

Healthcare Provision in Bangladesh
Medical Country of Origin Information Report
June 2023

Manuscript completed in 03/2023
Neither the European Union Agency for Asylum (EUAA) nor any person acting on behalf of the
EUAA is responsible for the use that might be made of the information contained within this
publication.
Luxembourg: Publications Office of the European Union, 2023
PDF ISBN 978-92-9403-287-4 doi: 10.2847/913591 BZ-07-23-194-EN-N
© European Union Agency for Asylum (EUAA), 2023
Cover photo/illustration: Indian people taking medicines, Rawpixel.com, © Adobe Stock
188476312, n.d.
Reproduction is authorised provided the source is acknowledged. For any use or reproduction
of photos or other material that is not under the EUAA copyright, permission must be sought
directly from the copyright holders.

HEALTHCARE PROVISION IN BANGLADESH
3
Acknowledgements
The EUAA acknowledges International SOS as the drafters of this report.
The report has been reviewed by International SOS and EUAA.

EUROPEAN UNION AGENCY FOR ASYLUM
4
Contents
Acknowledgements ........................................................................................................................ 3
Contents .......................................................................................................................................... 4
Disclaimer ........................................................................................................................................ 6
Glossary and abbreviations ........................................................................................................... 7
Introduction .................................................................................................................................... 12
Terms of reference ........................................................................................................ 12
Collecting information ................................................................................................... 12
Currency ........................................................................................................................... 12
Quality control ................................................................................................................. 12
1. General information .......................................................................................................... 15
1.1. Geographic context .................................................................................................................. 15
1.2. Demographic context ............................................................................................................... 16
1.3. Economic context ...................................................................................................................... 16
1.4. Vulnerable groups ...................................................................................................................... 17
1.4.1. Rohingya refugees ................................................................................................ 17
2. Healthcare system ............................................................................................................ 19
2.1. Health system organisation .................................................................................................... 19
2.1.1. Overview ................................................................................................................ 19
2.1.2. Public sector ....................................................................................................... 24
2.1.3. Private sector ...................................................................................................... 28
2.2. Healthcare resources .............................................................................................................. 30
2.3. Pharmaceutical sector ............................................................................................................. 30
2.4. Patient pathways ....................................................................................................................... 33
3. Economic factors .............................................................................................................. 34
3.1. Health services provided by the State / Public authorities ............................................ 34
3.2. Risk-pooling mechanisms ...................................................................................................... 35
3.2.1. Public health insurance, national or state coverage ................................ 35
3.2.2. Community-based health insurance schemes ......................................... 36
3.2.3. Private insurance companies ......................................................................... 37
3.3. Out-of-pocket health expenditure ....................................................................................... 39

HEALTHCARE PROVISION IN BANGLADESH
5
3.3.1. Cost of consultations ........................................................................................ 42
3.3.2. Cost of medication ............................................................................................ 43
4. List of useful links ............................................................................................................. 45
Annex 1: Bibliography .................................................................................................................. 47
Annex 2: Terms of Reference ...................................................................................................... 58

EUROPEAN UNION AGENCY FOR ASYLUM
6
Disclaimer
This report was written according to the EUAA COI Report Methodology (2023). The report is
based on carefully selected sources of information. All sources used are referenced.
The information contained in this report has been researched, evaluated and analysed with
utmost care. However, this document does not claim to be exhaustive. If a particular event,
person or organisation is not mentioned in the report, this does not mean that the event has
not taken place or that the person or organisation does not exist.
Furthermore, this report is not conclusive as to the determination or merit of any particular
application for international protection. Terminology used should not be regarded as
indicative of a particular legal position.
‘Refugee’, ‘risk’ and similar terminology are used as generic terminology and not in the legal
sense as applied in the EU Asylum Acquis, the 1951 Refugee Convention and the 1967
Protocol relating to the Status of Refugees.
Neither the EUAA, nor any person acting on its behalf, may be held responsible for the use
which may be made of the information contained in this report.
The drafting of this report was finalised on 3 May 2023. Any event taking place after this date
is not included in this report.

HEALTHCARE PROVISION IN BANGLADESH
7
Glossary and abbreviations
Term
Definition
8FYP
8
th
Five Year Plan for Bangladesh
ADB
Asian Development Bank
AMC
Antimicrobial Consumption
BDT
Bangladeshi Taka [currency]
BIDA
Bangladesh Investment Development Authority
CBHI
Community-Based Health Insurance
CC
Community Clinic
Chars
Riverine sand and silt landmasses which are home to over
5 million people.
CHCP
Community Health Care Providers
CHE
Current Health Expenditure: estimates of current health
expenditures include healthcare goods and services consumed
during each year. This indicator does not include capital health
expenditures such as buildings, machinery, IT and stocks of
vaccines for emergency or outbreaks.
1
CHT
Chittagong Hill Tracts
CMSD
Central Medical Store Depot
1
World Bank (The), Current health expenditure (% of GDP), 2023, url

EUROPEAN UNION AGENCY FOR ASYLUM
8
Term
Definition
COI
Country of Origin Information
CPP
Certificate for Pharmaceutical Products
DGDA
Directorate General of Drug Administration
DGFP
Directorate General of Family Planning
DGHS
Directorate General of Health Services
DGMEFW
Directorate General of Medical Education and Family Welfare
DGNM
Directorate General of Nursing and Midwifery
EASO
European Asylum Support Office
EPI
Expanded Programme on Immunization
ESP
Essential Health Services Package
EU
European Union
EU+ countries
Member States of the European Union and associated countries
EUAA
European Union Agency for Asylum
FDMN
Forcefully Displaced Myanmar Nationals
FSC
Free Sales Certificate
FWA
Family Welfare Assistant
FWV
Family Welfare Visitor

HEALTHCARE PROVISION IN BANGLADESH
9
Term
Definition
GDP
Gross Domestic Product
GED
General Economics Division
GMP
Good Manufacturing Practices Certificate
HA
Health Assistant
Haor
A wetland habitat in Bangladesh's north-eastern region that is
geographically a shallow depression in the form of a bowl or
saucer, also known as a back swamp, with a combined area of
approximately 2 million hectare (1 ha =2.471 acres) and population
of approximately 19.37 million inhabitants.
HCFC
Health Care Financing Strategy
HIES
Household Income and Expenditure Survey
HPNSDP
Health Population and Nutrition Sector Development Programme
HNPSIP
Health Nutrition Population Sector Strategic Investment Plan
HPNSP
Health, Population and Nutrition Sector Programme
HPSP
Health Population Sector Programme
HSD
Health Services Division
icddr,b
International Centre for Diarrhoeal Disease Research, Bangladesh
IDP
Internally Displaced People
IDRA
Insurance Development and Regulatory Authority

EUROPEAN UNION AGENCY FOR ASYLUM
10
Term
Definition
LGD
Local Government Division
MCWC
Maternal and Child Welfare Centre
MedCOI
Medical Country of Origin Information
MEFWD
Medical Education and Family Welfare Division
Member States
Member States of the European Union
MO
Medical Officer
MOF
Ministry of Finance
MOHFW
Ministry of Health and Family Welfare
MOLGRDC
Ministry of Local Government, Rural Development and
Cooperatives
NCD
Non-Communicable Disease
NCL
National Control Laboratory
NGO
Non-Governmental Organisation
NGO-MFI
NGO Microfinance Institute
NIPORT
National Institute of Population Research & Training
OOPE
Out of Pocket Expense
OPD
Outpatient Department

HEALTHCARE PROVISION IN BANGLADESH
11
Term
Definition
OTC
Over the Counter
PDAB
Permanent Total Disability Insurance
RMG
Ready-Made Garment
RMO
Resident Medical Officer
SACMO
Sub-Assistant Community Medical Officer
SBC
Sadharan Bima Corporation
SSK
Shasthyo Shurokhsha Karmasuchi
SWAp
Sector-Wide Approach
THE
Total Health Expenditure: the sum of public and private health
expenditure. It covers the provision of health services (preventive
and curative), family planning activities, nutrition activities, and
emergency aid designated for health but does not include
provision of water and sanitation.
2
UHFPO
Upazila Health and Family Planning Officers
UHFWCs
Union Level Facilities
Upazila
An administrative unit, which is a subdivision of a district formerly
known as "thana". Bangladesh has 495 Upazilas.
UPFO
Upazila Family Planning Officer
USD
United States Dollar
2
World Bank (The), Health expenditure, total (% of GDP), 2023, url

EUROPEAN UNION AGENCY FOR ASYLUM
12
Introduction
Methodology
The purpose of the report is to provide information on access to healthcare in Bangladesh.
This information is relevant to the application of international protection status determination
(refugee status and subsidiary protection) and migration legislation in EU+ countries.
Terms of reference
The terms of reference for this Medical Country of Origin Information Report can be found in
Annex 2. The drafting period finished on 27 January 2023, peer review occurred between 27
January - 10 February 2023, and additional information was added to the report as a result of
the quality review process during the review implementation up until 10 March 2023. The
report was internally reviewed subsequently.
Collecting information
EUAA contracted International SOS (Intl.SOS) to manage the report delivery including data
collection. Intl.SOS recruited and managed a local consultant to write the report and a public
health expert to edit the report. These were selected from Intl.SOS’ existing pool of
consultants. The consultant was selected based on their experience in leading comparable
projects and their experience of working on public health issues in Bangladesh.
This report is based on publicly available information in electronic and paper-based sources
gathered through desk-based research. This report also contains information from multiple
oral sources with ground-level knowledge of the healthcare situation in Bangladesh who were
interviewed specifically for this report. For security reasons, all oral sources are anonymised.
Currency
The currency in Bangladesh is the Bangladeshi taka (BDT). The currency name, the ISO code
and the conversion amounts are taken from the INFOEURO website of the European
Commission. The rate used is that prevailing at the date of the source, i.e. the publication or
the interview, that is being cited. The prevailing rate is taken from The European Commission
website, InforEuro.
3
Quality control
This report was written by Intl.SOS in line with the European Union Agency for Asylum (EUAA)
COI Report Methodology (2023)
4
, the EUAA Country of Origin Information (COI) Reports
3
European Commission, Exchange rate (InforEuro), n.d., url
4
EUAA, Country of Origin Information (COI) Report Methodology, February 2023, url

HEALTHCARE PROVISION IN BANGLADESH
13
Writing and Referencing Guide (2023)
5
and the EUAA Writing Guide (2022)
6
. Quality control of
the report was carried out both on content and form. Form and content were reviewed by
Intl.SOS and EUAA.
The accuracy of information included in the report was reviewed, to the extent possible,
based on the quality of the sources and citations provided by the consultants. All the
comments from reviewers were reviewed and were implemented to the extent possible, under
time constraints.
Sources
In accordance with EUAA COI methodology, a range of different published sources have been
consulted on relevant topics for this report. These include: governmental publications,
academic publications, reports by non-governmental organisations and international
organisations, as well as Bangladeshi media.
In addition to using publicly available sources, three oral sources were contacted for this
report. The oral sources are all officers in the MOHFW and they are anonymised in this report
for security reasons. The sources were assessed for their background and ground-level
knowledge. All oral sources are described in the Annex 1: Bibliography. Key informant
interviews were carried out in February 2023.
5
EUAA, Country of Origin Information (COI) Reports Writing and Referencing Guide, February 2023, url
6
EUAA, The EUAA Writing Guide, April 2022, url

HEALTHCARE PROVISION IN BANGLADESH
15
1. General information
The Constitution of the People's Republic of Bangladesh establishes the role of the State in
‘planned economic growth’ and ‘improvement in the material and cultural standard of living of
the people’. The government is responsible to its citizens for their basic needs, for example,
‘food, clothing, shelter, education and medical care’ (article 15(a)).
8
Article 18(1) of the
constitution establishes that the State shall have regard to ‘raising the level of nutrition and the
improvement of public health’ (article 18(1)).
9
1.1. Geographic context
Bangladesh covers 147 570 square kilometres,
10
and is densely populated with approximately
1 286 people per square kilometre.
11
It is the world’s seventh most climate risk-affected
country, with 185 extreme events recorded and 0.38 fatalities per 100 000 inhabitants
between 2000 and 2019.
12
According to a 2022 World Bank report, climate-related cyclones,
flooding, drought, change of disease patterns and loss of agricultural lands threaten
communities causing disproportional damage and disrupting lives and livelihoods. Floods
have caused severe economic impacts in Bangladesh, while cyclones are responsible for the
highest number of deaths. Heat stress, river and coastal flooding and landslides are predicted
to increase between 2041 and 2060 with devastating effects even under low-emission
scenarios.
13
In 2022, the World Bank reported on challenges facing Bangladesh: the capital and the
largest city Dhaka faces air pollution, water logging, poor waste disposal and traffic
congestion, while Chattogram and Khulna are exposed to risks related to their coastal
geographic location. Low-income residents are more exposed to these risks and face
inadequate water supply and sanitation, high population density and poor housing quality.
14
The use of solid fuels as primary cooking fuels, mostly wood and crop residues, increases
indoor air pollution and has adverse effects on the health of women and children.
15
A 2019
survey found that only 19 % of the population reported a primary reliance on clean fuels and
technologies for cooking and lighting.
16
8
Bangladesh, Constitution of the People's Republic of Bangladesh, 1972, url
9
Bangladesh, Constitution of the People's Republic of Bangladesh, 1972, url
10
World Bank (The), Surface area (sq. km) - Bangladesh, 2023, url
11
World Bank (The), Population density (people per sq. km of land area) - Bangladesh, 2023, url
12
Eckstein D. et al., Global Climate Risk Index 2021, Germanwatch, January 2021, url, p. 13
13
World Bank (The), Bangladesh Country Climate and Development Report, October 2022, url, p. 12
14
World Bank (The), Bangladesh Country Climate and Development Report, October 2022, url, p. 10
15
World Bank (The), Bangladesh Country Climate and Development Report, October 2022, url, p. 10
16
Bangladesh, BBS, Progotir Pathey, Bangladesh Multiple Indicator Cluster Survey 2019, Key Findings, 2019, url,
p. 11

EUROPEAN UNION AGENCY FOR ASYLUM
16
Bangladesh is vulnerable to environmental change, it is densely populated and will continue
to experience population increases through to 2050, by when it could have 13.3 million
internal climate migrants.
17
1.2. Demographic context
Bangladesh is undergoing social and demographic change, including urbanization and
industrialisation.
18
The population has increased from 50 million in 1960 to 169 million in
2021.
19
The 2017-2018 Demographic and Health Survey reports that 32 % of the population is
below 15 years of age.
20
Life expectancy at birth has increased from 50, in 1972, to 72 in
2020.
21
Migration from rural areas to urban areas is increasing. In 1960, 95 % of the population lived in
rural areas while in 2021 it was 61 %.
22
Bangladesh has a rural network of public sector health
services but lacks an equivalent network in the urban areas.
23
As a result, the poorest part of
the population living in urban areas is deprived of essential health care services.
24
A rapid and
consistent inflow of migrants provides an additional source of pressure on services in urban
slums and large cities.
25
Bangladesh is also undergoing an epidemiological transition, especially in its urban areas.
Shafique et al. cite studies from 2016 to 2019 on non-communicable diseases (NCDs) among
the urban poor in Bangladesh as showing increases in obesity and hypertension, with the
prevalence of hypertension in urban areas being more than double that of rural areas.
Hypertension and diabetes are also prevalent among urban slum dwellers in Dhaka, with
women reporting higher prevalence rates.
26
1.3. Economic context
In 2022, the World Bank reported that Bangladesh has been among the fastest growing
economies in the world, with annual per capita income growth of 4.0 % between 1990 and
2020, during which the country transited from a mainly agricultural economy to an industry
and services dominated economy.
27
Ready-made garment (RMG) exports, remittances from
17
World Bank (The), Groundswell: Preparing for Internal Climate Migration, 2018, url, p. 144
18
Bangladesh, GED, 8th Five Year Plan, July 2020 - June 2025, Promoting Prosperity and Fostering Inclusiveness,
December 2020, url, p. 587
19
World Bank (The), Population Total Bangladesh, 2023, url
20
Bangladesh, NIPORT, Bangladesh Demographic and Health Survey 2017-18, October 2020, url, p. 14
21
World Bank (The) Data, Life expectancy at birth, total (years) – Bangladesh, 2023, url
22
World Bank (The) Data, Rural population (% of total population) – Bangladesh, 2023, url
23
Bangladesh, MOLGRDC, National Urban Health Strategy, November 2014, url, p. 6
24
Bangladesh, MOLGRDC, National Urban Health Strategy, November 2014, url, p. 6
25
Bangladesh, GED, 8th Five Year Plan, July 2020 - June 2025, Promoting Prosperity and Fostering Inclusiveness,
December 2020, url, p. 587
26
Shafique, S. et al., Epidemiological Transition and Non-Communicable Diseases among Urban Poor in
Bangladesh: A Knowledge Synthesis, 2019, url, p. 4
27
World Bank (The), Bangladesh Country Climate and Development Report, October 2022, url, p. 8

HEALTHCARE PROVISION IN BANGLADESH
17
the Bangladeshi diaspora, stable macroeconomic conditions and domestic consumption
contribute to this growth.
28
Income levels are rising: the Household Income and Expenditure Survey (HIES) 2016 found the
national average monthly household income to be BDT 15 945 (EUR 168). Monthly household
incomes were found to differ between urban and rural areas being BDT 22 565 (EUR 237) and
BDT 13 353 (EUR 140) respectively. This is an increase since 2010, of 38.90 % at the national
level and of 36.96 % in urban and 38.40 % in rural areas.
29
The increase in non-communicable
diseases is partially attributed to poor nutrition related to lifestyle changes.
30
1.4. Vulnerable groups
The Ministry of Health and Family Welfare (MOHFW) identified hard to reach populations and
the disadvantaged including:
• specific populations: there are an estimated 2.5 million people who are members of
[minority] ethnic populations. 42 % reside in three hill districts of the Chittagong Hill
Tracts (CHT), while others are dispersed in hilly regions in the north and some coastal
districts. They belong to 45 different communities with low percentages of literacy and
nutritional status. These communities are poorly served by health facilities and it is
difficult to attract health workers to work in these remote areas;
• people with disabilities: many preventable disabilities are due to poverty, and disabled
girls face additional problems such as sexual abuse and marginalisation;
• elderly: elderly women are particularly affected, socially and economically, due to
widowhood and poverty;
• geographically excluded: populations in the chars, the haor areas and the remote
coastal areas where access is difficult, especially during rainy season; and
• professionally marginalized and socially excluded groups: including, but not limited to,
sweepers and sex workers who are also impoverished, who may not be aware of the
health consequences of their professional activities, and who are unable to take
preventive or curative measures or to change occupations.
31
1.4.1. Rohingya refugees
As of October 2022, more than 943 000 stateless Rohingya refugees are settled in Ukhiya
and Teknaf Upazilas, in the Southernmost coastal part of the country. The majority live in 34
28
World Bank (The), The World Bank in Bangladesh, 6 October 2022, url; ADB, Bangladesh, Asian Development
Bank Fact Sheet, July 2022, url, p. 1
29
Bangladesh, BBS, Preliminary Report on Household Income and Expenditure Survey 2016, October 2017, url,
pp. 21-22
30
Bangladesh, GED, 8th Five Year Plan, July 2020 - June 2025, Promoting Prosperity and Fostering Inclusiveness,
December 2020, url, p. 587
31
Bangladesh, MOHFW, Strategic Plan for Health Population and Nutrition Sector Development Program (HPNSDP)
2011-16, 2011, url, p. 25

EUROPEAN UNION AGENCY FOR ASYLUM
18
camps, the largest of which, Kutupalong-Balukhali Expansion Site, is host to more than
635 000 people.
32
The Government of Bangladesh refers to Rohingya refugees as Forcefully Displaced Myanmar
Nationals (FDMN).
33
The camps have been described as ‘crowded and unsafe’ and the
Bangladeshi government as keeping ‘restrictive policies’, for instance not allowing permanent
homes and restricting education and movement.
34
Public hospitals are facing increased
demand.
35
Crime rates have increased in the areas of the camps. Repatriation is regarded as
the goal of the Bangladeshi authorities, who are yet to allow any Rohingya to assimilate into
Bangladeshi society.
36
International Crisis Group states that the Government of Bangladesh is concerned that
planning for Rohingya refugees to remain in Bangladesh over the medium to long term would
relax international pressure on the Myanmar government and delay the creation of conditions
for the refugees’ safe and dignified return. The government is also concerned that further
waves of migration would occur if the conditions for Rohingya refugees were to improve in
Bangladesh and if they were to be allowed to integrate into Bangladeshi society.
37
It is also
noted by another source that the Government of Bangladesh is concerned that relaxing its
stance on repatriation would be ‘politically unpopular domestically’.
38
The government has so
far received USD 690 million in grants from Multi-Lateral Development Banks for longer-term
needs in Cox’s Bazar district and co-finances some activities. These funds are directed to a
range of sectors, including water and sanitation, health, social assistance, infrastructure and
disaster risk reduction.
39
32
UNOCHA, Rohingya Refugee Crisis, n.d., url
33
Rashid, R. et al., A descriptive study of Forcefully Displaced Myanmar Nationals (FDMN) presenting for care at
public health sector hospitals in Bangladesh, 2021, url, p. 1
34
Guardian (The), ‘Like an open prison’: a million Rohingya refugees still in Bangladesh camps five years after crisis,
23 August 2022, url
35
Rashid, R. et al., A descriptive study of Forcefully Displaced Myanmar Nationals (FDMN) presenting for care at
public health sector hospitals in Bangladesh, 2021, url, p. 1
36
Anwar A., Does Anyone Want to Solve the Rohingya Crisis?, The Diplomat, 2 February 2023, url
37
International Crisis Group, A Sustainable Policy for Rohingya Refugees in Bangladesh, 27 December 2019, url,
p. 10
38
Development Initiatives, Supporting Longer Term Development in Crises at the Nexus, Lessons from Bangladesh,
2021, url, p. 32
39
Development Initiatives, Supporting Longer Term Development in Crises at the Nexus, Lessons from Bangladesh,
2021, url, p. 37

HEALTHCARE PROVISION IN BANGLADESH
19
2. Healthcare system
2.1. Health system organisation
2.1.1. Overview
The MOHFW is responsible for developing national policies and for planning and decision-
making. MOHFW is financed through central government and through development budgets
and financing from external partners.
40
The Ministry and its regulatory bodies exert control
over the private sector and NGO facilities through rules and regulations.
41
In 2017, the MOHFW
created two divisions: the Health Services Division (HSD) and the Medical Education and
Family Welfare Division (MEFWD).
42
Each division is headed by a secretary who works under
the direction of the Minister of Health.
43
Figure 1. Organogram of the MOHFW, 2020
44
The HSD is responsible for nursing and midwifery; finance and audit; world health and public
health and drug administration and law.
45
Its mission is to ensure the delivery of affordable
quality healthcare for across Bangladesh.
46
The MEFWD is responsible for family planning and
medical education.
47
There are ten implementing authorities under the MOHFW and the head of each of these
holds the title of Director General.
48
The Directorate Generals of Health Services (DGHS) and
of Medical Education and Family Welfare (DGMEFW) are each implementing authorities under
the MOHFW. DGHS delivers and monitors routine health services directly.
49
DGMEFW
prepares and implements policies relating to medical education and family planning.
50
Each of
40
Bangladesh, MOHFW, Health Nutrition Population Sector Strategic Investment Plan, February 2016, url, p. 47
41
Bangladesh, MOHFW, Health Bulletin 2019, 2020, url, p. 9
42
Bangladesh, MOHFW, Health Bulletin 2019, 2020, url, p. 9
43
Bangladesh, MOHFW, Health Bulletin 2019, 2020, url, p. 10
44
Bangladesh, MOHFW, Health Bulletin 2020, 2022, url, p. 25
45
Bangladesh, MOHFW, Health Bulletin 2020, 2022, url, pp. 26
46
Bangladesh, MOHFW, [Mission of HSD], n.d., url
47
Bangladesh, MOHFW, Health Bulletin 2020, 2022, url, pp. 27
48
Bangladesh, MOHFW, Health Bulletin 2020, 2022, url, pp. 28
49
Bangladesh, DGHS, About us, n.d, url
50
Bangladesh, MOF, [Annual Report, Financial Year 2021-2022], October 2022, url,
p. 66

EUROPEAN UNION AGENCY FOR ASYLUM
20
these Directorate Generals operates along the eight administrative divisions of the country
(see Table 1).
The Health Population Nutrition Sector Development Plan (HPNSDP) is one of the main policy
documents for the MOHFW and brings the different health and nutrition programmes into a
single plan. This unifies programmes that had previously been supported by different donors
and planned and implemented by different government departments. The unified approach is
called the Sector Wide Approach (SWAp) and it aims to avoid duplication, improve efficiency
and reduce resource allocation. SWAp was launched in 1998.
51
Each HPNSDP is supported by
an Implementation Programme
52
and an Operational Plan. The Operational Plan set out details
of programme activities along with detailed budgets across the different programmes.
53
At the
time of writing the fifth HPNSDP is being prepared.
a) Administrative structure
This section presents the administrative structure in Bangladesh and shows how the
healthcare system maps onto this structure. It then introduces the Essential Health Service
Package (ESP) and its four tiers.
Table 1 (below) shows the administrative structure across Bangladesh. Bangladesh has eight
regional Divisions: Dhaka, Chattogram, Rajshahi, Khulna, Sylhet, Barisal, Rangpur and
Mymensingh.
54
These are local government bodies and distinct administrative units which are
administered under the Local Government Division (LGD) through elected representatives.
55
There are then Districts, Upazilas, Unions, Wards and Villages.
56
Local government in urban
areas is provided through the City Corporation and the Pourashava (Municipality). There are
12 City Corporations and 330 Municipalities across Bangladesh.
57
51
Bangladesh, MOHFW, Health Population and Nutrition Sector Development Program 2011-16, Program
Implementation Plan, July 2011, url, p. XV
52
Bangladesh, MOHFW, Health Population and Nutrition Sector Development Program 2011-16, Program
Implementation Plan, July 2011, url, pp. 33-34
53
Bangladesh, MOHFW, 4th Health, Population and Nutrition Sector Program 2017-2022, Operational Plan, April
2017, url
54
Bangladesh, Bangladesh National Portal, [Divisions], 25 April 2023, url
55
Bangladesh, MOLGRDC, National Urban Health Strategy, November 2014, url, p. 5
56
Bangladesh, MOHFW, Health Bulletin 2020, 2022, url, p. 18
57
Bangladesh, BBS, Statistical Yearbook Bangladesh 2021, June 2022, url, p. 45

HEALTHCARE PROVISION IN BANGLADESH
21
Table 1. Administrative units of Bangladesh
58
Administrative unit
Number of units
Division
8
City Corporation
12
Municipality
330
District
64
Upazila
492
Union
4 554
Ward
40 987
Village (approx.)
87 320
Figure 2 presents the healthcare system from ward to national level and shows how it maps
onto the administrative structure. Figure 2 also shows that healthcare facilities span different
administrative levels.
59
58
Bangladesh, BBS, Statistical Yearbook Bangladesh 2021, June 2022, url, p. 45; Bangladesh, Bangladesh National
Portal, [Divisions], 25 April 2023, url; Bangladesh, Bangladesh National Portal, [Upazilla List], 25
April 2023, url; Bangladesh, Bangladesh National Portal, [Union List], 25 April 2023, url; Bangladesh,
MOHFW, Health Bulletin 2020, 2022, url, p. 18
59
Bangladesh, MOHFW, Health Bulletin 2020, 2022, url, p. 18

EUROPEAN UNION AGENCY FOR ASYLUM
22
Figure 2. Managerial hierarchy according to types of facilities from national to the ward
level, from the MOHFW, 2020
60
The National Health Care Standards establish the Quality of Care in health service delivery
including service delivery; laboratory and other diagnostic services and pharmaceutical
services; infection control and waste management; and safe and appropriate environment.
61
An ESP was developed to improve services at the Upazila level and below, and also to
complement urban primary healthcare.
62
The ESP is delivered through four tiers which are
shown in Table 2.
63
60
Bangladesh, MOHFW, Health Bulletin 2020, 2022, url, p. 29
61
Bangladesh, MOHFW, National Health Care Standards, January 2015, url, p. 12
62
Bangladesh, MOHFW, Health Bulletin 2020, 2022, url, p. 250
63
Bangladesh, MOHFW, Health Nutrition Population Sector Strategic Investment Plan (HNPSIP) 2016 - 2021,
February 2016, url, pp. 40-41

HEALTHCARE PROVISION IN BANGLADESH
23
Table 2. The four tiers of the Essential Health Service Package, adapted from MOHFW's
Health Nutrition Population Sector Strategic Investment Plan (HNPSIP)
64
Tier
Description
1
Community Level facilities
Domiciliary Visit
Field staff (both from DGHS and Directorate General
Family Planning (DGFP)) conduct house-to-house visits
in the community to provide services to the clients in
their relevant geographical work areas.
Satellite Clinics and
Out-Reach Services
Satellite clinics (8 in each union per month) and EPI
Out-Reach Services (24 per month in each union) are
providing assigned services by Health and Family
Planning Field Workers.
Community Clinic (CC)
13 500 Community clinics have been established, one
per 6 000 population.
The Community Clinics are managed by Community
Health Care Providers (CHCP), Health Assistant (HA)
and Family Welfare Assistants (FWA).
2
Union Level Facilities (UHFWCs; Sub-Centres; and Maternal and Child Welfare
Centres (MCWCs) at union)
Union Health and Family Welfare Centres are mainly established in each Union.
Medical Doctors with additional, Family Welfare Visitors (FWVs); Sub-Assistant
Community Medical Officers (SACMO) and Pharmacists, mostly staff these Union
Level facilities.
3
Upazila Level Facilities (Health Complex (UHC) and MCWCs at Upazila)
The Upazila Health Complex is the first level referral centre in each upazila.
They include Upazila Health and Family Planning Officers (UHFPO), Resident
Medical Officers (RMO), Medical Officers (MOs), Medical Officer-MCHFP, Upazila
64
Bangladesh, MOHFW, Health Nutrition Population Sector Strategic Investment Plan (HNPSIP) 2016 – 2021,
February 2016, url, pp. 40-41

EUROPEAN UNION AGENCY FOR ASYLUM
24
Tier
Description
Family Planning Officers (UFPO), Specialist Doctors (Consultants); Staff Nurses;
Laboratory Technologists; and a cadre of field staff.
The Upazila Health Complexes provide both outpatient and inpatient facilities.
4
District Level Facilities (District Hospital and MCWCs at District)
District hospitals are specialised health care facilities and provide consultants from
all relevant disciplines.
The district hospitals are the secondary referral centres.
MCWCs in the districts include Maternal, Neonatal, Child and Family Planning
Services. These facilities are staffed with trained Medical Officers and FWVs.
2.1.2. Public sector
This section covers primary care for urban health services and for rural areas. It then turns to
secondary and tertiary care.
a) Urban health services – primary care
Urban health services are carried out through City Corporations and Municipalities
65
(see
Table 1) and are the responsibility of both the MOHFW and the Ministry of Local Government,
Rural Development and Co-operatives (MOLGRDC).
66
The Local Government (City
Corporation) Act
67
and the Local Government (Paurashava Act)
68
mandate that the Local
Government Division (LGD) deliver and maintain a range of services. These services include
education and basic health services (provision of preventive and promotive health as well as
limited curative care and services) and provision and the maintenance of basic services and
infrastructure for environmental sanitation.
69
The 8th Five Year Plan for Bangladesh (8FYP)
notes that primary health care is not adequate for the urban population and that it is
particularly weak for the urban poor.
70
The Bangladeshi news platform Business Standard reported in 2022 that the MOHFW has
long been interested in taking over urban health service centres, but that MOLGRDC is
65
Bangladesh, MOHFW, Health Bulletin 2019, 2020, url, pp. 162-163
66
Govindaraj, R. et al., Health and Nutrition in Urban Bangladesh, Social Determinants and Health Sector
Governance, World Bank, 2018, url, p. 61
67
Bangladesh, Government of the People’s Republic of Bangladesh,,
[Local Government (City Corporation) Act, 2009 (Act No. 60 of 2009)], 2009, url
68
Bangladesh, Government of the People’s Republic of Bangladesh, Local Government (Paurashava) Act, 2009, url
69
Govindaraj, R. et al., Health and Nutrition in Urban Bangladesh, Social Determinants and Health Sector
Governance, World Bank, 2018, url, p. 62
70
Bangladesh, GED, 8th Five Year Plan, July 2020 - June 2025, Promoting Prosperity and Fostering Inclusiveness,
December 2020, url, p. 587

HEALTHCARE PROVISION IN BANGLADESH
25
reluctant to cede control. The Business Standard further noted that MOHFW acknowledges
that it intends to develop its role in urban health care.
71
A draft service outline for the ESP Urban Component is available in the Health Nutrition
Population Sector Strategic Investment Plan (HNPSIP).
72
b) Rural health services – primary care
In 2020, there were 15 954 primary healthcare facilities in Bangladesh being run by the DGHS
(see Table 3). This includes 13 948 functional Community Clinics.
73
These are sited in rural
areas and provide services to between 6 000 and 12 000 people.
74
Each Community Clinic is
staffed by Community Health Care Providers (CHCP), one Health Assistant (HA) and Family
Welfare Assistants (FWA).
75
The Community Clinics do not provide curative services, but they
provide basic levels of care in Reproductive, Maternal, New-born, Child and Adolescent
Health; Maternal Health Care; New-born and Child Health Care; Management of Child
Malnutrition; Communicable Disease Control (CDC); Non-Communicable Disease Control
(NCDC); Common Illness and Injury; Emergency Care; Common Skin, Eye, Ear and Dental
Diseases; and Behaviour Change Communication.
76
The Upazila Health Complexes range in size from 10 to 100 bed facilities (see Table 3).
77
They
provide more specialised care in the categories described above for Community Clinics.
78
Table 3 shows that outpatient services are provided at Upazila health offices, Union Sub-
centres, Union health and family welfare centres, Urban dispensaries, School health clinics
and at the Tejgaon Health Complex in Dhaka.
District hospitals, located in each of the 64 districts of the country, provide both curative,
surgical and public health services including the Expanded Programme on Immunization (EPI).
A draft service outline for the ESP is available in the HNPSIP.
79
71
Business Standard (The), Ministry for aiding private hospitals to cut patient bills, 21 September 2022, url
72
Bangladesh, MOHFW, Health Nutrition Population Sector Strategic Investment Plan, February 2016, url, pp. 52-59
73
Bangladesh, MOHFW, Health Bulletin 2020, 2022, url, p. 247
74
Bangladesh, MOHFW, Health Bulletin 2020, 2022, url, p. 248
75
Bangladesh, MOHFW, Health Nutrition Population Sector Strategic Investment Plan, February 2016, url, pp. 40-41
76
Bangladesh, MOHFW, Health Nutrition Population Sector Strategic Investment Plan, February 2016, url, pp. 52-54
77
Bangladesh, MOHFW, Health Bulletin 2019, 2020, url, p. 159
78
Bangladesh, MOHFW, Health Nutrition Population Sector Strategic Investment Plan, February 2016, url, pp. 52-54
79
Bangladesh, MOHFW, Health Nutrition Population Sector Strategic Investment Plan, February 2016, url, pp. 52-59

EUROPEAN UNION AGENCY FOR ASYLUM
26
Table 3. Primary healthcare facilities run by the DGHS, adapted from MOHFW, Health
Bulletin 2020 (December)
80
Type of facility
Type of
service
Total no. of
facilities
Total no.
beds
Community clinic (functional)
(Tier 1)*
Outpatient
Department
(OPD)
13 948
0
Other primary-level facilities
(Tier 2)*
Upazila health office
OPD
60
0
Union Sub-centre
OPD
1 312
0
Union health and family welfare centre
(UH & FWC)
OPD
87
0
Urban dispensary
OPD
35
0
School health clinic
OPD
23
0
Tejgaon Health Complex, Dhaka
1
0
Subtotal of other primary-level facilities
1 518
Upazila health complex
(Tier 3)*
100-bed
Hospital
3
300
50-bed
Hospital
345
17 250
80
Bangladesh, MOHFW, Health Bulletin 2020, 2022, url, p. 247

HEALTHCARE PROVISION IN BANGLADESH
27
Type of facility
Type of
service
Total no. of
facilities
Total no.
beds
31-bed
Hospital
65
2 015
10-bed
Hospital
11
110
Subtotal of Upazila health complex
424
19 675
District Hospitals**
(Tier 3)*
50-bed
Hospital
2
100
31-bed
Hospital
7
217
30-bed
Hospital
3
90
25-bed
Hospital
1
25
20-bed
Hospital
38
760
10-bed
Hospital
13
130
Subtotal of District Hospitals
64
1 322
Grand total of primary-level facilities (not
including community clinic)
2 006
20 999
EUROPEAN UNION AGENCY FOR ASYLUM
28
Type of facility
Type of
service
Total no. of
facilities
Total no.
beds
Grand total of primary-level facilities in the
country (including community clinic)
15 954
20 999
* Tiers 1-4 are from the ESP and are defined in Table 2 above.
** District Hospitals with 50 beds and less are here counted as providers of primary care and shown as Tier 3.
c) Secondary care
Secondary care requires specialised equipment and laboratory facilities and includes
diagnosis and treatment which has to be undertaken in a hospital: it is therefore provided at
the level of District Hospital and above. The Facility Registry states that secondary care is
provided from District Hospitals, General Hospitals and 100-250 Bed Hospitals.
81
The Facility
Registry reports that there are 61 such hospitals with approved bed space for a total of
12 350.
82
Table 3, above, lists District Hospitals with 10 to 50 beds and notes that, in this
report, these are counted as providers of primary care and shown as Tier 3 in the ESP.
d) Tertiary care
Tertiary level health facilities provide advanced medical investigations and treatment. Tertiary
care is available to patients who have been referred from primary or secondary health facilities
by medical professionals and tertiary care facilities must offer specialised consultative health
care in both in-patient and outpatient departments. The Facility Registry states that tertiary
care is provided from Medical College Hospitals, Specialised Institutes and Maternity Hospitals
and that these are located at different regional levels,
83
and that in tertiary care facilities under
the DGHS, across Bangladesh, there is approved bed space for 23 076 patients.
84
2.1.3. Private sector
The economic policy of Bangladeshi governments since the 1990s has led to an increase in
for-profit, private sector health care facilities.
85
The MOHFW explains the importance of it
having a partnership-based relationship with the private sector.
86
The Bangladesh Investment
Development Authority (BIDA) describes how the private sector plays a major role in
81
Bangladesh, Government of People's Republic of Bangladesh, Facility Registry [tab for Secondary Health Care],
2023, url
82
Bangladesh, Government of People's Republic of Bangladesh, Facility Registry [Report for all District/General
Hospital], 7 March 2023, url
83
Bangladesh, Government of People's Republic of Bangladesh, Facility Registry [tab for Tertiary Health Care],
2023, url
84
Bangladesh, Government of People's Republic of Bangladesh, Facility Registry [Report for 300-500 bed Hospital
(not district hospital), Chest Disease Hospital, Dental College Hospital, Infectious Disease Hospital, Leprosy
Hospital, Medical College Hospital, Medical University, Medical University, Special Purpose Hospital, Specialized
Hospital], 7 March 2023, url
85
Bangladesh, BBS, Report on the Survey of Private Healthcare Institutions 2019, January 2021, url, p. 1
86
Bangladesh, MOHFW, Health Nutrition Population Sector Strategic Investment Plan, February 2016, url, p. 2

HEALTHCARE PROVISION IN BANGLADESH
29
delivering healthcare services and how most tertiary healthcare institutions are run by the
private sector.
87
BIDA characterises private hospitals as being:
• large-scale multi-specialty hospitals with 250 plus beds (such as Evercare, Square,
United, Labaid, Ali Asgar Hospitals), that primarily serve affluent and upper-middle
class segments and account for around 11 % of total beds available in Dhaka;
• foundation/ non-profit hospitals which offer specialised services with discounted
pricing (such as the National Heart Foundation, Kidney Foundation, Ahsania Mission
Cancer and General Hospital); and
• general hospitals/ clinics/ nursing homes as well as private medical college hospitals.
88
A 2019 Bangladesh Bureau of Statistics (BBS) survey of private sector healthcare institutions
concluded that ‘private sector healthcare institutions outnumbered the public sector
healthcare institutions by a large margin’.
89
In 2023, the Facility Registry reported 107 400
hospital beds as being available in 4 164 private hospitals
and clinics.
90
The BBS survey also determined that private sector healthcare provision is not
comprehensive. Gaps were in particular found in the provision of emergency life support,
treatment of HIV and cardiovascular conditions, and the provision of specialised cancer
therapy.
91
Private facilities that provide health care services and all pharmacies must obtain a license to
operate from MOHFW.
92
In 2017 the MOHFW issued an order to all private hospitals, clinics
and diagnostic centres regarding the renewal of licences.
93
The HNPSIP identifies the need to
tighten regulation of private secondary and tertiary care facilities.
94
In 2022, the health
research institute icddr,b reported that approximately 80 % of hospitals in Bangladesh were
private facilities and that many operated with little regulation. icddr,b describes the results of a
survey of private health facilities which it conducted, that found that 6 % of facilities surveyed
had a valid license and that 59 % were in the process of applying for a new, or renewing an
existing, license.
95
The news site bdnews24.com reported that, as of 31 August 2022, the
government had levied fines worth BDT 1.1 million [EUR 11 500] on unregistered private
medical facilities across Bangladesh.
96
87
Bangladesh, BIDA, Healthcare & Medical Device Industries, June 2021, url, p. 2
88
Bangladesh, BIDA, Healthcare & Medical Device Industries, June 2021, url, p. 3
89
Bangladesh, BBS, Report on the Survey of Private Healthcare Institutions 2019, January 2021, url, p. xxxv
90
Bangladesh, Government of People's Republic of Bangladesh, Facility Registry [Report for all Private Hospital /
Clinic], 7 March 2023, url
91
Bangladesh, BBS, Report on the Survey of Private Healthcare Institutions 2019, January 2021, url, pp. xliii-xliv
92
Govindaraj, R. et al., Health and Nutrition in Urban Bangladesh, Social Determinants and Health Sector
Governance, World Bank, 2018, url, p. 65
93
Bangladesh, MOHFW, , [Emergency Notice for Private Hospitals, clinics
and diagnostic centers], 5 September 2017, url
94
Bangladesh, MOHFW, Health Nutrition Population Sector Strategic Investment Plan, February 2016, url, p. 20
95
icddr,b, Licensing is the gateway to improving quality of services at private health facilities: finds an icddr,b
assessment, 30 August 2022, url
96
bdnews24.com, Bangladesh regulator orders private medical facilities to display registration details, 2
September 2022, url

EUROPEAN UNION AGENCY FOR ASYLUM
30
2.2. Healthcare resources
In 2015, the WHO characterised the health system in Bangladesh as having a shortage of
skilled health workers with twice as many doctors as nurses. Skilled health workers are
clustered in urban areas.
97
Community Clinics, the main rural facilities, are typically
understaffed and are insufficiently equipped.
98
The WHO found unqualified/semi-qualified
allopathic practitioners, such as village doctors and Community Health Workers (CHWs), to be
located mainly in rural areas. Traditional healers and trained/traditional birth attendants
practice in rural areas. Drug shop attendants are evenly distributed between urban and rural
areas.
99
An inequitable distribution of the health workforce was first reported in 1998.
100
In 2007,
Bangladesh Health Watch reported an unequal distribution and found key health providers
and qualified professionals being mainly located in urban areas and the metropolitan areas of
Dhaka, Chittagong, Rajshahi and Khulna.
101
An interviewee for this report stated that the
distribution of skilled human resources and the allocation of funding is to this day unequal: in
the divisions of Dhaka, Barisal, Mymensingh and Sylhet between 60 % and 70 % of posts for
qualified health professionals are filled, while the Chattogram, Khulna, Rajshahi and Rangpur
divisions have between 30 % and 40 % of posts filled. In addition, the skilled medical
resources are concentrated in cities rather than being spread across the divisions and
covering remote areas where demand is high.
102
In 2015, the WHO further reported that emergency transport services (ambulance) are
available in public sector facilities, but these are not in a centralized system so individual
facilities need to be contacted to access the service. The authors noted there are some for-
profit private enterprises that provide emergency transport services but that public sector
ambulance services can be poorly equipped, inoperative and can sometimes be used for
other purposes.
103
2.3. Pharmaceutical sector
Drug administration is a directorate within the MOHFW which is led by the Directorate General
of Drug Administration (DGDA).
104
The office of the DGDA is mandated to ensure quality,
97
WHO, Regional Office for the Western Pacific, Bangladesh Health System Review, 2015, url, p. 93
98
WHO, Regional Office for the Western Pacific, Bangladesh Health System Review, 2015, url, p. 92
99
WHO, Regional Office for the Western Pacific, Bangladesh Health System Review, 2015, url, p. 94
100
Ahmed, S.M. et al., The health workforce crisis in Bangladesh: shortage, inappropriate skill-mix and inequitable
distribution, 2011, url, p. 6
101
Bangladesh Health Watch, The State of Health in Bangladesh 2007: health workforce in Bangladesh, who
constitutes the healthcare system?, 2007, url, p. 24
102
Source B, interview, Dhaka, 8 February 2023. Source B is an officer in the DGHS / DGMEFW, MOHFW. The
person wishes to remain anonymous.
103
WHO, Regional Office for the Western Pacific, Bangladesh Health System Review, 2015, url p. 114
104
Bangladesh, MOHFW, Health Bulletin 2019, 2020, url, p. 9

HEALTHCARE PROVISION IN BANGLADESH
31
efficacy and safety of pharmaceutical products through the implementation of relevant
legislation.
105
The main functions of the DGDA are:
• to supervise and implement the drug regulations;
• to regulate activities related to import, procurement of raw and packing materials,
production and import of finished medication, export, sale, pricing, and so on;
• to monitor and regulate the activities of all drug manufacturing companies;
• as Licensing Authority (LA), the DGDA issues licenses to manufacture, store, sell,
import and export drugs and medicines.
106
Pharmaceutical manufacturing in Bangladesh currently uses advanced technology to produce
medicines and, since 2009, Bangladeshi manufacturers have been supplying essential
medicine to all health centres in the country.
107
In 2016, Bangladesh met 97 %
108
of its domestic
demand and in 2020, this rose to 98 %.
109
BIDA reported that the industry contributed
approximately 1.8 % to the GDP.
110
Since 2016 the country has exported medical drugs to 113
countries.
111
BIDA also reported that, in 2020, Bangladesh had 271 Allopathic, 205 Ayurvedic,
271 Unani (Islamic traditional medicine), 32 Herbal and 79 Homeopathic drug producing
companies.
112
Bangladesh has had three iterations of its National Drugs Policy: the first was in 1982;
113
the
second was in 2005;
114
and the third in 2016.
115
The 2016 drug policy formulated specific
guidelines for drug safety, efficacy, logical use of drugs and effective control of drugs.
116
It
contains guidelines for production, marketing, storage and import and export of medicine.
117
A
guideline on Antimicrobial Consumption Surveillance has been issued
118
as well as a centre
and a clinical study for bioequivalence.
119
The 2016 national drug policy has established a
Pharmacovigilance System to monitor adverse drug reactions. This was examined by external
WHO assessors in July 2021 and awarded maturity level 3.
120
105
Bangladesh, MOHFW, DGDA, Quality manual, 18 May 2021, url, p. 13
106
Bangladesh, MOHFW, DGDA, Background, 6 March 2022, url
107
Bangladesh, MOHFW, [Gazette on National Drug Policy 2016], 2017, url, p. 2
108
Bangladesh, MOHFW, [Gazette on National Drug Policy 2016], 2017, url, p. 1
109
Bangladesh, BIDA, Pharmaceuticals & API Industries, December 2020, url, p. 2
110
Bangladesh, BIDA, Pharmaceuticals & API Industries, December 2020, url, p. 2
111
Bangladesh, MOHFW, [Gazette on National Drug Policy 2016], 2017, url, p. 1
112
Bangladesh, BIDA, Pharmaceuticals & API Industries, December 2020, url, p. 2
113
Bangladesh, DDA, Report of the Expert Committee for Drugs on National Drug Policy 1982, 1986, url
114
Bangladesh, MOHFW, National Drug Policy, 5 May 2005, url
115
Bangladesh, MOHFW, [Gazette on National Drug Policy 2016], 2017, url
116
Bangladesh, MOHFW, [Gazette on National Drug Policy 2016], 2017, url, p. 23
117
Bangladesh, MOHFW, [Gazette on National Drug Policy 2016], 2017, url, pp. 2-30
118
Bangladesh, MOHFW, DGDA, (Draft) Guideline on Antimicrobial Consumption Surveillance in Bangladesh, July
2022, url
119
Source A, interview, Dhaka, 8 February, 2023. Source A is an officer in the MOHFW. The person wishes to
remain anonymous.
120
Bangladesh, MOHFW, ADRM, DGDA, Pharmacovigilance Newsletter, March 2022, url, p. 5

EUROPEAN UNION AGENCY FOR ASYLUM
32
The national Essential Drugs List is set out in the 2016 policy, and it includes lists for essential
Allopathic,
121
Ayurvedic
122
and Unani
123
drugs. It covers Homeopathic Medicine
124
and Over-
The-Counter (OTC) medicines selected from commonly used Allopathic, Ayurvedic and Unani
drugs with fewer or smaller side-effects.
125
The Central Medical Store Depot (CMSD) of the
DGHS is responsible for the purchase, storage and distribution of all medical drugs to all
required places.
126
There are 219 medicines on the list, of which 117 have a fixed retail price.
127
Healthcare and pharmaceutical professionals are able to get information on available and
recent drug products from DIMS (Drug Information Management System). DIMS is a
commercial software application which can be used on mobile phones, which provides an
index of clinical drug information applicable across Bangladesh and which is currently free to
use. It provides information on available and recent drug products and is aimed at healthcare
and pharmaceutical professionals. The developers state that it is updated frequently and that
it has information on over 24 000 brand name and 1 400 generic medications.
128
DIMS
provides a database into which pharmaceutical companies can upload information about their
medications.
129
The issue of counterfeit medicines and the adverse effect they have on society has been
raised in the media.
130
An analysis of medicines collected from private drug outlets in Dhaka
city found that the majority of the samples analysed were of good quality; and that over 90 %
of the samples from the Dhaka City Corporation region were acceptable in quality and in
compliance with pharmacopoeial reference ranges.
131
The authors concluded that there is
scope for improving the storage of the ‘distributed medicines and for lowering the prices of
the medicines in the private drug outlets’.
132
The authors also noted that, during their survey,
no provider asked the buyers of the samples for a medical prescription.
133
121
Bangladesh, MOHFW, [Gazette on National Drug Policy 2016], 2017, url, pp. 24-39
122
Bangladesh, MOHFW, [Gazette on National Drug Policy 2016], 2017, url, pp. 40-41
123
Bangladesh, MOHFW, [Gazette on National Drug Policy 2016], 2017, url, pp. 42-49
124
Bangladesh, MOHFW, [Gazette on National Drug Policy 2016], 2017, url, pp. 50-57
125
Bangladesh, MOHFW, [Gazette on National Drug Policy 2016], 2017, url, pp. 58-64
126
Bangladesh, MOHFW, Central Medical Stores Depot (CMSD), url
127
Prothomalo.com, Price of 53 essential medicines set to increase, 16 July 2022, url
128
IT Medicus, Drug Information Management System (DIMS), 2022, url
129
IT Medicus, What is DIMS Gateway, 2022, url
130
New Age Bangladesh, Counterfeit medicines flood markets across Bangladesh, 25 September 2021, url; Daily
Star (The), Countering counterfeit medicine in Bangladesh, 27 February 2022, url
131
Rahman, M.S. et al., A comprehensive analysis of selected medicines collected from private drug outlets of
Dhaka city, Bangladesh in a simple random survey, 2022, url, p. 10
132
Rahman, M.S. et al., A comprehensive analysis of selected medicines collected from private drug outlets of
Dhaka city, Bangladesh in a simple random survey, 2022, url, p. 14
133
Rahman, M.S. et al., A comprehensive analysis of selected medicines collected from private drug outlets of
Dhaka city, Bangladesh in a simple random survey, 2022, url, p. 4

HEALTHCARE PROVISION IN BANGLADESH
33
2.4. Patient pathways
The HNPSIP identifies a functional referral system as one of its ten key messages.
134
This
includes developing partnerships between the public sector and Alternative Medicine Care
providers and hospitals and clinics in the private sector so as to increase accessibility of
services, including in urban and rural areas that are hard to reach.
135
MOHFW recognises the
importance of referral systems that span community level facilities to national-level hospitals
and the need for Health Information Systems to enable this.
136
The Business Standard reported in 2022 that the MOHFW acknowledges that patients do not
use primary healthcare centres, but rather go directly to hospitals. MOHFW intends to expand
its role in urban health care to counteract this issue in urban areas and to reduce pressure on
secondary and tertiary healthcare facilities.
137
A functioning referral system could reportedly
halve the pressure on large tertiary hospitals.
138
This is corroborated by an interviewee for this report who stated that referrals from Upazila
Health Complexes to secondary and tertiary level healthcare do occur but, when people fall ill,
they tend to go straight to the outpatient and emergency departments of secondary and
tertiary health care.
139
In 2018, the World Bank reported that providers and services were fragmented and that there
was no coordination of the health care service delivery system in urban areas, which resulted
in a subsequent failure to provide comprehensive care. The World Bank authors found no sign
of horizontal integration, i.e., of facilities working together to provide a comprehensive range
of services to the population in their districts. They also found that the referral system lacked
vertical integration, with patients accessing specialized care directly without referrals.
140
134
Bangladesh, MOHFW, Health Nutrition Population Sector Strategic Investment Plan (HNPSIP), 2016 – 2021,
February 2016, url, p. 3
135
Bangladesh, MOHFW, Health Nutrition Population Sector Strategic Investment Plan (HNPSIP), 2016 – 2021,
February 2016, url, p. 17
136
Bangladesh, MOHFW, Health Bulletin 2020, 2022, url, pp. 317-318
137
Business Standard (The), Ministry for aiding private hospitals to cut patient bills, 21 September 2022, url
138
Daily Star (The), Patient Referral System: Still elusive after all these years, 23 January 2023, url
139
Source B, interview, Dhaka, 8 February 2023. Source B is an officer in the DGHS / DGMEFW, MOHFW. The
person wishes to remain anonymous.
140
Govindaraj, R. et al., Health and Nutrition in Urban Bangladesh, Social Determinants and Health Sector
Governance, World Bank, 2018, url, p. 70

EUROPEAN UNION AGENCY FOR ASYLUM
34
3. Economic factors
3.1. Health services provided by the State / Public
authorities
Health services provided by the State are set out in section 2.1.2. Public sector. The
Government of Bangladesh has been described as subsidising public health facilities so as to
cover the ‘bare minimum’ of the cost of care.
141
Despite an upward trend in health expenditure
shown in Figure 3 and Figure 4 below, Bangladesh continues to have the lowest per capita
expenditure on health, and the lowest expenditure as a percentage of GDP, of the 11 member
states in the WHO South East Asia Region.
142
Figure 3 shows that per capita health
expenditure by the Government increased from USD 8.62 in 2000 to USD 50.66 in 2020.
143
Figure 3. Current health expenditure per capita (current USD) - Bangladesh
144
141
Rahman, M.M., et al., Forgone healthcare and financial burden due to out-of-pocket payments in Bangladesh: a
multilevel analysis, 2022, url, p. 9
142
WHO, Current health expenditure per capita (current USD) – WHO South East Asia Region, n.d., url; WHO,
Current health expenditure as a percentage of Gross Domestic Product (GDP) – WHO South East Asia Region, n.d.,
url
143
WHO, Current health expenditure per capita (current USD) - Bangladesh, n.d., url
144
WHO, Current health expenditure per capita (current USD) - Bangladesh, n.d., url. Select: Indicators, Aggregates
‘Current Health Expenditure (CHE) per Capita in US$’; Country: Bangladesh; Years 2000 to 2021; Units of
expenditure: current US$ per capita

HEALTHCARE PROVISION IN BANGLADESH
35
Figure 4 shows per capita spending as a percentage of Gross Domestic Product (GDP). This
has risen gradually from 2.11 % in 2000 to 2.63 % in 2020.
Figure 4. Current health expenditure as a percentage of Gross Domestic Product (GDP)
145
3.2. Risk-pooling mechanisms
3.2.1. Public health insurance, national or state coverage
The Health Care Financing Strategy (HCFC) 2012–2032
146
aims to introduce social health
protection schemes for the poor and for formal sector employees and to move towards
provision for the entire population.
147
In principle, all citizens with an identity card have access
to public health facilities without paying a contribution. For outpatient consultation a low user
charge is required, and while medical supplies should be provided for free, it is commonly not
available in the facilities so the patients will need to supply them. OOP payments are still the
main financer for health services, through the purchase of pharmaceuticals and medical
goods.
148
In 2016, the government introduced a demand-side social health protection scheme, Shasthyo
Suroksha Karmasuchi (SSK), for the below-poverty line population in three upazilas.
149
The
145
WHO, Current health expenditure as a percentage of Gross Domestic Product (GDP) - Bangladesh, n.d., url.
Select: Indicators, Aggregates ‘Current Health Expenditure (CHE) as % Gross Domestic Product (GDP)’; Country:
Bangladesh; Years 2000 to 2020; Units of expenditure: current US$ per capita
146
Bangladesh, MOHFW, Expanding Social Protection for Health: Towards Universal Coverage, Health Care
Financing Strategy 2012–2032, September 2012, url
147
Rahman, T. et al., Financial risk protection in health care in Bangladesh in the era of Universal Health Coverage,
June 2022, url, p. 13
148
WHO, Regional Office for the Western Pacific, Bangladesh Health System Review, 2015, url, pp. 66-70
149
Bonilla-Chacin, M.E. et al., Pathways to Reduce Household Out-of-Pocket Expenditure, 2020, url, p. 32

EUROPEAN UNION AGENCY FOR ASYLUM
36
scheme covers inpatient care for 70 different disease groups, with a benefit of USD 620 per
household per year.
150
SSK is in the piloting phase and while the package of benefits that it
offers is expected to evolve the efficacy of the scheme in providing protection is not yet
known.
151
3.2.2. Community-based health insurance schemes
In Bangladesh, community-based health insurance (CBHI) exists mainly as a form of micro-
health insurance initiated by NGO-microfinance institutes (NGO-MFIs), by private insurance
companies and by the state-owned corporations, the general insurer Sadharan Bima
Corporation (SBC) and the life insurer Jiban Bima Corporation (JBC).
152
Sheikh et al. categorize
CBHI based on the types of insurance providers:
‘(i) provider-based model, in which private health facilities commence health insurance and
offer healthcare from their health facilities;
(ii) microfinance-based model, where microfinance organizations manage insurance
programs for their borrowers; and
(iii) non-microfinance-based model, where NGOs launch health insurance for the organized
community or specified geographic areas without any link with microfinance’
153
People who cannot secure traditional health insurance, can obtain access to quality
healthcare via micro health insurance packages which have low premium rates. This can
decrease OOP (out-of-pocket) expenses and provide financial protection from unexpected
health care expenditures.
154
Micro-insurance for health is also designed to address spatial
exclusion from health services and cultural exclusion of women from health services.
155
In an academic study the micro-insurance sector in Bangladesh is described as not being very
effective and the authors state that work needs to be done to encourage the use of micro-
insurance products and to build trust among potential stakeholders.
156
The NGO-MFIs in Bangladesh’s microinsurance consists of national institutions such as BRAC,
Grameen Kalyan and Proshika and smaller regional-level NGOs. The national institutions
account for most of the country’s microinsurance clients while smaller regional-level NGOs
tend to offer a larger variety of microinsurance products and have a more substantial number
of policy-holders from lower revenue groups.
157
150
Ahmed, S. et al., Evaluating the implementation related challenges of Shasthyo Suroksha Karmasuchi (health
protection scheme) of the government of Bangladesh: a study protocol, 2018, url, pp. 1-2
151
Bonilla-Chacin, M.E. et al., Pathways to Reduce Household Out-of-Pocket Expenditure, 2020, url, p. 32
152
Sultana, D. et al., Evolution of Micro Insurance in Bangladesh: Financial Cushion for the Bottom of the Pyramid
Population, 2021, url
153
Sheikh, N. et al., Implementation barriers and remedial strategies for community-based health insurance in
Bangladesh: insights from national stakeholders, 2022, url, p. 2
154
BRAC, The Good Feed, Health: Healthcare made hassle-free: Micro health insurance, 12 September 2022, url
155
Werner, W.J., Micro-Insurance in Bangladesh: Risk Protection for the Poor?, August 2009, url, p. 563
156
Mamun, M., The Effectiveness of Microinsurance in Bangladesh: Can It Sustain? 2017, url, p. 14
157
Sultana, D. et al., Evolution of Micro Insurance in Bangladesh: Financial Cushion for the Bottom of the Pyramid
Population, 30 May 2021, url

HEALTHCARE PROVISION IN BANGLADESH
37
BRAC advertises two types of insurance: one with an annual premium of BDT 1 220 [EUR 13]
and one of BDT 650 [EUR 7]. Under the lower premium, BRAC states that the insured is
covered for life insurance of BDT 10 000 [EUR 105] and benefits from the following services:
• outpatient treatment of up to BDT 1 500 [EUR 16];
• hospital facility stay of up to BDT 10 000 [EUR 105];
• normal childbirth of up to BDT 2 200 [EUR 23] and
• caesarean delivery of up to BDT 6 500 [EUR 68].
158
BRAC states that a normal childbirth costs BDT 2 500 [EUR 26] at a BRAC maternity centre. In
addition, there is an admission fee of BDT 100 [EUR 1] as well as check-ups performed by a
midwife or a medical officer costing BDT 100 [EUR 1] and BDT 200 [EUR 2] respectively.
159
Micro-health insurance plans are provided by NGO-MFIs to guarantee loan repayment, as
health issues account for around one-third of all microcredit defaults.
160
Sultana et al. write that
micro-health insurance was originally a way of safeguarding a loan and the model is now used
to improve access to healthcare, especially for lower socioeconomic groups.
161
3.2.3. Private insurance companies
At the end of 2019, 32 life insurers and 45 non-life licensed insurers were in operation.
162
Insurance penetration is low with 13 million people (approximately 8 % of the population) in
Bangladesh having an insurance policy of any kind.
163
The Insurance Development and
Regulatory Authority (IDRA) states that the insurance market does not offer a diverse range of
products and notes that neither universal health insurance nor catastrophic insurance are
available. IDRA attributes this low demand to the poor reputation of the sector and to it being
complicated to there being no established practice amongst Bangladeshi households to
renew insurance policies.
164
Despite this, IDRA expresses optimism about health insurance as
a sector because middle-income groups are increasingly using, and various corporates are
offering, health insurance.
165
Since its inception, in 2010, to 2019, IDRA has approved different types of life insurance, for
example, various types of microinsurance, deposit insurance, Pension Insurance, Accidental
Life Insurance as a Rider (ADAB), Permanent Total Disability Insurance (PDAB) and Health
Insurance, Children Protection Insurance, Hajj Bima,
166
Denmohor Bima,
167
Education Expense
158
BRAC, The Good Feed, Health: Healthcare made hassle-free: Micro health insurance, 12 September 2022, url
159
BRAC, The Good Feed, Health: Healthcare made hassle-free: Micro health insurance, 12 September 2022, url
160
Khan, M.R., et al., Assessing Microinsurance as a Tool to Address Loss and Damage in the National Context of
Bangladesh, June 2013, url, pp. 10-11
161
Sultana, D. et al., Evolution of Micro Insurance in Bangladesh: Financial Cushion for the Bottom of the Pyramid
Population, 2021, url
162
Bangladesh, IDRA, Annual Report, 2018-2019 and 2019-2020, n.d., url, p. 14
163
Bangladesh, IDRA, Annual Report, 2018-2019 and 2019-2020, n.d., url, p. 8
164
Bangladesh, IDRA, Annual Report, 2018-2019 and 2019-2020, n.d., url, pp. 8, 29
165
Bangladesh, IDRA, Annual Report, 2018-2019 and 2019-2020, n.d., url, p. 28
166
Protection and savings policy to enable participation in the hajj, the pilgrimage to Mecca.
167
Policy to enable payment of Denmohor, a fee payable by husband to wife as part of the marriage contract.

EUROPEAN UNION AGENCY FOR ASYLUM
38
Insurance Plan, Mortgage Assurance Plan, Family Protection Plan and SME Loan Protection
Plan.
168
Table 5 shows that when looking at the premiums taken by Life Insurance products, the
percentage of the premiums that were taken by Group & Health Insurance increased from
4.57 % in 2015 to 7.26 % in 2019. Individual insurance is the largest sub-sector and has the
largest growth in percentage points.
169
Table 4. Percentage of gross premium in Life Insurance (2015 to 2019)
170
Year
Individual
Micro-
insurance
Group & Health
Islami
2015
65.64 %
17.64 %
4.57 %
12.15 %
2016
66.95 %
15.55 %
4.79 %
12.70 %
2017
77.8 %
14.66 %
6.00 %
11.53 %
2018
66.37 %
15.45 %
6.55 %
11.62 %
2019
66.13 %
15.43 %
7.26 %
11.18 %
Private insurance companies currently offer a variety of microinsurance products and many of
these schemes have similar terms and conditions. Examples include Gono-Grameen Bima
(general rural insurance), Grameen Jibon Bima (rural life insurance) and Daridra Bimochone
Jibon Bima (rural health insurance) (life insurance for poverty alleviation).
171
These seek to
combine microfinance credit for the poor with health insurance. These private companies are
including the disadvantaged population.
172
168
Bangladesh, IDRA, Annual Report, 2018-2019 and 2019-2020, n.d., url, p. 15
169
Bangladesh, IDRA, Annual Report, 2018-2019 and 2019-2020, n.d., url, p. 28
170
Bangladesh, IDRA, Annual Report, 2018-2019 and 2019-2020, n.d., url, p. 27
171
Sultana, D. et al., Evolution of Micro Insurance in Bangladesh: Financial Cushion for the Bottom of the Pyramid
Population, 2021, url
172
Sultana, D. et al., Evolution of Micro Insurance in Bangladesh: Financial Cushion for the Bottom of the Pyramid
Population, 2021, url

HEALTHCARE PROVISION IN BANGLADESH
39
3.3. Out-of-pocket health expenditure
A study done between 1 December 2015 to 31 December 2016, found health expenditure to
be one of the main reasons for poverty and deprivation amongst low-income households with
approximately 4.7 million people in Bangladesh going into poverty due to health care costs.
173
Out-of-pocket (OOP) health expenditure is unpredictable and has negative consequences
which leave households exposed to the effects of catastrophic health costs. These are
defined as costs that ‘severely disrupt household living standards’ by absorbing between 10 %
and 40 % of household resources.
174
BIDA states that Bangladesh has one of the highest OOP expenditure rates in the world (as a
percentage of Total Health Expenditure (THE).
175
In 2012, MOHFW stated that the reliance on
OOP payments is inequitable and inefficient with a severe impact on the poor. MOHFW set an
objective to halve OOP payments for health, at the point of service and to lower them from the
2012 level of 64 % of THE to a target of 32 % by 2032.
176
The target is not being met as BIDA
reported OOP payments have increased and were close to 74 % of THE in 2020.
177
173
Rabbani, A., Sarker, M., Understanding the effects of an employer-provided health security program on the well-
being, productivity, and health seeking behavior of workers in a semi-formal manufacturing setting in Bangladesh,
2017, url
174
Werner, W.J., Micro-insurance in Bangladesh: Risk Protection for the Poor?, 2009, url, p. 564
175
Bangladesh, BIDA, Healthcare & Medical Device Industries, June 2021, url, p. 6
176
Bangladesh, MOHFW, Expanding Social Protection for Health: Towards Universal Coverage, Health Care
Financing Strategy 2012 -2032, September 2012, url, p. 21
177
Bangladesh, BIDA, Healthcare & Medical Device Industries, June 2021, url, p. 6

EUROPEAN UNION AGENCY FOR ASYLUM
40
Figure 5. Household Out-of-Pocket Payment as a percentage of Current Health
Expenditure
178
Figure 5 uses Current Health Expenditure (CHE) to show that OOPs have increased since
2000 and that they have been above 70 % of CHE since 2014.
179
Figure 6 shows a steady increase in the money paid by each household rising to a high of
USD 37.49 [EUR 34] in 2020.
180
178
WHO, Household out-of-pocket payment as a % of Current health expenditure (CHE) - Bangladesh, n.d., url.
Select: Health Expenditure Data, Financing Schemes, Current health expenditure by financing schemes,
‘Household out-of-pocket payment as a % of Current health expenditure (CHE)’; Country: Bangladesh; Years 2000
to 2020; Units of expenditure: % of Current health expenditure (CHE)
179
WHO, Household out-of-pocket payment as a % of Current health expenditure (CHE) - Bangladesh, n.d., url
180
WHO, Household out-of-pocket payment in current US$ per Capita - Bangladesh, n.d., url
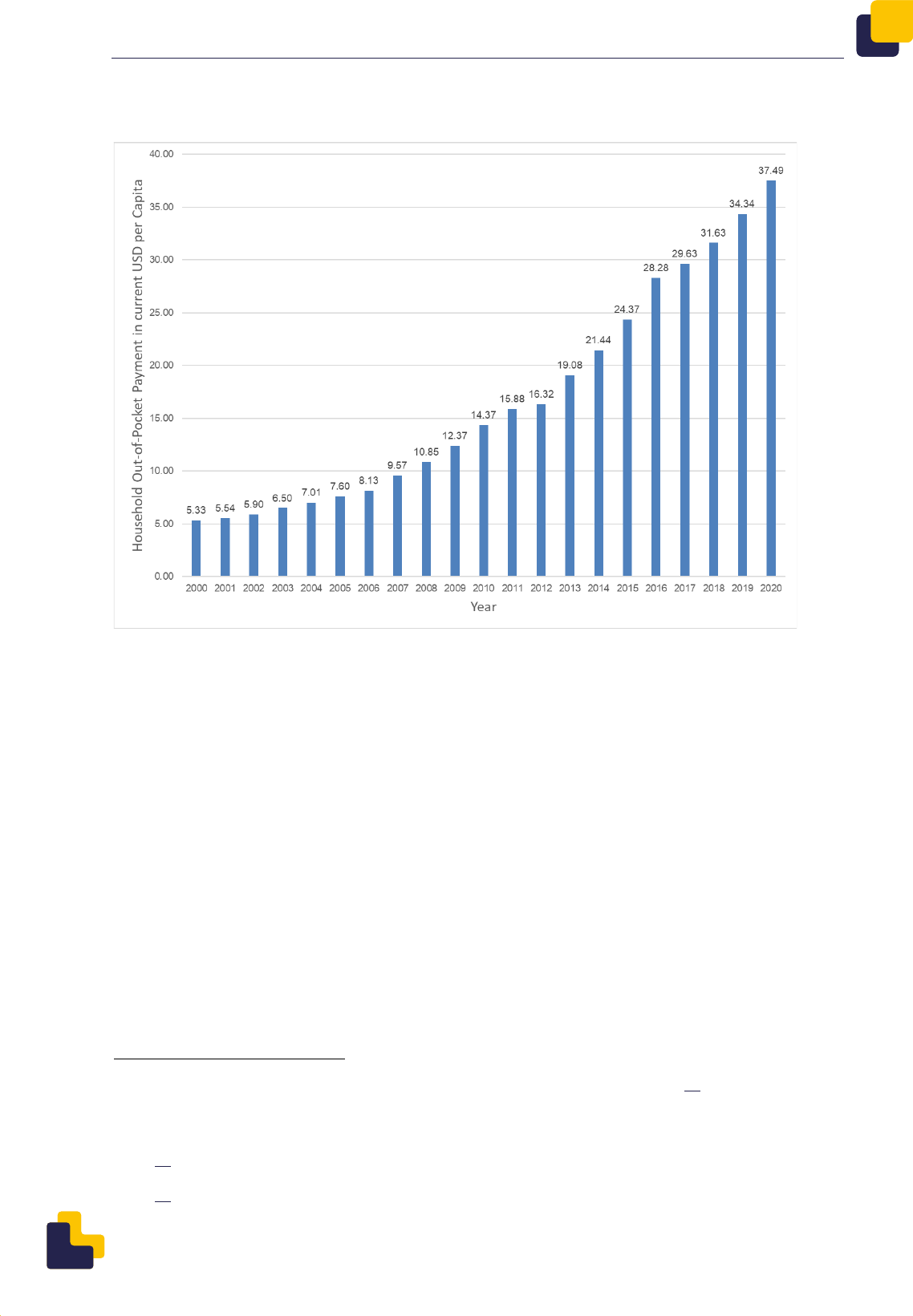
HEALTHCARE PROVISION IN BANGLADESH
41
Figure 6. Household Out-of-Pocket Payment in current USD per Capita
181
A survey of 3 100 households in Dhaka Urban area found that the average OOP spend was
7.7 % of monthly household income (see Table 5 below).
182
Table 6 shows how this study
calculates the percentage of OOP against an average monthly household income for each of
five income quintiles, rather than a national average, and finds great variation in the
percentages paid, from 5.2 % for the richest quintile to 13.3 % and then 32.7 % for the two
poorest quintiles.
183
181
WHO, ‘Household Out-of-Pocket Payment in current US$ per Capita - Bangladesh’, n.d., url. Select: Health
Expenditure Data, Financing Schemes, Current health expenditure by financing schemes, ‘Household out-of-pocket
payment’; Country: Bangladesh; Years 2000 to 2020; Units of expenditure: current US$ per capita
182
Sarker, A.R. et al., Out-of-pocket payment for healthcare among urban citizens in Dhaka, Bangladesh, 24 January
2022, url, p. 11
183
Sarker, A.R. et al., Out-of-pocket payment for healthcare among urban citizens in Dhaka, Bangladesh, 24 January
2022, url, p. 11

EUROPEAN UNION AGENCY FOR ASYLUM
42
Table 5. Cost burden across socioeconomic groups from a household survey in Dhaka
Urban area
184
Income quintile
Average monthly
income (BDT)
Average OOP
Expenditure (BDT)
OOP as a
percentage of
monthly household
income
Poorest
9 852
3 226
32.7 %
Poorer
19 655
2 610
13.3 %
Middle
29 215
2 426
8.3 %
Richer
47 256
3 490
7.4 %
Richest
143 901
7 417
5.2 %
Overall
49 362
3 794
7.7 %
The Business Standard reported that those in lower socioeconomic groups are not able to
afford health services and cite maternal and reproductive health, children’s health services
and non-communicable diseases as services that are out of reach. The price of care at private
treatment facilities in urban areas means it is not accessible to some middle-income groups.
185
3.3.1. Cost of consultations
In an interview conducted for this report, Source C stated that in private practice, the price of
consultation varies between BDT 300 and BDT 2 000 [EUR 3 and EUR 17] depending on the
level of specialty. Private hospitals set the prices for follow-up by specialists and their
assistants. The higher prices charged by the private hospitals are explained as being due to
the price of land, cost of building and maintaining the facilities and staff costs.
186
Institutional care is expensive as, in addition to care, patients and their families must pay for
travel and food as well as hidden expenditures such as ‘unofficial medical charges and
184
Sarker, A.R. et al., Out-of-pocket payment for healthcare among urban citizens in Dhaka, Bangladesh, 24 January
2022, url, p. 11
185
Business Standard (The), Ministry for aiding private hospitals to cut patient bills, 21 September 2022, url
186
Source C, interview, Dhaka, 8 February 2023. Source C is an officer in the MOHFW. The person wishes to
remain anonymous.

HEALTHCARE PROVISION IN BANGLADESH
43
financial incentives or tips to the porters and female helpers (ayas)’.
187
A 2016 study in Sylhet
looked beyond the price of treatment to report on both the direct, and the indirect, costs of
outpatient treatment in order to establish the total cost of illness incurred by a patient and
their household. This study provides an illustration of the full cost of treatment that is borne by
an individual and their household, rather than the price charged by a healthcare facility.
188
The authors divide direct costs of treatment into medical and non-medical costs. Medical costs
include ‘diagnosis, registration fees, medications, diagnostics, continuing care, hospitalization,
rehabilitation; and non-medical costs are the costs of transport to the hospital and any informal
payments’. The authors explain that informal payments include any transfer of money, from
patients to staff, in the expectation of preferential treatment.
189
Indirect costs of illness arise
from loss of income and productivity and can be lost time at work or lost time by a caregiver.
190
The study found that outpatients in public hospitals experience higher total costs than those
treated in private hospitals.
191
The majority of public hospital patients (71 %) were from rural
areas and so had higher travel costs and spent longer travelling than the, mainly urban,
patients of private hospitals. The outpatient experience in public hospitals was characterised
by insufficient numbers of doctors and long queues for treatment. This prompted patients in
public hospitals to make offers of informal payment in order to hasten their access to the
doctors.
192
The cost for treatment in public hospitals is comprised of approximately 97 % of indirect costs
and 3 % of direct costs.
193
While the direct costs in private hospitals are higher than in public
hospitals, the indirect costs incurred in getting care from public hospitals are twice that of
private hospitals. As a result, this 2016 study found that the average total cost of outpatient
treatment in public hospitals was greater (BDT 9 923 or EUR 114) than that in private hospitals
(BDT 5 607 or EUR 64).
194
3.3.2. Cost of medication
Kasonde et al. examined the availability, price and affordability of 61 medicines across six
regions in Bangladesh. They found the private sector (retail pharmacies and clinics) had
greater access to the surveyed medicines than the public sector. The study also showed that,
when compared with international prices, the prices for most medicines in the private sector
were not excessive although some were found to be expensive in all sectors. NCD medicines
were the least affordable medicines by unit price and length of treatment.
195
NCD medicines
and essential medicines were also harder to get than infectious disease medicines and non-
187
Rahman, M.M., et al., Forgone healthcare and financial burden due to out-of-pocket payments in Bangladesh: a
multilevel analysis, 2022, url, p. 9
188
Pavel, M.S., Cost of illness for outpatients attending public and private hospitals in Bangladesh, 2016, url, p. 1
189
Pavel, M.S., Cost of illness for outpatients attending public and private hospitals in Bangladesh, 2016, url, p. 4
190
Pavel, M.S., Cost of illness for outpatients attending public and private hospitals in Bangladesh, 2016, url, p. 4
191
Pavel, M.S., Cost of illness for outpatients attending public and private hospitals in Bangladesh, 2016, url, p. 8
192
Pavel, M.S., Cost of illness for outpatients attending public and private hospitals in Bangladesh, 2016, url, p. 7
193
Pavel, M.S., Cost of illness for outpatients attending public and private hospitals in Bangladesh, 2016, url, p. 9
194
Pavel, M.S., Cost of illness for outpatients attending public and private hospitals in Bangladesh, 2016, url, p. 6
195
Kasonde, L. et al., Evaluating medicine prices, availability and affordability in Bangladesh using World Health
Organisation and Health Action International methodology, 2019, url, p. 8

EUROPEAN UNION AGENCY FOR ASYLUM
44
essential medicines, respectively.
196
They also stated that, while the availability of medicines is
low in public sector facilities, approximately 50 % of public hospital physicians describe
themselves as satisfied with the availability of medicines in facilities from District to Union Sub-
Centre level.
197
In July 2022, the price review committee of the DGDA increased prices of essential drugs.
The newspaper New Age described in an opinion piece this as adding to economic hardship
in an economy that has been affected by Covid.
198
The prices of 19 generic drugs of 53 brands
were increased by the DGDA and drug manufacturers also increased the prices of other
drugs.
199
Media sources report increases in the prices of commonly used drugs such as
amoxicillin, metronidazole, paracetamol,
200
aspirin, diazepam, penicillin, phenobarbital,
phenoxy methyl,
201
benzathine benzylpenicillin, chlorphenamine, ferrous, folic acid,
furosemide, lidocaine, methyldopa, norgestrel, prochlorperazine, and xylometazoline.
202
The price of a single 500 mg paracetamol tablet was increased from BDT 0.7 to BDT 1.2; a
200 mg metronidazole tablet from BDT 0.60 to BDT 1.0; and a 15 ml bottle of amoxicillin BP
from BDT 26.34 to BDT 35.
203
The increases in price vary but they range from rises of 50 % to
100 %.
204
CAB are reported as stating that prices, in retail pharmacists, rose between 13 % and
75 % between May and November 2022.
205
New Age reported that the government has ‘little control over the drug market’.
206
The
newspaper further informed that the DGDA states that drug prices were last reviewed in 2015
and that the market prices of raw materials have increased. In this review, the government
was reportedly under pressure from producers and that consumer’s interests had been of
secondary concern.
207
196
Kasonde, L. et al., Evaluating medicine prices, availability and affordability in Bangladesh using World Health
Organisation and Health Action International methodology, 2019, url, p. 1
197
Kasonde, L. et al., Evaluating medicine prices, availability and affordability in Bangladesh using World Health
Organisation and Health Action International methodology, 2019, url, pp. 1-2
198
New Age Bangladesh, Increase in drug prices adds to people’s economic burden, Opinion, 19 July 2022, url
199
New Age Bangladesh, Increase in drug prices adds to people’s economic burden, Opinion, 19 July 2022, url
200
New Age Bangladesh, Increase in drug prices adds to people’s economic burden, Opinion, 19 July 2022, url;
Business Standard (The), Prices of 53 drugs hiked, 17 July 2022, url; Financial Express (The), Cut prices of
emergency drugs to ease burden on commoners, 24 November 2022, url
201
Business Standard (The), Prices of 53 drugs hiked, 17 July 2022, url; Financial Express (The), Cut prices of
emergency drugs to ease burden on commoners, 24 November 2022, url
202
Business Standard (The), Prices of 53 drugs hiked, 17 July 2022, url
203
New Age Bangladesh, Increase in drug prices adds to people’s economic burden, Opinion, 19 July 2022, url
204
Business Standard (The), Prices of 53 drugs hiked, 17 July 2022, url
205
Financial Express (The), Cut prices of emergency drugs to ease burden on commoners, 24 November 2022, url
206
New Age Bangladesh, Increase in drug prices adds to people’s economic burden, Opinion, 19 July 2022, url
207
New Age Bangladesh, Increase in drug prices adds to people’s economic burden, Opinion, 19 July 2022, url

HEALTHCARE PROVISION IN BANGLADESH
45
4. List of useful links
Organisation
Web address
Bangladesh National Nutrition
Council
http://bnnc.portal.gov.bd/
Diagnostic Centres and
Hospitals
https://www.populardiagnostic.com
Directorate General of Health
Services
https://dghs.gov.bd
Facility Registry
http://facilityregistry.dghs.gov.bd/index.php
Health Economic Unit
https://heu.gov.bd/
Health Services Division
https://hsd.gov.bd/
Hospital Services Management
http://hospitaldghs.gov.bd/introduction/
Ministry of Health and Family
Welfare
http://www.mohfw.gov.bd/
Ministry of Health Education and
Family Welfare division
https://mefwd.gov.bd
Private Hospitals
Ahsania Mission Cancer Hospital
http://www.ahsaniacancer.org.bd/mirpur_center.php
Ali Asgar Hospitals
https://www.asgaralihospital.com
Anwar Khan Modern Hospitals
https://akmmc.edu.bd

EUROPEAN UNION AGENCY FOR ASYLUM
46
Organisation
Web address
Birdem General Hospital
https://www.birdembd.org
Evercare
https://www.evercarebd.com
Green Life Medical College
https://greenlife.edu.bd
LabAID Hospitals
https://labaidgroup.com/specialized/
National Heart Foundation
Bangladesh
https://www.nhf.org.bd
Square Hospitals
https://www.squarehospital.com
United Hospitals
https://www.uhlbd.com/bn

HEALTHCARE PROVISION IN BANGLADESH
47
Annex 1: Bibliography
Oral sources
Source A, interview, Dhaka, 8 February 2023. Source A is an officer in the MOHFW. The
person wishes to remain anonymous.
Source B, interview, Dhaka, 8 February 2023. Source B is an officer in the DGHS / DGMEFW,
MOHFW. The person wishes to remain anonymous.
Source C, interview, Dhaka, 8 February 2023. Source C is an officer in the MOHFW. The
person wishes to remain anonymous.
Public sources
ADB (Asian Development Bank (The)), Bangladesh, Asian Development Bank Fact Sheet, July
2022, https://www.adb.org/sites/default/files/publication/27753/ban-2021.pdf, accessed
7 March 2023
ADB (Asian Development Bank (The)), Social Protection Project Briefs, Developing
Microinsurance Sector in Bangladesh, n.d.,
https://www.adb.org/sites/default/files/publication/28949/developing-microinsurance-ban.pdf,
accessed 5 January 2023
Ahmed, S., Hasan, Z., Ahmed, M.W., Dorin, F., Sultana, M., Islam, Z., Mirelman, A.J., Rehnberg,
C., Khan, J.A.M., Chowdhury, M.E., Evaluating the implementation related challenges of
Shasthyo Suroksha Karmasuchi (health protection scheme) of the government of Bangladesh:
a study protocol, in: BMC Health Services Research, Vol. 18, Issue 1, July 2018,
http://dx.doi.org/10.1186/s12913-018-3337-x, accessed 7 February 2023
Ahmed, S.M., Hossain, M.A., Rajachowdhury, A.M., Bhuiya, A.U., The health workforce crisis in
Bangladesh: shortage, inappropriate skill-mix and inequitable distribution, in: Human
resources for health, Vol 9, Issue 1: 3, 2011, http://dx.doi.org/10.1186/1478-4491-9-3, accessed
10 January 2023
Anwar, A., Does Anyone Want to Solve the Rohingya Crisis? The Diplomat, 2 February 2023,
https://thediplomat.com/2023/02/does-anyone-want-to-solve-the-rohingya-crisis/, accessed 3
March 2023
Bangladesh Health Watch, The State of Health in Bangladesh 2007: health workforce in
Bangladesh, who constitutes the healthcare system?, James P. Grant School of Public Health,
BRAC University, May 2008, http://hdl.handle.net/10361/592, accessed 10 January 2023

EUROPEAN UNION AGENCY FOR ASYLUM
48
Bangladesh, Bangladesh National Portal, [Union List], 25 April 2023,
http://www.bangladesh.gov.bd/site/view/union-list/Union-List, accessed 3 May 2023
Bangladesh, Bangladesh National Portal, [Upazilla List], 25 April 2023,
http://www.bangladesh.gov.bd/site/view/upazila-list/Upazilla-List, accessed 3 May 2023
Bangladesh, Bangladesh National Portal, [Divisions], 25 April 2023,
http://www.bangladesh.gov.bd/site/view/division-list/List-of-Divisions, accessed 3 May 2023
Bangladesh, BBS (Bangladesh Bureau of Statistics), Preliminary Report on Household Income
and Expenditure Survey 2016, 2017, available at: https://catalog.ihsn.org/catalog/7399/related-
materials, accessed 10 January 2023
Bangladesh, BBS (Bangladesh Bureau of Statistics), Progotir Pathey, Bangladesh Multiple
Indicator Cluster Survey 2019, Key Findings, 2019,
http://bbs.portal.gov.bd/sites/default/files/files/bbs.portal.gov.bd/page/b343a8b4_956b_45ca
_872f_4cf9b2f1a6e0/37817b8e25d0d6c1f442e294921ff85e.pdf, accessed 2 February 2023
Bangladesh, BBS (Bangladesh Bureau of Statistics), Report on the Survey of Private
Healthcare Institutions 2019, Ministry of Planning, Dhaka, Bangladesh, January 2021,
http://bbs.portal.gov.bd/sites/default/files/files/bbs.portal.gov.bd/page/b343a8b4_956b_45ca
_872f_4cf9b2f1a6e0/2021-06-30-04-58-22ea330d54a12a1b26bb608d43130b91.pdf,
accessed 7 March 2023
Bangladesh, BBS (Bangladesh Bureau of Statistics), Statistical Yearbook Bangladesh 2021,
June 2022,
http://203.112.218.65:8008/WebTestApplication/userfiles/Image/latesreport/SYB_2021.pdf,
accessed 3 May 2023
Bangladesh, BIDA (Bangladesh Investment Development Authority), Healthcare & Medical
Device Industries, 2021,
https://bida.gov.bd/storage/app/uploads/public/616/6c3/2de/6166c32dec22c700971227.pdf,
20 January 2023
Bangladesh, BIDA (Bangladesh Investment Development Authority), Pharmaceuticals & API
Industries, December 2020,
https://bida.gov.bd/storage/app/uploads/public/616/6c2/000/6166c2000004a202755426.pdf,
accessed 20 January 2023
Bangladesh, Constitution of the People’s Republic of Bangladesh, 1972,
http://bdlaws.minlaw.gov.bd/act-367.html, accessed 01 February 2023
Bangladesh, DDA (Directorate of Drug Administration), Report of the Expert Committee for
Drugs on National Drug Policy of Bangladesh 1982, 1986,
https://dgda.portal.gov.bd/sites/default/files/files/dgda.portal.gov.bd/law/d7161df8_ee32_4d19
_bf16_a663382ae7b5/drug-policy-1982.pdf, accessed 07 February 2023

HEALTHCARE PROVISION IN BANGLADESH
49
Bangladesh, DGHS (Directorate Generals of Health Services), About us, n.d,
https://old.dghs.gov.bd/index.php/en/component/content/article/109-english-root/about-
us/436-who-are-we, accessed 3 March 2023
Bangladesh, GED (General Economics Division), 8th Five Year Plan, July 2020 - June 2025,
Promoting Prosperity and Fostering Inclusiveness, December 2020,
http://plancomm.gov.bd/sites/default/files/files/plancomm.portal.gov.bd/files/68e32f08_13b8_
4192_ab9b_abd5a0a62a33/2021-02-03-17-04-ec95e78e452a813808a483b3b22e14a1.pdf,
accessed 2 February 2022
Bangladesh, Government of People's Republic of Bangladesh, Facility Registry [Report for all
District/General Hospital], 2023,
http://facilityregistry.dghs.gov.bd/report_org_list.php?admin_division=0&admin_district=0&ad
min_upazila=0&org_agency=0&org_type%5B%5D=28&form_submit=1, accessed
7 March 2023
Bangladesh, Government of People's Republic of Bangladesh, Facility Registry [Report for all
Private Hospital / Clinic], 2023,
http://facilityregistry.dghs.gov.bd/report_org_list.php?admin_division=0&admin_district=0&ad
min_upazila=0&org_agency=0&org_type%5B%5D=43&form_submit=1, accessed
7 March 2023
Bangladesh, Government of People's Republic of Bangladesh, Facility Registry [Report for
300-500 bed Hospital (not district hospital), Chest Disease Hospital, Dental College Hospital,
Infectious Disease Hospital, Leprosy Hospital, Medical College Hospital, Medical University,
Medical University, Special Purpose Hospital, Specialized Hospital], 7 March 2023,
http://facilityregistry.dghs.gov.bd/report_org_list.php?admin_division=0&admin_district=0&ad
min_upazila=0&org_agency=0&org_type%5B%5D=75&org_type%5B%5D=34&org_type%5B%
5D=7&org_type%5B%5D=33&org_type%5B%5D=35&org_type%5B%5D=5&org_type%5B%5D
=1&org_type%5B%5D=3&org_type%5B%5D=20&org_type%5B%5D=19&form_submit=1,
accessed 7 March 2023
Bangladesh, Government of People's Republic of Bangladesh, Facility Registry [tab for
Secondary Health Care], 2023, http://facilityregistry.dghs.gov.bd/, accessed 7 March 2023
Bangladesh, Government of People's Republic of Bangladesh, Facility Registry [tab for Tertiary
Health Care], 2023, http://facilityregistry.dghs.gov.bd/, accessed 7 March 2023
Bangladesh, Government of the People’s Republic of Bangladesh, Local Government
(Paurashava) Act 2009, 2009,
https://oldweb.lged.gov.bd/UploadedDocument/UnitPublication/10/112/PaurashavaAct2009.do
c, accessed 26 January 2023
Bangladesh, Government of the People’s Republic of Bangladesh, ,
[Local Government (City Corporation) Act, 2009 (Act No. 60 of 2009)],
2009, available at: http://www.clcbd.org/document/535.html, accessed 3 February 2023

EUROPEAN UNION AGENCY FOR ASYLUM
50
Bangladesh, IDRA (Insurance Development and Regulatory Authority), Annual Report, 2018-
2019 and 2019-2020, n.d.,
http://www.idra.org.bd/sites/default/files/files/idra.portal.gov.bd/annual_reports/d40ac24d_22
94_435f_8b35_5223f794a087/2023-02-22-09-36-
82e078d51b665eaed9a5f78f444c2e73.pdf, accessed 24 February 2023
Bangladesh, MOF (Ministry of Finance), Chapter 6 Medical Education and Family Welfare
Division, 2022,
https://mof.portal.gov.bd/sites/default/files/files/mof.portal.gov.bd/page/3ef1111d_f0d6_41ea_a
ca9_6afb61228825/G-1_05_74_Medical%20%20Edication_English.pdf, in: ,
- [Annual Report, Financial Year 2021-2022], October 2022,
https://mof.portal.gov.bd/sites/default/files/files/mof.portal.gov.bd/page/5cd219b8_9aec_4d5f
_a703_7f87e8e57b51/Annual%20Report%202021-22%20pdf%20f.pdf, accessed
8 March 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), 4th Health, Population and
Nutrition Sector Program 2017-2022, Operational Plan, Hospital Services Management
(January 2017 - June 2022), April 2017, http://hospitaldghs.gov.bd/wp-
content/uploads/2020/01/HSM_OP_2017-22.pdf, accessed 10 January 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), ADRM, DGDA (Directorate General
of Drug Administration), Pharmacovigilance Newsletter, 8
th
Issue, March 2022,
http://dgdagov.info/index.php/newsletter/2392-pharmacovigilance-newsletter-issue-8/file,
accessed 5 January 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), Bangladesh National Health
Accounts, 1991-2001, December 2003,
http://oldweb.heu.gov.bd/pdf/Research%20Paper%20No.31.pdf, accessed 5 January 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), Central Medical Stores Depot
(CMSD), n.d., http://cmsd.gov.bd/site/page/1fb0e2c4-b44b-48cb-9338-e17962c34b57/-,
accessed 7 February 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), Community Based Health Care,
DGHS, 2018, http://www.communityclinic.gov.bd, accessed 5 January 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), DGDA (Directorate General of
Drug Administration), Background, 6 March 2022, http://dgdagov.info/index.php/about-
dgda/background, accessed 10 March 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), DGDA (Directorate General of
Drug Administration), (Draft) Guideline on Antimicrobial Consumption (AMC) Surveillance in
Bangladesh, July 2022, http://dgdagov.info/index.php/information-center/guidance-
documents/2340-amc-surveillance-guideline-for-comments/file, accessed 5 January 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), DGDA (Directorate General of
Drug Administration), [National Drugs Policy 2016],

HEALTHCARE PROVISION IN BANGLADESH
51
http://www.dgda.gov.bd/site/view/law/---
%20National%20Drug%20policy,%202005.%20Public%20Health%20Section-1, accessed
5 January 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), DGDA (Directorate General of
Drug Administration), Quality manual, Document #: NC-QA-QLM/001/21-07, 18 May 2021,
http://dgdagov.info/index.php/ncl/quality-manual/1674-quality-manual/file, accessed
29 November 2022
Bangladesh, MOHFW (Ministry of Health & Family Welfare), Expanding Social Protection for
Health: Towards Universal Coverage, Health Care Financing Strategy 2012–2032, September
2012, https://socialprotection.gov.bd/wp-content/uploads/2017/03/HCF-Strategy-Bd-2012-
2032.pdf, accessed 5 January 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), Health Bulletin 2019, June 2020,
https://old.dghs.gov.bd/images/docs/Publicaations/Health%20Bulletin%202019%20Print%20V
ersion%20(2)-Final.pdf, accessed 29 November 2022
Bangladesh, MOHFW (Ministry of Health & Family Welfare), Health Bulletin 2020, 2022,
https://old.dghs.gov.bd/images/docs/vpr/lhb_2020.pdf, accessed 7 March 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), Health Nutrition Population Sector
Strategic Investment Plan (HNPSIP), 2016 – 2021, February 2016,
http://hospitaldghs.gov.bd/wp-content/uploads/2019/11/HNP-SIP-Draft-3.0_Master-
Doc_27.02.2015-min.pdf, accessed 2 March 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), Health Population and Nutrition
Sector Development Program 2011-16, Program Implementation Plan, July 2011,
http://www.mohfw.gov.bd/index.php?option=com_docman&task=doc_download&gid=1641&la
ng=bn, accessed 8 March 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), Health, Population and Nutrition
Sector Development Program (HPNSDP), n.d.
http://www.mohfw.gov.bd/index.php?option=com_content&view=article&id=166&Itemid=150&l
ang=bn, accessed 5 January 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), National Health Care Standards,
January 2015, http://qis.gov.bd/wp-
content/uploads/2019/04/2017_02_26_1488073894_902rds_.pdf, accessed 29 November
2022
Bangladesh, MOHFW (Ministry of Health & Family Welfare), National Drug Policy, 5 May 2005,
https://www.who.int/docs/default-source/searo/hsd/edm/nmp-ban-2005-goweb-
ok.pdf?sfvrsn=101bc39d_2, accessed 9 January 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), Strategic Plan for Health
Population and Nutrition Sector Development Program (HPNSDP) 2011-16, 2011,

EUROPEAN UNION AGENCY FOR ASYLUM
52
http://www.mohfw.gov.bd/index.php?option=com_docman&task=doc_download&gid=1384&la
ng=bn, accessed 3 February 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), [Gazette
on National Drug Policy 2016], 2017,
http://www.dgda.gov.bd/sites/default/files/files/dgda.portal.gov.bd/law/f65ac2f6_bd35_4bda_
94fc_3322b04b4075/2021-10-26-05-26-5d0b9bdb903fe45aceb2f2b7e2453c56.pdf,
accessed 5 January 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), ,
[National Drugs Policy 2016], 2017,
http://www.dgda.gov.bd/sites/default/files/files/dgda.portal.gov.bd/law/f65ac2f6_bd35_4bda_
94fc_3322b04b4075/2021-10-26-05-26-5d0b9bdb903fe45aceb2f2b7e2453c56.pdf,
accessed 5 January 2023 f, accessed 5 January 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), [Mission of Health Services
Division], n.d., https://hsd.gov.bd/site/page/66a54e07-5541-48fd-a438-bd48472cebad/,
accessed 10 January 2023
Bangladesh, MOHFW (Ministry of Health & Family Welfare), [Health Services
Division], April 2012, https://hsd.gov.bd/site/organogram/8628956f-bdab-4f64-a7da-
d864b3cf830d/, accessed 5 January 2023
Bangladesh, MOHFW, , [Emergency Notice for Private
Hospitals, clinics and diagnostic centers], 5 September 2017,
http://103.247.238.81/hsmdghs/files/notice1.pdf, accessed 3 May 2023
Bangladesh, MOLGRDC (Ministry of Local Government, Rural Development and Cooperatives),
Local Government Division, National Urban Health Strategy 2014,
http://uphcp.gov.bd/cmsfiles/files/NUHS.pdf, accessed 5 January 2023
Bangladesh, NIPORT (National Institute of Population Research and Training), Ministry of
Health and Family Welfare, ICF, Bangladesh Demographic and Health Survey 2017-18,
October 2020, https://www.dhsprogram.com/pubs/pdf/FR344/FR344.pdf, accessed
2 February 2023
bdnews24.com, Bangladesh regulator orders private medical facilities to display registration
details, 2 September 2022, https://bdnews24.com/bangladesh/y4s747umhz, accessed
2 March 2023
Bonilla-Chacin, M.E., Hossain, R., Mahmud, S.H., Amin, N., Sarker, M.A.B., Sadat, M.A., Paul, S.,
Ahmed, S., Begum, T., Smith, O., Kumar, A., Pathways to Reduce Household Out-of-Pocket
Expenditure, Health, Nutrition and Population Discussion Paper, World Bank,
http://hdl.handle.net/10986/35658, accessed 7 March 2023

HEALTHCARE PROVISION IN BANGLADESH
53
BRAC (Bangladesh Rural Advancement Committee), The Good Feed, Health: Healthcare made
hassle-free: Micro health insurance, 12 September 2022, https://blog.brac.net/healthcare-
made-hassle-free-micro-health-insurance/, accessed 3 March 2023
Business Standard (The), Ministry for aiding private hospitals to cut patient bills, 21 September
2022, https://www.tbsnews.net/bangladesh/health/ministry-aiding-private-hospitals-cut-
patient-bills-500934, accessed 2 March 2023
Business Standard (The), Out-of-pocket spending on treatment rises further, 4 January 2023,
https://www.tbsnews.net/bangladesh/health/out-pocket-expenditure-treatment-increases-
further-562758, accessed 5 January 2023
Business Standard (The), Prices of 53 drugs hiked, 17 July 2022,
https://www.tbsnews.net/bangladesh/health/prices-53-drugs-hiked-459394, accessed
9 March 2023
Daily Star (The), Countering counterfeit medicine in Bangladesh, 27 February 2022,
https://www.thedailystar.net/health/news/countering-counterfeit-medicine-bangladesh-
2971806, accessed 7 March 2023
Daily Star (The), Patient Referral System: Still elusive after all these years, 23 January 2023,
https://www.thedailystar.net/news/bangladesh/news/patient-referral-system-still-elusive-after-
all-these-years-3227801, accessed 9 March 2023
Development Initiatives, Supporting longer term development in crises at the nexus, Lessons
from Bangladesh, April 2021,
https://devinit.org/documents/948/Supporting_longer_term_development_in_crises_at_the_n
exus_Lessons_from_Bangladesh.pdf, accessed 5 January 2023
Eckstein, D., Künzel, V., and Schäfer, L., Global Climate Risk Index 2021, German Watch,
January 2021,
https://www.germanwatch.org/sites/default/files/Global%20Climate%20Risk%20Index%20202
1_2.pdf, accessed 5 January 2023
EUAA (European Union Agency for Asylum), EUAA Country of Origin Information (COI) Reports
Writing and Referencing Guide, February 2023,
https://euaa.europa.eu/sites/default/files/publications/2023-
02/2023_02_EUAA_COI_Writing_and_Referencing_Guide_Rebranded.pdf, accessed
9 March 2023
EUAA (European Union Agency for Asylum), The EUAA Writing Guide, April 2022,
https://euaa.europa.eu/publications/euaa-writing-guide, accessed 9 March 2023
European Commission, Exchange rate (InforEuro), n.d., https://commission.europa.eu/funding-
tenders/procedures-guidelines-tenders/information-contractors-and-beneficiaries/exchange-
rate-inforeuro_en, accessed 9 March 2023
EUROPEAN UNION AGENCY FOR ASYLUM
54
Financial Express (The), Cut prices of emergency drugs to ease burden on commoners,
24 November 2022, https://thefinancialexpress.com.bd/trade/cut-prices-of-emergency-drugs-
to-ease-burden-on-commoners-1669264974, accessed 9 March 2023
Govindaraj, R., Raju, D., Secci, F., Chowdhury, S., Frere, J., Health and Nutrition in Urban
Bangladesh, Social Determinants and Health Sector Governance, World Bank, 2018,
https://openknowledge.worldbank.org/bitstream/handle/10986/29091/9781464811999.pdf?seq
uence=2&isAllowed=y, accessed 3 February 2023
Guardian (The), ‘Like an open prison’: a million Rohingya refugees still in Bangladesh camps
five years after crisis, 23 August 2022, https://www.theguardian.com/global-
development/2022/aug/23/five-years-rohingya-refugees-2017-bangladesh-myanmar-military-
crackdown, accessed 3 March 2023
icddr,b, (International Centre for Diarrhoeal Disease Research, Bangladesh), Licensing is the
gateway to improving quality of services at private health facilities: finds an icddr,b
assessment, 30 August 2022, https://www.icddrb.org/quick-links/press-
releases?id=135&task=view, accessed 2 March 2023
International Crisis Group, A Sustainable Policy for Rohingya Refugees in Bangladesh
Brussels, Belgium, 2019, https://icg-prod.s3.amazonaws.com/303-a-sustainable-policy-for-
rohingya.pdf, accessed 3 February 2023
IT Medicus, Drug Information Management System (DIMS), 2022, proprietary software
available to download at: https://dimsbd.com/, accessed 9 March 2023
IT Medicus, What is DIMS Gateway, 2022, https://dimsbd.com/gateway-registration, accessed
9 March 2023
Kasonde, L., Tordrup, D., Naheed, A., Zeng, W., Ahmed, S., Babar, Z. Ud-Din, Evaluating
medicine prices, availability and affordability in Bangladesh using World Health Organisation
and Health Action International methodology, in: BMC Health Services Research, Vol. 19,
Number 383, 2019, http://dx.doi.org/10.1186/s12913-019-4221-z, accessed 3 March 2023
Khan, M.R., Roddick, S., Roberts, E., Assessing Microinsurance as a Tool to Address Loss and
Damage in the National Context of Bangladesh, Loss and Damage in Vulnerable Countries
Initiative, June 2013, https://www.gov.uk/research-for-development-outputs/assessing-
microinsurance-as-a-tool-to-address-loss-and-damage-in-the-national-context-of-
bangladesh#citation, accessed 26 January 2023
Mamun, M., The Effectiveness of Microinsurance in Bangladesh: Can It Sustain?, in:
International Review of Financial Consumers, Vol 2, Issue 1: 7-16, April 2017,
http://dx.doi.org/10.36544/irfc.2017.1-1.2, accessed 5 January 2023
New Age Bangladesh, Counterfeit medicines flood markets across Bangladesh,
25 September 2021, https://www.newagebd.net/article/150157/counterfeit-medicines-flood-
markets-across-bangladesh, accessed 7 March 2023

HEALTHCARE PROVISION IN BANGLADESH
55
New Age Bangladesh, Increase in drug prices adds to people’s economic burden, Opinion, 19
July 2022, https://www.newagebd.net/article/176166/increase-in-drug-prices-adds-to-peoples-
economic-burden, accessed 9 March 2023
Pavel, M.S., Chakrabarty S, Gow J., Cost of illness for outpatients attending public and private
hospitals in Bangladesh, in: International Journal for Equity in Health, Vol 15, Number 167,
2016, http://dx.doi.org/10.1186/s12939-016-0458-x, accessed 21 January 2023
Prothomalo.com, Price of 53 essential medicines set to increase, 16 July 2022,
https://en.prothomalo.com/bangladesh/117b56hhm2, accessed 9 March 2023
Rabbani, A., Sarker, M., Understanding the effects of an employer-provided health security
program on the well-being, productivity, and health seeking behavior of workers in a semi-
formal manufacturing setting in Bangladesh International Growth Center, IGC, 2017,
https://www.theigc.org/project/understanding-the-effects-of-an-employer-provided-health-
security-program-on-the-well-being-productivity-and-health-seeking-behavior-of-workers-in-a-
semi-formal-manufacturing-setting-in-bangladesh/, accessed 5 January 2023
Rahman, M.M., Islam, M.R., Rahman, M.S., Hossain, F., Alam, A., Rahman O., Jung J., Akter S.,
Forgone healthcare and financial burden due to out-of-pocket payments in Bangladesh: a
multilevel analysis, in: Health Economics Review, Vol 12, Number 5, 2022,
http://dx.doi.org/10.1186/s13561-021-00348-6, accessed 2 March 2023
Rahman, M.S., Yoshida, N., Tsuboi, H., Karmoker, J.R., Kabir, N., Schaefermann, S., Akimoto, Y.,
Bhuiyan, M.A., Reza, S., Kimura, K., A comprehensive analysis of selected medicines collected
from private drug outlets of Dhaka city, Bangladesh in a simple random survey, in: Scientific
Reports, Vol 12, Number 234, 2022, https://doi.org/10.1038/s41598-021-04309-1, accessed
7 March 2023
Rahman, T., Gasbarro, D., Alam K., Financial risk protection in health care in Bangladesh in the
era of Universal Health Coverage, in: PLoS ONE, Vol 17, Issue 6, 2022,
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0269113, accessed 7 February
2023
Rashid, R., Shamsu Uddin, A.M., Pu Chaw Nu, Salam, A. Barua, S., Mannan, A., Shahjahan, M.,
Ahmed, M., Rahman, R., Dondorp, A., Maude, R., Deen J., Seidlein L. & Abul Faiz, M., A
descriptive study of Forcefully Displaced Myanmar Nationals (FDMN) presenting for care at
public health sector hospitals in Bangladesh, in: Global Health Action, Vol 14, Issue 1, 2021,
available at: http://dx.doi.org/10.1080/16549716.2021.1968124, accessed 3March 2023
Sarker, A.R., Ali, S.M.Z., Ahmed, M., Chowdhury, S.M.Z.I., Ali, N., Out-of-pocket payment for
healthcare among urban citizens in Dhaka, Bangladesh, in: PLOS ONE, Volume 17, Issue 1, 24
January 2022, https://doi.org/10.1371/journal.pone.0262900, accessed 8 March 2023
Shafique, S., Saif-Ur-Rahman, K.M., Kamruzzaman, Hossain, T., Mamun, R., Akhter, S., Rahman,
A., Hossain, S., Koot, J., Anwar, I., Epidemiological Transition and Non-Communicable
Diseases among Urban Poor in Bangladesh: A Knowledge Synthesis, Strengthening Health
Applying Research Evidence (SHARE) Project, Universal Health Coverage Programme, Health

EUROPEAN UNION AGENCY FOR ASYLUM
56
System and Population Studies Division, 2019, https://europa.eu/capacity4dev/capacity-
building-in-public-health-for-development/documents/share-bangladesh-epidemiological-
transition-and-non-communicable-diseases-among-urban-poor, accessed 20 January 2023
Sheikh, N., Tagoe, E.T., Akram, R., Ali, N., Howick, S., Morton, A., Implementation barriers and
remedial strategies for community-based health insurance in Bangladesh: insights from
national stakeholders, in: BMC Health Services Research, 2022, Volume 22, Issue 1,
http://dx.doi.org/10.1186/s12913-022-08561-7, accessed 8 February 2023
Sultana, D., Kaisar, F., Nazrul, S., Evolution of Micro Insurance in Bangladesh: Financial
Cushion for the Bottom of the Pyramid Population, 2021,
https://www.lightcastlebd.com/insights/2021/05/evolution-of-micro-insurance-in-bangladesh-
financial-cushion-for-the-bottom-of-the-pyramid-population/, accessed 5 January 2023
UN (United Nations), Bangladesh - Map No. 3711 Rev.1, October 2003,
https://www.un.org/geospatial/content/bangladesh-1, accessed 29 November 2022
UNOCHA (United Nations Office for the Coordination and Humanitarian Affairs), Rohingya
Refugee Crisis, n.d., https://www.unocha.org/rohingya-refugee-crisis, accessed 26 January
2023
USAID, Research Brief Evaluation of the Pilot Shasthyo Shurokhsha Karmasuchi (SSK), n.d.,
http://rdm.icddrb.org/wp-content/uploads/2021/07/Brief-on-evaluation-of-SSK-study.pdf,
accessed 29 November 2022
Werner, W.J., Micro-insurance in Bangladesh: Risk Protection for the Poor? in: Journal of
Health, Population and Nutrition, Vol 27, Issue 4, 2009,
http://dx.doi.org/10.3329/jhpn.v27i4.3402, accessed 5 January 2023
WHO (World Health Organization), Current health expenditure as a percentage of Gross
Domestic Product (GDP) - Bangladesh, Global Health Expenditure Database, n.d.,
https://apps.who.int/nha/database/ViewData/Indicators/en, accessed 7 March 2023
WHO (World Health Organization), Current health expenditure per capita (current USD) -
Bangladesh, Global Health Expenditure Database, n.d.,
https://apps.who.int/nha/database/ViewData/Indicators/en, accessed 7 March 2023
WHO (World Health Organization), Household out-of-pocket payment as a % of Current health
expenditure (CHE) - Bangladesh, Global Health Expenditure Database, n.d.,
https://apps.who.int/nha/database/ViewData/Indicators/en, accessed 7 March 2023
WHO (World Health Organization), Household out-of-pocket payment in current US$ per
Capita - Bangladesh, Global Health Expenditure Database, n.d.,
https://apps.who.int/nha/database/ViewData/Indicators/en, accessed 7 March 2023
WHO (World Health Organization), Regional Office for the Western Pacific, Bangladesh Health
System Review, Health systems in transition, Vol 5, Issue 3, 2015,
https://apps.who.int/iris/handle/10665/208214, accessed 6 February 2023

HEALTHCARE PROVISION IN BANGLADESH
57
World Bank (The) Data, Life expectancy at birth, total (years) – Bangladesh, 2023,
https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=BD, accessed 2 March 2023
World Bank (The), Bangladesh Country Climate and Development Report (CCDR), October
2022, https://openknowledge.worldbank.org/bitstream/handle/10986/38181/CCDR-
Bangladesh-MainReport.pdf, accessed 2 February 2023
World Bank (The), Current health expenditure (% of GDP), 2023,
https://databank.worldbank.org/metadataglossary/health-nutrition-and-population-
statistics/series/SH.XPD.CHEX.GD.ZS, accessed 7 March 2023
World Bank (The), Data, Rural population (% of total population) - Bangladesh, 2023,
https://data.worldbank.org/indicator/SP.RUR.TOTL.ZS?locations=BD, accessed 2 February
2023
World Bank (The), Groundswell: Preparing for Internal Climate Migration, 2018
https://openknowledge.worldbank.org/handle/10986/29461, accessed 2 March 2023
World Bank (The), Health expenditure, total (% of GDP), 2023,
https://databank.worldbank.org/metadataglossary/world-development-
indicators/series/SH.XPD.TOTL.ZS, accessed 7 March 2023
World Bank (The), Population density (people per sq. km of land area) - Bangladesh, 2023,
https://data.worldbank.org/indicator/AG.SRF.TOTL.K2?locations=BD, accessed 7 March 2023
World Bank (The), Population Total Bangladesh, 2022,
https://data.worldbank.org/indicator/SP.POP.TOTL?locations=BD, accessed 10 January 2023
World Bank (The), Surface area (sq. km) - Bangladesh, 2023,
https://data.worldbank.org/indicator/AG.SRF.TOTL.K2?locations=BD, accessed 7 March 2023
World Bank (The), The World Bank in Bangladesh, 6 October 2022,
https://www.worldbank.org/en/country/bangladesh/overview#1, accessed 7 March 2023

EUROPEAN UNION AGENCY FOR ASYLUM
58
Annex 2: Terms of Reference
General information
Avoid general Country of Origin Information (COI), focus on aspects that have an impact on
healthcare.
This section is devoted to the geographic, demographic, political and/or economic contexts
which are relevant to analyse the health system in the country in question. If possible, explain
the impact of these factors on the accessibility of healthcare. Ensure that in this section are
included all particular aspects that can have an impact on the provision of healthcare in the
country. (e.g., security situation, internally displaced people (IDPs) / refugees, ethnic tensions,
etc.).
Healthcare system
Health system organisation
a) Overview
How is the healthcare system organised (e.g., organised as primary, secondary and tertiary
healthcare)? If so, could you explain who provides care at each level and what type of care is
provided at each level? Does a system of referrals and counter referrals exist?
Is the healthcare system centralised, decentralised or federal? How are the healthcare
jurisdictions distributed between the levels of power? How is the health sector financing
distributed between the levels of power? In the cases of states with federal / confederal
structure, if the care is not available in the state / region/republic of residence of the patient,
but is however available in another federated state (region / republic) of the same country, is
there a possibility for the patient to be transferred there? Is there a mandatory referral system?
What are the conditions?
Is there recent data on the geographical distribution of the health structures? If so, could you
give an overview? Is there a difference in the care supply, in respect to the different
healthcare levels, in the urban and rural regions? Do the patients in the urban and rural zones
have equal access to healthcare? Are there regions / provinces particularly affected by a lack
of hospitals or health centres? Ensure that there is Information on the number of healthcare
facilities at each level of healthcare.
Use links to existing documents online for more detailed information.
b) Public sector
How is the public sector structured? What are the strengths? What are the weaknesses?

HEALTHCARE PROVISION IN BANGLADESH
59
c) Private sector
Does a private health sector exist? How is it structured? Is there a difference (quantitatively
and qualitatively) between hospitals and health structures in the public and private sector?
What are the main differences, for the patient looking for medical care, between the state-
financed healthcare system and the private sector?
Healthcare resources
Is there recent data on the number of healthcare personnel in the country (e.g., cardiologists,
psychologists, etc. per number of inhabitants)? If so, provide a brief overview (context /
comparison with other similar countries or Europe)?
How is the distribution of human resources in health care in the country? Are there regions /
provinces particularly affected by a shortage of healthcare professionals? Is the distribution of
the healthcare personnel equal between the public and private sectors?
Are there any specific needs with regards to human resources for health? Are there any
under-represented professional categories? Could you specify?
Is there an emergency healthcare service, e.g., ambulances? How is it organised?
Health expenditure / GDP.
Pharmaceutical sector
Is there a national essential drugs list for the country? What does it mean in terms of access to
drugs for patients? How often is the list updated? If generic drugs are not widely available, do
patients have access to generic drugs? Are they accessible to patients and how?
Is there a supply system for drugs? Does the country experience regular stock shortages? If
so, does it affect the patients’ access to medication? What drugs and diseases are mainly
affected by these stock shortages? What organisations regulate / control the market? Are
there many illegal medications in circulation?
Are the drugs accessible both in urban and rural areas? Are the drugs accessible
geographically in all the country's regions?
Are any medications only available in hospitals, not pharmacies? If so which ones?
Can non-registered medication be imported (parallel import)? How?
Patient’s pathways
In general: when in need of medical treatments and/or medicines, where and how can patients
find information? What is the ‘typical route’ of a patient who needs healthcare; treatments
and/or medicines? What does he/she do and where does he/she go primarily and what

EUROPEAN UNION AGENCY FOR ASYLUM
60
happens next? What are the main obstacles in general to access medical treatments /
medicines in the country?
Economic factors
Risk-pooling mechanisms
Include only the mechanisms which are relevant to the country in question. Remove section if
there are none.
Health services provided by the State / Public authorities
Is there a national health and social insurance system / certain state coverage in the country?
How is the Public Health / Social Insurance system organised?
How is health insurance financed? Is it financed by the employer and/or employee
contribution or by taxation or by OOP (out of pocket payments)? What is the patient's financial
contribution?
What does it consist of? Who is entitled to public health insurance (or other form of public /
state coverage)? Is the entire population entitled to this insurance? If not, what are the
administrative procedures that should be undertaken and/or the conditions that are necessary
in order to be registered with health insurance? Are the procedures identical for the entire
population? Is being employed one of the conditions to qualify for health insurance? Does the
health coverage target certain groups of the population (pregnant women, children, seniors,
etc.)? What are the criteria in order to be covered by public health insurance? Is a patient’s
financial participation necessary for the registration? If so, how much should they pay? What
percentage of the population is covered by public health insurance?
Does the country have a complementary system to protect the most vulnerable and those
who cannot contribute or be enrolled in the National Health insurance?
Are returning migrants / citizens covered by public health insurance?
Public health insurance, national or state coverage
Note for drafters: the aim of this section is to make clear to the reader what is covered by
public health insurance and to what extent it is covered. Below are guiding aspects to take
into account.
What type of healthcare / what diseases does health insurance cover? Is maternity care
covered by health insurance? Where is the healthcare provided (in which healthcare facility or
at what level of the health pyramid structure)?

HEALTHCARE PROVISION IN BANGLADESH
61
Are medicines covered by health insurance? Does it cover all medicines or only some of them
or only a percentage of the cost? What are the conditions to benefit from drug coverage?
Are there cash benefits in case of illness for employees? If so, in which cases and conditions
and what is the amount of these benefits?
In case a patient needs medical care and does not have the means to pay, are there any
governmental measures allowing them access to healthcare? Is there a difference between
emergency care and non-emergency care? What are the solutions for patients without
financial resources?
Community-based health insurance schemes
Are there community-based health insurances in the country? What are the conditions to
register? Which are the practical steps to register? How much must an average person / family
pay to become a member? Do all community-based health insurances offer the same
coverage and have the same mechanism?
Which risks are covered? What type of healthcare, what diseases do the community-based
health insurances cover? Where is the healthcare provided (in which healthcare facility or at
what level of the health pyramid structure)? Are the drugs covered by community-based
health insurance? Does the insurance cover all drugs or only some of them or only a
percentage of the cost? Are there conditions to benefit from the coverage? Does the patient
have to participate financially in order to have access to care (co-payment)? What is the
recovery rate for the medical costs?
What is the percentage of population’s coverage by the community-based health insurances?
Private health insurance schemes
Are there private health insurance systems? What are the main health insurances in the
country? What are the conditions necessary to benefit from them?
What do these health insurances cover? What type of healthcare, which diseases are
covered? Where is the healthcare provided (in which healthcare facility or at which level of the
health pyramid structure)?
How much must a person / family pay to obtain a private insurance on average?
What is the percentage of the population’s coverage by private health insurances? Who has
access to this type of insurance?
Out-of-pocket health expenditure
Average total of out-of-pocket payment on total health expenditure.
Information on the frequency of health expenditure events that may bankrupt a person /
family.

EUROPEAN UNION AGENCY FOR ASYLUM
62
a) Cost of consultations
Provide a range of prices for consultations with a general practitioner and different specialists
as well as for a hospital stay. What is the price of a consultation / hospitalisation in an
emergency department? What is the share of financial participation by patients?
Is there a difference in respect to prices between the private and public facilities? Are there
any geographical disparities?
Is there a practice of overcharging medical fees? Is it common? If so, could you explain the
context? How much does it amount to?
b) Cost of medication
General information about the prices of medication: Are the prices regulated? Is there an
inflation problem, price variation, etc.?
Are there medications provided for free (e.g., are certain medicines covered by the state)? If
so, could you specify which ones and in what facilities or at what health level?
In general, what share of the health budget per person / family goes to the purchase of drugs?
Does the price of medication vary between pharmacies? Is there a difference in respect to
prices between the private and public facilities? Are there any geographical disparities?
List of useful links
Include links that provide long-term value and are likely to be kept updated, such as websites
detailing epidemiologic data, national disease programmes, Ministry of Health website, certain
large hospitals, online pharmacies, etc. Not e.g., individual research articles or other ‘static’
material.


