - Same as face.

Titles - Color of any titles if applicable: Are to be in the same ink as the form, Flint
J6983 OCR Red “dropout” ink.
Symbol - The identifiable 1500 in a rectangle located in the upper left front of the form
above the PICA boxes is to be in black ink.
Two Part Snap-set:
Size - Dimensions are same as Cut Sheet (detached 8.5 by 11 inches), plus top stub (.5 to
.75 inches).
Print -
Part 1 - Face and back - head to head.
Part 2 - Face and back - head to head.
Margins - Same as Cut Sheet.
Askewity - Same as Cut Sheet.
Stock -
Part 1 - Carbonless, 20 CB - Recycled White
Part 2 - Any color that will not interfere with scanning of Part 1 sheet.
Ink Color -
Part 1 - (OCR-Red Ink) must be in Flint J-6983 Red OCR “dropout” ink or an exact
match.
Part 2 - Any color that will not interfere with scanning of Part 1 sheet.
Titles - Color of any titles if applicable: Are to be in the same ink as the form, Flint
J6983 OCR Red “dropout” ink.
Symbol - The identifiable 1500 in a rectangle located in the upper left front of the form
above the PICA boxes is to be in black ink.
Perforations - Perforate top stub for disassembly of parts.
One Part Marginally Punched Continuous Form:
Size - Same dimensions as for Cut Sheet, plus 0.5 inch left and right, (overall: 9.5 by 11
inches, detached: 8.5 by 11 inches).

Print - Face and back, head to head.
Margins - On detached sheet, same as for Cut Sheet.
Askewity - On detached sheet, same as for Cut Sheet.
Paper Stock - Same as for Cut Sheet.
Ink Color - Same as for Cut Sheet (OCR-Red Ink) must be in Flint J-6983 Red OCR
“dropout” ink or an exact match.
Titles - Color of any titles if applicable: Are to be in the same ink as the form, Flint J6983
OCR Red “dropout” ink.
Symbol - The identifiable 1500 in a rectangle located in the upper left front of the form
above the PICA boxes is to be in black ink.
Perforations - Marginally 0.5 inch left and right, tear line horizontally every 11 inches.
Two Part Marginally Punched Continuous Forms:
Size - Same dimensions as for Cut Sheet, plus 0.5 inch left and right, (overall: 9.5 by 11
inches, detached: 8.5 by 11 inches).
Print -
Part 1 -Face and back, head to head.
Part 2 -Face and back, head to head.
Margins - On detached sheet, same as for Cut Sheet.
Askewity - On detached sheet, same as for Cut Sheet.
Paper Stock -
Part 1 - Carbonless, 20 CB - Recycled White
Part 2 - Any color or weight that does not interfere with scanning of part 1 sheet. Suggest
the following sequence:
Paper Weight:
1st part is 20 CB - OCR Bond

2nd part is 14 CFB (if not last part)
Last part is 15CF
CB = Coated Back (Carbonless black print)
CFB = Coated Front and Back (Carbonless black print)
CF = Coated Front (Carbonless black print)
Ink color -
Part 1 - Same as for cut sheet, (OCR-Red Ink) must be in Flint J-6983 Red OCR
“dropout” ink or an exact match.
Part 2 - Any color that will not interfere with scanning of the part 1 sheet.
Titles - Color of any titles if applicable: Are to be in the same ink as the form, Flint J6983
OCR Red “dropout” ink.
Symbol - The identifiable 1500 in a rectangle located in the upper left front of the form
above the PICA boxes is to be in black ink.
Joining - Crimp left and right.
Perforations - Marginally 0.5 inch left and right, tear line horizontally every 11”.
NOTE: Users may determine the number of parts that are applicable to their needs. Up
to four total parts are feasible on some printers; some other printers may limit the
readability of multiple plies. Color of any titles if applicable: Are to be in the same ink
as the form, Flint J6983 OCR Red “dropout” ink.
Symbol: NUCC requires the use of an approved Form CMS-1500 in the formats
provided displaying the 1500 symbol as approved by the NUCC. All printing of Form
CMS-1500 must occur in accordance with the NUCC requirements.
Form Name - CMS-1500 Health Insurance Paper Claim Form, Approved by the National
Uniform Claims Committee (NUCC).
Form Identification: The lower right-hand margin contains the approved OMB numbers
and should be consistent throughout.
No modification is to be made to the Form CMS-1500 (08-05) without prior approval
from the NUCC and CMS.

Exhibit 1
(Rev. 1970, 05-21-10)
Form CMS-1500 (08/05) User Print File Specifications (Formerly Exhibit 2)
LINE FIELD LITERAL
FIELD
TYPE*
BYTES
COL-
UMNS
1
Left printer alignment block
M
3
01-03
1
Right printer alignment block M 3 77-79
3 1 Medicare M 1 01
3 1 Medicaid M 1 08
3 1 Tricare Champus M 1 15
3
1
Champva
M
1
24
3 1 Group Health Plan M 1 31
3 1 FECA Blk Lung M 1 39
3 1 Other M 1 45
3 1a Insured's ID Number A/N 29 50-78
5
2
Patient's Name (Last, First, MI)
A
28
01-28
5 3 Patient's Birth Date (Month) N 2 31-32
5 3 Patient's Birth Date (Day) N 2 34-35
5 3 Patient's Birth (Year) N 4 37-40
5 3 Sex-Male M 1 42
5
3
Sex-Female
M
1
47
5 4 Insured Name (Last, First, MI) A 29 50-78
7 5 Patient's Address A/N 28 01-28
7 6 Patient Relationship to Insured (Self) M 1 33
7 6 Patient Relationship to Insured (Spouse) M 1 38
7
6
Patient Relationship to Insured (Child)
M
1
42
7 6 Patient Relationship to Insured (Other) M 1 47
7 7 Insured's Address A/N 29 50-78
9 5 Patient's City A 24 01-24
* M = mark (X), A = alpha, N = numeric
9
5
Patient's State
A
3
26-28
9 8 Patient Status (Single) M 1 35

LINE FIELD LITERAL
FIELD
TYPE*
BYTES
COL-
UMNS
9 8 Patient Status (Married) M 1 41
9 8 Patient Status (Other) M 1 47
9 7 Insured's City A 23 50-72
9 7 Insured's State A 4 74-77
11 5 Patient's ZIP Code N 12 01-12
11 5 Patient's Area Code N 3 15-17
11 5 Patient's Phone Number N 10 19-28
11
8
Patient Status (Employed)
M
1
35
11
8
Patient Status (Full Time Student)
M
1
41
11 8 Patient Status (Part Time Student) M 1 47
11 7 Insured's ZIP Code N 12 50-61
11 7 Insured's Area Code N 3 65-67
11 7 Insured's Phone Number N 10 69-78
13 9 Other Insured's Name (Last, First, MI) A 28 01-28
13 11 Insured's Policy, Group or FECA
Number
A/N 29 50-78
15 9a Other Insured's Policy or Group
Number
A/N 28 01-28
15 10a Condition Related (Employment C/P,
Yes)
M 1 35
15 10a Condition Related (Employment C/P,
No)
M 1 41
15 11a Insured's Date of Birth (Month) N 2 53-54
15
11a
Insured's Date of Birth (Day)
N
2
56-57
15
11a
Insured's Date of Birth (Year)
N
4
59-62
15 11a Sex-Male M 1 68
15 11a Sex-Female M 1 75
17 9b Other Insured's Date of Birth (Month) N 2 02-03
* M = mark (X), A = alpha, N = numeric
17 9b Other Insured's Date of Birth (Day) N 2 05-06
17 9b Other Insured's Date of Birth (Year) N 4 08-11

LINE FIELD LITERAL
FIELD
TYPE*
BYTES
COL-
UMNS
17 9b Sex-Male M 1 18
17
9b
Sex-Female
M
1
24
17
10b
Condition Related To: (Auto Accident-
Yes)
M
1
35
17
10b
Condition Related To: (Auto Accident-
No)
M
1
41
17 10b Condition Related To: (Auto Accident-
State)
A 2 45-46
17 11b Insured's Employer's Name or School
Name
A/N 29 50-78
19 9c Other Insured's Employer's Name or
School
A/N 28 01-28
19 10c Other Accident (Yes) M 1 35
19 10c Other Accident (No) M 1 41
19 11c Insured's Insurance Plan or PayerID A/N 29 50-78
21 9d
Other Insured’s Plan Name or Payer
ID
A/N 28 01-28
21 10d (Reserved for Local Use) A/N 19 30-48
21 11d Another Benefit Health Plan (Yes) M 1 52
21 11d Another Benefit Health Plan (No) M 1 57
25
12
Left Blank for Patient's Signature & Date
25 13 Left Blank for Insured's Signature
27 14 Date of Current Illness, Injury,
Pregnancy (Month)
N 2 02-03
27 14 Date of Current Illness, Injury,
Pregnancy (Day)
N 2 05-06
27 14 Date of Current Illness, Injury,
Pregnancy - (Year)
N 4 08-11
27 15 First Date Has Had Same or Similar
Illness (Month)
N 2 37-38
* M = mark (X), A = alpha, N = numeric
27 15 First Date Has Had Same or Similar
Illness (Day)
N 2 40-41
27 15 First Date Has Had Same or Similar
Illness - (Year)
N 4 43-46

LINE FIELD LITERAL
FIELD
TYPE*
BYTES
COL-
UMNS
27 16 Dates Patient Unable to Work (From
Month)
N
2 54-55
27 16 Dates Patient Unable to Work (From
Day)
N
2 57-58
27
16
Dates Patient Unable to Work (From
Year)
N
4
60-63
27
16
Dates Patient Unable to Work (To
Month)
N
2
68-69
27 16 Dates Patient Unable to Work (To Day)
N
2 71-72
27 16
Dates Patient Unable to Work (To
Year)
N
4 74-787
28 17a Legacy Qualifier/Provider Number of
Referring Physician
A/N 19 30-48
29 17 Name of Referring Physician or Other
Source
A 26 01-26
29 17b NPI Number of Referring Physician N 17 32-48
29 18 Hospitalization Related Current Svcs
(From Month)
N 2 54-55
29 18 Hospitalization Related Current Svcs
(From Day)
N 2 57-58
29 18 Hospitalization Related Current Svcs
(From Year)
N 4 60-63
29 18 Hospitalization Related Current Svcs
(To Month)
N 2 68-69
29 18 Hospitalization Related Current Svcs
(To Day)
N 2 71-72
29 18 Hospitalization Related Current Svcs
(To Year)
N
30 19 Reserved for Local Use A/N 35 14-48
31 19 Reserved for Local Use A/N 48 01-48
31 20 Outside Lab (Yes) M 1 52
* M = mark (X), A = alpha, N = numeric
31 20 Outside Lab (No) M 1 57
31 20 $ Charges N 8/8 62-78

LINE FIELD LITERAL
FIELD
TYPE*
BYTES
COL-
UMNS
33 21.1 Diagnosis or Nature of Illness or Injury
(Code)
A/N 8 03-10
33 21.3 Diagnosis or Nature of Illness or Injury
(Code)
A/N 8 30-37
33
22
Medicaid Resubmission Code
A/N
11
50-60
33 22.2 Original Reference Number A/N 18 61-78
35 21.2 Diagnosis or Nature of Illness or Injury
(Code)
A/N 8 03-10
35 21.4 Diagnosis or Nature of Illness or Injury
(Code)
A/N 8 30-37
35 23 Prior Authorization Number A/N 29 50-78
38 24 Line Detail Narrative A/N 63 01-63
38 24.1i Legacy Qualifier Rendering Provider A/N 2 65-66
38 24.1j Legacy Provider Number Rendering
Provider
A/N 11 68-78
39 24.1a Date(s) of Service - (From Month) N 2 01-02
39 24.1a Date(s) of Service - (From Day) N 2 04-05
39 24.1a Date(s) of Service - (From Year) N 2 07-08
39 24.1a Date(s) of Service - (To Month) N 2 10-11
39
24.1a
Date(s) of Service - (To Day)
N
2
13-14
39
24.1a
Date(s) of Service - (To Year)
N
2
16-17
39 24.1b Place of Service A/N 2 19-20
39 24.1c EMG A 2 22-23
39 24.1d Procedures, Svcs or Supplies
(CPT/HCPCS)
A/N 6 25-30
39 24.1d Procedures, Svcs or Supplies (Modifier
1)
A/N 2 33-34
39 24.1d Procedures, Svcs or Supplies (Modifier
2)
A/N 2 36-37
39 24.1d Procedures, Svcs or Supplies (Modifier
3)
A/N 2 39-40
39
24.1d
Procedures, Svcs or Supplies (Modifier
4)
A/N
2
42-43
* M = mark (X), A = alpha, N = numeric
39 24.1e Diagnosis Pointer N 4 45-48
39 24.1f $ Charges N 8 50-57

LINE FIELD LITERAL
FIELD
TYPE*
BYTES
COL-
UMNS
39 24.1g Days or Units N 3 59-61
39
24.1h
EPSDT Family Plan
A
1
63
39
24.li
Legacy Qualifier Rendering Provider
(Leave Blank)
A/N
0
39
24.1j
Legacy Provider Number Rendering
Provider
A/N
11
68-78
40 24 Line Detail Narrative A/N 63 01-63
40 24.2i Legacy Qualifier Rendering Provider A/N 2 65-66
40 24.2j Legacy Provider Number Rendering
Provider
A/N 11 68-78
41 24.2a Date(s) of Service - (From Month) N 2 01-02
41 24.2a Date(s) of Service - (From Day) N 2 04-05
41 24.2a Date(s) of Service - (From Year) N 2 07-08
41 24.2a Date(s) of Service - (To Month) N 2 10-11
41 24.2a Date(s) of Service - (To Day) N 2 13-14
41
24.2a
Date(s) of Service - (To Year)
N
2
16-17
41
24.2b
Place of Service
A/N
2
19-20
41 24.2c EMG A 2 22-23
41 24.2d Procedures, Svcs or Supplies
(CPT/HCPCS)
A/N 6 25-30
41 24.2d Procedures, Svcs or Supplies (Modifier
1)
A/N 2 33-34
41 24.2d Procedures, Svcs or Supplies (Modifier
2)
A/N 2 36-37
41 24.2d Procedures, Svcs or Supplies (Modifier
3)
A/N 2 39-40
41 24.2d Procedures, Svcs or Supplies (Modifier
4)
A/N 2 42-43
41 24.2e Diagnosis Pointer N 4 45-48
41 24.2f $ Charges N 8 50-57
41 24.2g Days or Units N 3 59-61
41 24.2h EPSDT Family Plan A 1 63
* M = mark (X), A = alpha, N = numeric
41 24.2i Legacy Qualifier Rendering Provider
(Leave Blank)
A/N 0

LINE FIELD LITERAL
FIELD
TYPE*
BYTES
COL-
UMNS
41 24.2j Legacy Provider Number Rendering
Provider
A/N 11 68-78
42 24 Line Detail Narrative A/N 63 01-63
42 24.3i Legacy Qualifier Rendering Provider A/N 2 65-66
42
24.3j
Legacy Provider Number Rendering
Provider
A/N
11
68-78
43 24.3a Date(s) of Service - (From Month) N 2 01-02
43 24.3a Date(s) of Service - (From Day) N 2 04-05
43 24.3a Date(s) of Service - (From Year) N 2 07-08
43 24.3a Date(s) of Service - (To Month) N 2 10-11
43 24.3a Date(s) of Service - (To Day) N 2 13-14
43 24.3a Date(s) of Service - (To Year) N 2 16-17
43 24.3b Place of Service A/N 2 19-20
43 24.3c EMG A 2 22-23
43
24.3d
Procedures, Svcs or Supplies
(CPT/HCPCS)
A/N
6
25-30
43
24.3d
Procedures, Svcs or Supplies (Modifier
1)
A/N
2
33-34
43 24.3d Procedures, Svcs or Supplies (Modifier
2)
A/N 2 36-37
43 24.3d Procedures, Svcs or Supplies (Modifier
3)
A/N 2 39-40
43 24.3d Procedures, Svcs or Supplies (Modifier
4)
A/N 2 42-43
43 24.3e Diagnosis Pointer N 4 45-48
43 24.3f $ Charges N 8 50-57
43 24.3g Days or Units N 3 59-61
43
24.3h
EPSDT Family Plan
A
1
63
43 24.3i Legacy Qualifier Rendering Provider
(Leave Blank)
A/N 0
43 24.3j Legacy Provider Number Rendering
Provider
A/N 11 68-78
44
24
Line Detail Narrative
A/N
63
01-63
* M = mark (X), A = alpha, N = numeric
44 24.4i Legacy Qualifier Rendering Provider A/N 2 65-66

LINE FIELD LITERAL
FIELD
TYPE*
BYTES
COL-
UMNS
44 24.4j Legacy Provider Number Rendering
Provider
A/N 11 68-78
45 24.4a Date(s) of Service - (From Month) N 2 01-02
45 24.4a Date(s) of Service - (From Day) N 2 04-05
45
24.4a
Date(s) of Service - (From Year)
N
2
07-08
45 24.4a Date(s) of Service - (To Month) N 2 10-11
45 24.4a Date(s) of Service - (To Day) N 2 13-14
45 24.4a Date(s) of Service - (To Year) N 2 16-17
45 24.4b Place of Service A/N 2 19-20
45 24.4c EMG A 2 22-23
45 24.4d Procedures, Svcs or Supplies
(CPT/HCPCS)
A/N 6 25-30
45 24.4d Procedures, Svcs or Supplies (Modifier
1)
A/N 2 33-34
45 24.4d Procedures, Svcs or Supplies (Modifier
2)
A/N 2 36-37
45
24.4d
Procedures, Svcs or Supplies (Modifier
3)
A/N
2
39-40
45
24.4d
Procedures, Svcs or Supplies (Modifier
4)
A/N
2
42-43
45 24.4e Diagnosis Pointer N 4 45-48
45 24.4f $ Charges N 8 50-57
45 24.4g Days or Units N 3 59-61
45 24.4h EPSDT Family Plan A 1 63
45 24.4i Legacy Qualifier Rendering Provider
Blank) (Leave
A/N 0
45 24.4j Legacy Provider Number Rendering
Provider
A/N 11 68-78
46 24 Line Detail Narrative A/N 63 01-63
46 24.5i Legacy Qualifier Rendering Provider A/N 2 65-66
46 24.5j Legacy Provider Number Rendering
Provider
A/N 11 68-78
47
24.5a
Date(s) of Service - (From Month)
N
2
01-02
* M = mark (X), A = alpha, N = numeric
47 24.5a Date(s) of Service - (From Day) N 2 04-05

LINE FIELD LITERAL
FIELD
TYPE*
BYTES
COL-
UMNS
47 24.5a Date(s) of Service - (From Year) N 2 07-08
47
24.5a
Date(s) of Service - (To Month)
N
2
10-11
47
24.5a
Date(s) of Service - (To Day)
N
2
13-14
47 24.5a Date(s) of Service - (To Year) N 2 16-17
47 24.5b Place of Service A/N 2 19-20
47 24.5c EMG A 2 22-23
47 24.5d Procedures, Svcs or Supplies
(CPT/HCPCS)
A/N 6 25-30
47 24.5d Procedures, Svcs or Supplies (Modifier
1)
A/N 2 33-34
47 24.5d Procedures, Svcs or Supplies (Modifier
2)
A/N 2 36-37
47 24.5d Procedures, Svcs or Supplies (Modifier
3)
A/N 2 39-40
47 24.5d Procedures, Svcs or Supplies (Modifier
4)
A/N 2 42-43
47
24.5e
Diagnosis Pointer
N
4
45-48
47
24.5f
$ Charges
N
8
50-57
47 24.5g Days or Units N 3 59-61
47 24.5h EPSDT Family Plan A 1 63
47 24.5i Legacy Qualifier Rendering Provider
(Leave Blank)
A/N 0
47 24.5j Legacy Provider Number Rendering
Provider
A/N 11 68-78
48 24 Line Detail Narrative A/N 63 01-63
48 24.6i Legacy Qualifier Rendering Provider A/N 2 65-66
48 24.6j Legacy Provider Number Rendering
Provider
A/N 11 68-78
49 24.6a Date(s) of Service - (From Month) N 2 01-02
49 24.6a Date(s) of Service - (From Day) N 2 04-05
49 24.6a Date(s) of Service - (From Year) N 2 07-08
49
24.6a
Date(s) of Service - (To Month)
N
2
10-11
49 24.6a Date(s) of Service - (To Day) N 2 13-14
* M = mark (X), A = alpha, N = numeric
49 24.6a Date(s) of Service - (To Year) N 2 16-17

LINE FIELD LITERAL
FIELD
TYPE*
BYTES
COL-
UMNS
49 24.6b Place of Service A/N 2 19-20
49
24.6c
EMG
A
2
22-23
49
24.6d
Procedures, Svcs or Supplies
(CPT/HCPCS)
A/N
6
25-30
49
24.6d
Procedures, Svcs or Supplies (Modifier
1)
A/N
2
33-34
49 24.6d Procedures, Svcs or Supplies (Modifier
2)
A/N 2 36-37
49 24.6d Procedures, Svcs or Supplies (Modifier
3)
A/N 2 39-40
49 24.6d Procedures, Svcs or Supplies (Modifier
4)
A/N 2 42-43
49 24.6e Diagnosis Pointer N 4 45-48
49 24.6f $ Charges N 8 50-57
49 24.6g Days or Units N 3 59-61
49
24.6h
EPSDT Family Plan
A
1
63
49
24.6i
Legacy Qualifier Rendering Provider
(Leave Blank)
A/N
0
49
24.6j
Legacy Provider Number Rendering
Provider
A/N
11
68-78
51
25
Federal Tax ID Number
N
15
1-15
51 25 Federal Tax ID Number (SSN) M 1 17
51 25 Federal Tax ID Number (EIN) M 1 19
51 26 Patient's Account Number A/N 14 23-36
51 27 Accept Assignment (Yes) M 1 38
51 27 Accept Assignment (No) M 1 43
51 28 Total Charge N 9 51-59
51 29 Amount Paid N 8 62-69
51 30 Balance Due N 8 71-78
52 33 Billing Provider Phone Number Area
Code
N 3 66-68
52
33
Billing Provider Phone Number
N
9
70-78
* M = mark (X), A = alpha, N = numeric
53 32 Name of Facility Where Svcs Rendered A/N 26 23-48

LINE FIELD LITERAL
FIELD
TYPE*
BYTES
COL-
UMNS
53 33 Physician/Supplier Billing Name A/N 29 50-78
54
32
Address of Facility Where Svcs
Rd d
A/N
26
23-48
54 33 Physician/Supplier Address A/N 29 50-78
55 31 Left Blank for Signature
Physician/Supplier
55 32 City, State and ZIP Code of Facility A/N 26 23-48
55 33 City, State and ZIP Code of Billing
P id
A/N 29 50-78
56 32a Facility NPI Number N 10 24-33
56 32b Facility Qualifier and Legacy Number A/N 14 35-48
56 33a Billing Provider NPI Number N 10 51-60
56 33b Billing Provider Qualifier and Legacy
Nb
A/N 17 62-78
* M = mark (X), A = alpha, N = numeric

Transmittals Issued for this Chapter
Rev # Issue Date
Subject Impl Date CR#
R12671CP
06/06/2024
Billing and Payment for Telehealth Services
with Place of Service (POS) 10
07/08/2024
13582
R12456CP
01/11/2024
New Physician Specialty Code for
Epileptologists
07/01/2024
13425
R12411CP
12/14/2023
New Place of Service (POS) Code 27 -
"Outreach Site/Street”
01/02/2024
13314
R12254CP
09/20/2023
New Place of Service (POS) Code 27 -
"Outreach Site/Street” – Rescinded and
Replaced by Transmittal 12411
01/02/2024
13314
R12231CP
08/31/2023
New Dental Specialty Codes for Medicare 01/02/2024
13323
R12202CP
08/10/2023
New Place of Service (POS) Code 27 -
"Outreach Site/Street” – Rescinded and
Replaced by Transmittal 12254
01/02/2024
13314
R11437CP
05/27/2022
New/Modifications to the Place of Service
(POS) Codes for Telehealth
04/04/2022
12427
R11045CP
10/13/2021
New/Modifications to the Place of Service
(POS) Codes for Telehealth- Rescinded and
Replaced by Transmittal 4472
04/04/2022
12427
R10341CP
09/04/2020
Internet Only Manual Update to Pub. 100-
04, Chapter 16, Section 60.1.2 and Pub.
100-04, Chapter 26, Section 10.4, Item 19
10/06/2020
11935
R10124CP
05/08/2020
New Physician Specialty Code for
Micrographic Dermatologic Surgery (MDS)
and Adult Congenital Heart Disease
(ACHD) and a New Supplier Specialty
Code for Home Infusion Therapy Services
10/05/2020
11750
12/05/2019
New Medicare Provider Specialty Code
(D5) and Billing Codes for Opioid
Treatment Programs and New Place of
Service Code 58
01/06/2020
11353

Rev # Issue Date
Subject Impl Date CR#
R4388CP 09/06/2019
Manual Updates to Chapters 1, 22, 24, 26,
and 31 in Publication (Pub.) 100-04
10/07/2019
11331
08/01/2019
New Medicare Provider Specialty Code
(D5) and Billing Codes for Opioid
Treatment Programs and New Place of
Service Code 58 – Rescinded and Replaced
by Transmittal 4472
01/06/2020
11353
R4232CP 02/08/2019
Update to Publication (Pub.) 100-04
Chapter 26 to Provide Language-Only
Changes for the New Medicare Card Project
03/12/2019
11129
R4184CP 12/20/2018
New Physician Specialty Code for Undersea
and Hyperbaric Medicine
01/07/2019
10666
R4039CP 04/27/2018
New Physician Specialty Code for Medical
Genetics and Genomics
10/01/2018
10457
R3873CP 10/06/2017
Place of Service Codes 04/02/2018
10272
R3881CP 10/13/2017
Clinical Laboratory Fee Schedule Not
Otherwise Classified, Not Otherwise
Specified, or Unlisted Service or Procedure
Code Data Collection
01/16/2018
10232
R3762CP 04/28/2017
New Physician Specialty Code for
Advanced Heart Failure and Transplant
Cardiology, Medical Toxicology, and
Hematopoietic Cell Transplantation and
Cellular Therapy
10/02/2017
9957
R3637CP 10/28/2016
New Physician Specialty Code for
Hospitalist
04/03/2017
9716
R3586CP 08/12/2016
New Place of Service (POS) Code for
Telehealth and Distant Site Payment Policy
01/03/2017
9726
R3547CP 06/22/2016
New Physician Specialty Code for Dentist 07/05/2016
9355

Rev # Issue Date
Subject Impl Date CR#
R3544CP 06/15/2016
New Physician Specialty Code for Dentist -
Rescinded and replaced by Transmittal
3547
07/05/2016
9355
R3490CP 04/01/2016
Medicare Internet Only Manual Publication
100-04 Chapter 26 - Completing and
Processing Form CMS-1500 Data Set
04/25/2016
9344
R3484CP 03/25/2016
Medicare Internet Only Manual Publication
100-04 Chapter 26 - Completing and
Processing Form CMS-1500 Data Set -
Rescinded and replaced by Transmittal
3490
04/25/2016
9344
R3447CP 01/29/2016
New Physician Specialty Code for Dentist –
Rescinded and replaced by Transmittal
3544
07/05/2016
9355
R3315CP 08/06/2015
New and Revised Place of Service Codes
(POS) for Outpatient Hospital
01/04/2016
9231
R3255CP 05/08/2015
Correction to the Multi-Carrier System
(MCS) Editing on the Service Location
National Provider Identifier (NPI) Reported
for Anti-Markup and Reference Laboratory
Claims
10/05/2015
9150
R3177CP 01/30/2015
Updating CMS IOM 100-04, Chapter 26
with Specialty Code B1
03/02/2015
9001
R3103CP 11/03/2014
Reporting the Service Location National
Provider Identifier (NPI) on Anti-Markup
and Reference Laboratory Claims
04/06/2015
8806
R3098CP 10/21/2014
Reporting the Service Location National
Provider Identifier (NPI) on Anti-Markup
and Reference Laboratory Claims –
Rescinded and replaced by Transmittal
3103
04/05/2014
8806

Rev # Issue Date
Subject Impl Date CR#
R3083CP 10/02/2014
Form CMS-1500 Instructions: Revised for
Form Version 02/12
01/06/2014
8509
R3073CP 09/23/2014
New Physician Specialty Code for
Interventional Cardiology
01/05/2015
8812
R3061CP 09/04/2014
New Physician Specialty Code for
Interventional Cardiology – Rescinded and
replaced by Transmittal 3073
01/05/2015
8812
R3048CP 08/22/2014
New Physician Specialty Code for
Interventional Cardiology – Rescinded and
replaced by Transmittal 3061
01/05/2015
8812
R3047CP 08/22/2014
Reporting the Service Location National
Provider Identifier (NPI) on Anti-Markup
and Reference Laboratory Claims –
Rescinded and replaced by Transmittal
3098
01/05/2014
8806
R2984CP 07/11/2014
Beneficiary Signature Requirements for
Ambulance Services
08/12/2014
8760
R2842CP 12/27/2013
Form CMS-1500 Instructions: Revised for
Form Version 02/12 – Rescinded and
replaced by Transmittal 3083
01/06/2014
8509
R2814CP 11/15/2013
2014 Annual Type of Service (TOS) Update
01/06/2014
8519
R2744CP 07/24/2013
Type of Service (TOS) Corrections 2013 10/07/2013
8392
R2738CP 07/12/2013
Type of Service (TOS) Corrections 2013 –
Rescinded and replaced by Transmittal
2744
10/07/2013
8392
R2721CP 06/12/2013
New Non-Physician Specialty Code for
Complimentary Insurer
10/07/2013
8282
R2697CP 05/03/2013
New Non-Physician Specialty Code for
Complimentary Insurer – Rescinded and
replaced by Transmittal 2721
10/07/2013
8282
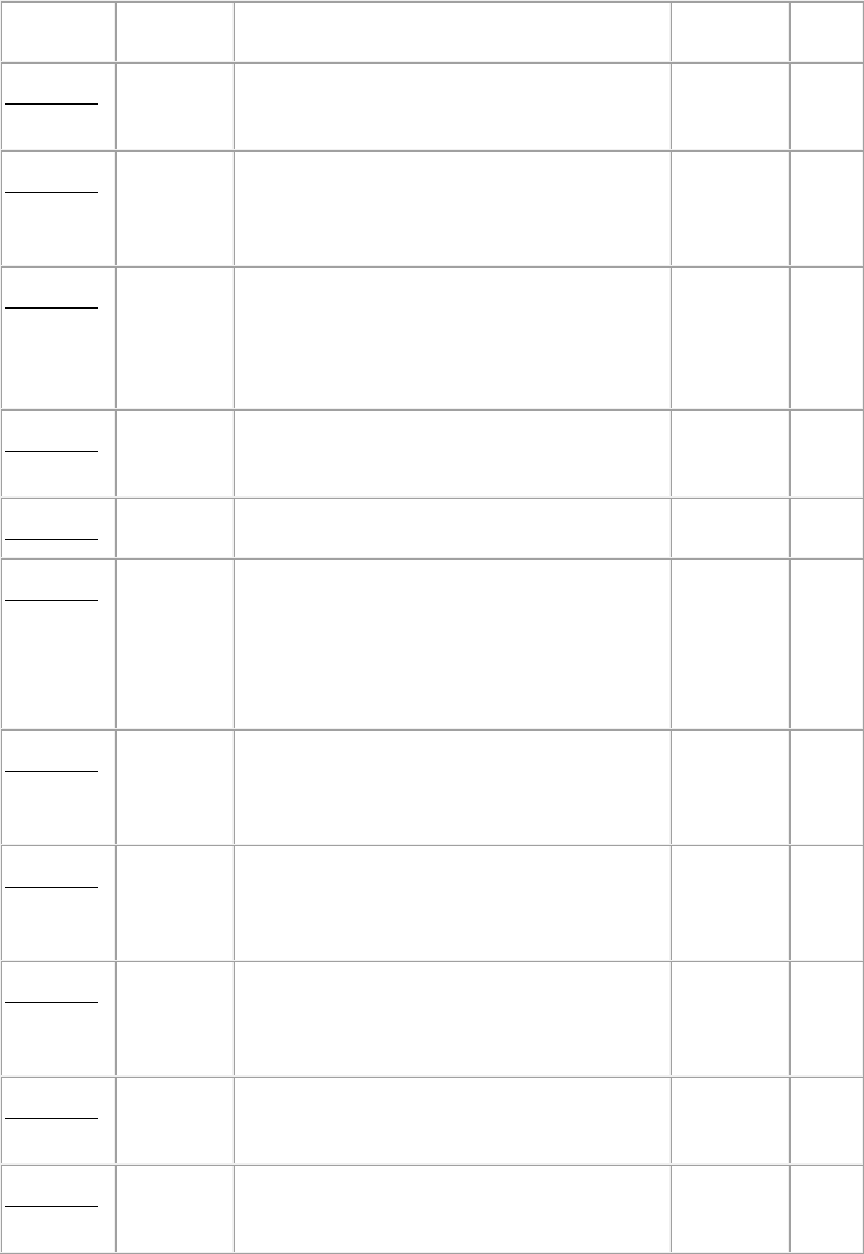
Rev # Issue Date
Subject Impl Date CR#
R2679CP 03/29/2013
Revised and Clarified Place of Service
(POS) Coding Instructions
04/01/2013
7631
R2613CP 12/14/2012
Revised and Clarified Place of Service
(POS) Coding Instructions – Rescinded and
replaced by Transmittal 2679
04/01/2013
7631
R2614CP 12/14/2012
Updated Billing Requirements for
Outpatient Therapy Services -- Middle
Class Tax Relief and Jobs Creation Act
(MCTRJCA) of 2012
11/27/2012
8097
R2602CP 11/30/2012
New Place of Service (POS) Code for Place
of Employment/Worksite
04/01/2013
8125
R2598CP 11/23/2012
Annual Type of Service (TOS) Update 01/07/2013
8082
R2571CP 10/26/2012
Updated Billing Requirements for
Outpatient Therapy Services –
Middle Class
Tax Relief and Jobs Creation Act
(MCTRJCA) of 2012 – Rescinded and
replaced by Transmittal 2614
11/27/2012
8097
R2570CP 10/26/2012
Annual Type of Service (TOS) Update –
Rescinded and replaced by Transmittal
2598
01/07/2013
8082
R2563CP 10/11/2012
Revised and Clarified Place of Service
(POS) Coding Instructions – Rescinded and
replaced by Transmittal 2613
04/01/2013
7631
R2561CP 09/28/2012
Revised and Clarified Place of Service
(POS) Coding Instructions – Rescinded and
replaced by Transmittal 2563
04/01/2013
7631
R2516CP 08/10/2012
New Non-Physician Specialty Code for
Centralized Flu
01/07/2013
7884
R2462CP 04/27/2012
New Physician Specialty Code for Sleep
Medicine and Sports Medicine
10/01/2012
7600

Rev # Issue Date
Subject Impl Date CR#
R2435CP 03/29/2012
Revised and Clarified Place of Service
(POS) Coding Instructions – Rescinded and
replaced by Transmittal 2561
10/01/2012
7631
R2407CP 02/03/2012
Revised and Clarified Place of Service
(POS) Coding Instructions – Rescinded and
replaced by Transmittal 2435
04/02/2012
7631
R2375CP 12/22/2011
Annual Type of Service (TOS) Update 01/03/2012
7586
R2325CP 10/26/2011
Annual Type of Service (TOS) Update –
Rescinded and replaced by Transmittal
2375
01/03/2012
7586
R2284CP 08/26/2011
Clarification to Chapter 26, Section 10-4-
Items 14-33-
Provider of Service or Supplier
Information
09/26/2011
7538
R2261CP 07/29/2011
Affordable Care Act – Section 3113 –
Laboratory Demonstration for Certain
Complex Diagnostic Tests (This CR fully
rescinds and replaces CR 7413)
01/03/2012
7516
R2248CP 06/24/2011
New Specialty Code for Advanced
Diagnostic Imaging Accreditation
04/01/2011
7175
R2226CP 05/20/2011
Affordable Care Act-Section 3113-
Laboratory Demonstration for Certain
Complex Diagnostic Tests (This CR fully
rescinds and replaces CR 7278) – This CR
rescinded and replaced by CR 7516,
Transmittal 2261
01/03/2012
7413
R2204CP 04/29/2011
Type of Service (TOS) Corrections 10/03/2011
7407
R2192CP 04/12/2011
New Specialty Code for Advanced
Diagnostic Imaging Accreditation –
Rescinded and replaced by Transmittal
2248
07/05/2011
7175

Rev # Issue Date
Subject Impl Date CR#
R2191CP 04/08/2011
New Specialty Code for Advanced
Diagnostic Imaging Accreditation –
Rescinded and replaced by Transmittal
2192
07/05/2011
7175
R2173CP 03/11/2011
Affordable Care Act – Section 3113 –
Laboratory Demonstration for Certain
Complex Diagnostic Tests – Rescinded and
replaced by CR 7413, Transmittal 2226
7/05/2011 7278
R2162CP 02/22/2011
Updates to the Internet Only Manual Pub.
100-04, Chapter 1 - General Billing
Requirements, Chapter 15 - Ambulance,
and Chapter 26 - Completing and
Processing Form CMS-1500 Data Set
03/21/2011
7018
R2144CP 01/28/2011
Affordable Care Act – Section 3113 –
Laboratory Demonstration for Certain
Complex Diagnostic Tests – Rescinded and
replaced by Transmittal 2173
7/05/2011 7278
R2126CP 12/23/2010
Annual Type of Service (TOS) Update 01/03/2011
7185
R2124CP 12/23/2010
Updates to the Internet Only Manual Pub.
100-04, Chapter 1 - General Billing
Requirements, Chapter 15 - Ambulance,
and Chapter 26 - Completing and
Processing Form CMS-1500 Data Set -
Rescinded and replaced by Transmittal
2162
01/25/2011
7018
R2103CP 11/19/2010
Fractional Mileage Units Submitted on
Ambulance Claims
01/03/2011
7065
R2098CP 11/19/2011
New Physician Specialty Codes for Cardiac
Electrophysiology and Sports Medicine
04/04/2011
7209
R2079CP 10/29/2010
New Specialty Code for Advanced
Diagnostic Imaging Accreditation –
Rescinded and replaced by Transmittal
2191
04/04/2011
7175

Rev # Issue Date
Subject Impl Date CR#
R2072CP 10/22/2010
Annual Type of Service (TOS) Update –
Rescinded and replaced by Transmittal
2126
01/03/2011
7185
R2065CP 10/15/2010
Fractional Mileage Units Submitted on
Ambulance Claims – Rescinded and
replaced by Transmittal 2103
01/03/2011
7065
R2041CP 08/31/2010
Revisions to Claims Processing Instructions
for Services Rendered in Place of Service
Home
01/03/2011
6947
R2035CP 08/27/2010
Change Physician Specialty Code 12 to
Osteopathic Manipulative Medicine
01/03/2011
6890
R2030CP 08/20/2010
New Durable Medical Equipment,
Prosthetics. Orthotics, and Supplies
(DMEPOS) Specialty Code for Ocularists
01/03/2011
6891
R2029CP 08/13/2010
Fractional Mileage Units Submitted on
Ambulance Claims – Rescinded and
replaced by Transmittal 2065
01/03/2011
7065
R2015CP 07/30/2010
Revisions to Claims Processing Instructions
for Services Rendered in Place of Service
Home - Rescinded and replaced by
Transmittal 2041.
01/03/2011
6947
R2003CP 07/19/2010
New Physician Specialty Code for Geriatric
Psychiatry
04/05/2010
6533
R1974CP 05/21/2010
Cardiac Rehabilitation and Intensive
Cardiac Rehabilitation
10/04/2010
6850
R1970CP 05/21/2010
Updated Form CMS-1500 Information 10/04/2010
6929
R1931CP 03/12/2010
Revision of the Internet Only Manual
(IOM) to Remove References to “Purchased
Diagnostic Test” and Replace With
Language Consistent With the Anti-
Markup
Rule
06/14/2010
6627

Rev # Issue Date
Subject Impl Date CR#
R1910CP 02/05/2010
Type of Service (TOS) Corrections 04/05/2010
6835
R1873CP 12/11/2009
Place of Service (POS) and Date of Service
(DOS) Instructions for the Interpretation
(Professional Component) and Technical
Component of Diagnostic Tests - Rescinded
01/04/2010
6375
R1869CP 12/11/2009
New Place of Service (POS) Code for
Walk-in Retail Health Clinic
03/11/2010
6752
R1836CP 10/27/2009
New Physician Specialty Code for Geriatric
Psychiatry – Rescinded and replaced by
Transmittal 2003
04/05/2010
6533
R1830CP 10/16/2009
Annual Type of Service (TOS) Update 01/04/2010
6693
R1823CP 10/02/2009
Place of Service (POS) and Date of Service
(DOS) Instructions for the Interpretation
(Professional Component) and Technical
Component of Diagnostic Tests –
Rescinded and replaced by Transmittal
1873
01/04/2010
6375
R1806CP 08/28/2009
October 2009 Update to the Ambulatory
Surgical Center (ASC) Payment System;
Summary of Payment Policy Changes
10/05/2009
6629
R1725CP 05/01/2009
Requirements for Specialty Codes 07/06/2009
6303
R1715CP 04/24/2009
New Physician Specialty Code for Hospice
and Palliative Care
10/05/2009
6311
R1686CP 02/20/2009
New Non-Physician Practitioner Specialty
Code for Speech Language Pathologists
07/06/2009
6292
R1638CP 11/20/2008
Annual Type of Service (TOS) Update 01/05/2009
6272
R1637CP 11/14/2008
Annual Type of Service (TOS) Update -
Rescinded and replaced by Transmittal
1638
01/05/2009
6272

Rev # Issue Date
Subject Impl Date CR#
R1586CP 09/05/2008
Pneumococcal Pneumonia, Influenza Virus,
and Hepatitis B Vaccines
10/06/2008
6079
R1552CP 07/18/2008
VMS Recognition of New Specialty Codes
for Suppliers of Durable Medical
Equipment, Prosthetics, Orthotics and
Supplies (DMEPOS) With Pedorthic
Personnel, Medical Supply Companies With
Pedorthic Personnel, and Rehabilitation
Agencies. (DME MACs Only)
01/05/2009
5930
R1481CP 03/21/2008
Type of Service (TOS) Corrections 04/07/2008
5977
R1432CP 02/01/2008
Medicare Fee for Service Legacy Provider
IDs Prohibited on Form CMS-1500 and
Form CMS-1450 (UB-04) Claims
04/07/2008
5858
R1420CP 01/25/2008
Clarification Regarding the Coordination of
Benefits Agreement (COBA) Medigap
Claim-Based Crossover Process
02/01/2008
5837
R1412CP 01/11/2008
Reporting of Hematocrit or Hemoglobin
Levels on All Claims for the Administration
of Erythropoiesis Stimulating Agents
(ESAs), Implementation of New Modifiers
for Non-ESRD Indications, and Reporting
of Hematocrit/Hemoglobin Levels on all
Non-ESRD, Non-ESA Claims Requesting
Payment for Anti-Anemia Drugs
04/07/2008
5699
R1410CP 01/11/2008
Annual Type of Service (TOS) Update 01/07/2008
5838
R1401CP 12/21/2007
Medicare Shared Systems Modifications
Necessary to Accept and Crossover to
Medicaid National Drug Codes (NDC) And
Corresponding Quantities Submitted on
Form CMS-1500 Paper Claims
04/07/2008
5835
R1398CP 12/19/2007
Annual Type of Service (TOS) Update
(Replaced by Transmittal 1410)
01/07/2008
5838

Rev # Issue Date
Subject Impl Date CR#
R1393CP 12/14/2007
Revised Guidance for Completing Form
CMS-1500
01/07/2008
5749
R1369CP 11/02/2007
Crossover of Assignment of Benefits
Indicator (CLM08) From Paper Claim Input
04/07/2008
5780
R1366CP 11/02/2007
Update to Place of Service (POS) Code Set:
New Code for Temporary Lodging
04/07/2008
5777
R1325CP 08/29/2007
Testing and Implementation of 2008
Ambulatory Surgical Center (ASC)
Payment System Changes
01/07/2008
5680
R1308CP 07/20/2007
Testing and Implementation of 2008
Ambulatory Surgical Center (ASC)
Payment System Changes – Replaced by
Transmittal 1325 –
Replaced by Transmittal
1325
01/07/2008
5680
R1215CP 03/30/2007
Revisions to Form CMS-1500 Submission
Requirements
04/30/2007
5489
R1191CP 03/02/2007
Type of Service (TOS) Corrections 04/02/2007
5510
R1086CP 10/27/2006
Annual Type of Service (TOS) Update 01/02/2007
5361
R1058CP 09/15/2006
Additional Requirements Necessary to
Implement the Revised Health Insurance
Claim Form CMS-1500 (08/05)
01/02/2007
5060
R1049CP 09/01/2006
Update to the Place of Service (POS) Code
Set to Add a Code for Prison/Correctional
Facility
01/02/2007
4316
R1010CP 07/28/2006
Additional Requirements Necessary to
Implement the Revised Health Insurance
Claim Form CMS-1500 (08/05) Rescinded
and replaced by Transmittal 1058
01/02/2007
5060

Rev # Issue Date
Subject Impl Date CR#
R980CP 06/14/2006
Changes Conforming to CR 3648
Instructions for Therapy Services -
Replaces
Rev. 941
10/02/2006
4014
R941CP 05/05/2006
Changes Conforming to CR 3648
Instructions for Therapy Services
10/02/2006
4014
R899CP 03/31/2006
Revised Heath Insurance Claim Form CMS-
1500
10/02/2006
4293
R870CP 02/24/2006
Type of Service (TOS) Corrections 04/03/2006
4322
R735CP 10/31/2005
Processing All Diagnosis Codes Reported
on Claims Submitted to Carriers
04/03/2006
4097
R727CP 10/28/2005
Annual Type of Service (TOS) 01/03/2006
4145
R549CP 04/29/2005
Update to the Place of Service (POS) Code
Set to Add a Code for Pharmacy
10/03/2005
3819
R511CP 03/28/2005
Type of Service (TOS) Corrections 04/18/2005
3788
R506CP 03/18/2005
Updated Manual Instructions for Item 24G
(Days or Units)
07/01/2005
3753
R476CP 02/18/2005
Type of Service (TOS) Corrections 04/04/2005
3717
R400CP 12/16/2004
Incorrect Reporting of MTUS Indicator
When Drugs are Billed Using an NDC Code
04/04/2005
3435
R359CP 11/04/2004
2005 Annual Type of Service (TOS) 01/03/2005
3519
R349CP 10/29/2004
2005 Annual Type of Service (TOS) 01/03/2005
3519
R335CP 10/29/2004
Correction of Reporting of MTUS Indicator
When Drugs are Billed Using an NDC Code
– Rescinded and replaced by Transmittal
400
04/04/2005
3435
R317CP 10/22/2004
Clarification to Chapter 26 N/A 3431

Rev # Issue Date
Subject Impl Date CR#
R228CP 07/16/2004
Lab and Carrier Processing of Claims for
Reference Lab Services When there is No
Face-to-Face Encounter with the
Beneficiary
08/16/2004
3267
R153CP 04/30/2004
Correction of Type of Service (TOS)
Inconsistencies
10/04/2004
3189
R148CP 04/23/2004
Describing the Identity of the Ordering and
Supervising Physician on Form CMS-1500
Paper Claim
05/24/2004
3138
R145CP 04/23/2004
Deletion of the Data Element Requirements
Matrix for Carriers from Chapter 1 and
Chapter 26
05/24/2004
3164
R121CP 03/19/2004
Manualization of Program Memorandum B-
03-040, CR 2730, Dated May 16, 2003,
Regarding Place of Service (POS) Codes
and Revises the Wording of the Group
Home Code, 14
04/01/2004
3087
R108CP 02/27/2004
Correction of Type of Service (TOS)
Inconsistencies in CR 2929
03/29/2004
3018
R005CP 10/10/2003
Update to 2004 HCPCS/Type of Service
Crosswalk
01/01/2004
2929
R001CP 10/01/2003
Initial Publication of Manual NA NA
Back to top of Chapter
