
CONTRACTOR PROJECT REPORT
Developing Health Equity Measures
Prepared for
the Office of the Assistant Secretary for Planning and Evaluation (ASPE)
at the U.S. Department of Health & Human Services
by
RAND Health Care
May 2021

ii
Office of the Assistant Secretary for Planning and Evaluation
The Assistant Secretary for Planning and Evaluation (ASPE) advises the Secretary of the U.S.
Department of Health and Human Services (HHS) on policy development in health,
disability, human services, data, and science; and provides advice and analysis on economic
policy. ASPE leads special initiatives; coordinates the Department's evaluation, research,
and demonstration activities; and manages cross-Department planning activities such as
strategic planning, legislative planning, and review of regulations. Integral to this role, ASPE
conducts research and evaluation studies; develops policy analyses; and estimates the cost
and benefits of policy alternatives under consideration by the Department or Congress.
Office of Health Policy
The Office of Health Policy (HP) provides a cross-cutting policy perspective that bridges
Departmental programs, public and private sector activities, and the research community, in
order to develop, analyze, coordinate and provide leadership on health policy issues for the
Secretary. HP carries out this mission by conducting policy, economic and budget analyses,
assisting in the development and review of regulations, assisting in the development and
formulation of budgets and legislation, and assisting in survey design efforts, as well as
conducting and coordinating research, evaluation, and information dissemination on issues
relating to health policy.
ASPE Project Team
Rachael Zuckerman, Lok Samson, Wafa Tarazi, Victoria Aysola, and Oluwarantimi Adetunji
This research was funded by the U.S. Department of Health and Human Services Office of the
Assistant Secretary for Planning and Evaluation under Contract Number HHSP233201500038I
and carried out by RAND Health Care. Please visit https://aspe.hhs.gov/social-risk-factors-and-
medicares-value-based-purchasing-programs for more information about ASPE research on
social risk factors and Medicare's value-based purchasing programs.

iii
ASPE Executive Summary
In 2014, under the Improving Medicare Post-Acute Care (IMPACT) Act, Congress asked that
ASPE study the relationship between social risk factors
1
and Medicare’s value-based
purchasing (VBP) programs. ASPE wrote two Reports to Congress, making recommendations
based on the studies’ findings. This included the recommendations that the Centers for
Medicare and Medicaid Services (CMS) include measures of health equity in public reporting
and VBP programs. Moreover, in the ASPE commissioned report, Systems Practices for the
Care of Socially At-Risk Populations, the National Academies of Sciences, Engineering, and
Medicine calls out a commitment to health equity as one of six promising practices to
improve care for socially at-risk populations.
2
However, as Medicare’s VBP programs do not currently include health equity measures,
appropriate measures need to be developed and/or identified before they can be
incorporated into these programs. In response to this challenge, ASPE asked the RAND
Corporation to develop a proposed definition of health equity as a starting place and to
identify existing health equity measurement approaches that may be suitable for inclusion
in Medicare’s VBP programs, quality reporting efforts, and confidential reports. RAND
identified 10 existing approaches to health equity measurement and convened a technical
expert panel (TEP) to:
(1) provide feedback on the project team’s proposed definition of a health equity measure
and identification of features of health equity measurement approaches;
(2) develop a set of criteria for evaluating health equity measurement approaches for
potential inclusion in Medicare’s VBP programs, quality reporting efforts, and confidential
reports; and
(3) evaluate the set of health equity measurement approaches identified by the team
according to these criteria.
Based on input from RAND, ASPE, and the TEP, in this report RAND defines a health equity
measurement approach as “an approach to illustrating or summarizing the extent to which
the quality of health care provided by an organization contributes to reducing disparities in
health and health care at the population level for those patients with greater social risk
factor burden by improving the care and health of those patients.” We note that this
definition focuses on health care quality, as that was the charge from Congress under the
IMPACT Act, but measurement approaches could be considered more broadly in other
contexts.
The purpose of including health equity measurement approaches in VBP programs and
quality reporting efforts is to motivate a focus on improving health for all by reducing
disparities and to help providers prioritize particular areas for quality improvement. It could
also encourage providers to improve health equity through service enhancements, patient
engagement activities, and adoption of best practices.
Of the 10 health equity measurement approaches evaluated by the TEP (which are
described in detail in the report itself), the CMS Office of Minority Health’s (OMH) Health
Equity Summary Score (HESS) received the highest ratings from the TEP overall. This
1
The term “social risk factors” was suggested by the National Academies of Sciences, Engineering, and
Medicine as discussed below.
2
National Academies of Sciences, Engineering, and Medicine. 2016. Systems practices for the care of socially
at-risk populations. Washington, DC: The National Academies Press.

iv
approach first identified those patient experience and clinical care measures that are most
suitable for health equity comparisons. Then, the HESS assessed the extent to which care
provided through Medicare Advantage contracts was equitable based on race, ethnicity,
and dual/low-income subsidy (LIS) eligibility status. The HESS combines data across multiple
performance measures, multiple social risk factors, and multiple types of comparisons to
create a summary index of health equity.
The Biden-Harris Administration has emphasized the importance of equity across the
government, and health equity in particular. This report directly responds to Executive
Order 13985, Advancing Racial Equity and Support for Underserved Communities Through
the Federal Government, which asks all federal agencies to “identify the best methods,
consistent with applicable law, to assist agencies in assessing equity with respect to race,
ethnicity, religion, income, geography, gender identity, sexual orientation, and disability.”
3
Although this report focuses on the Medicare program, much of the findings are applicable
more broadly, including the definition of a health equity measurement approach, the
criteria that were developed for evaluating health equity measures, and the TEP’s discussion
of the measures identified.
Going forward, the health equity measures identified and evaluated in this report can
contribute to HHS implementation of Executive Order 13985 and the recommendations in
the Report to Congress on the Role of Social Risk in Medicare’s Value-Based Purchasing
Programs.
4
A Note on Social Risk Factors, Race, and Ethnicity
Although the IMPACT Act required that ASPE study “the effect of individuals’ socioeconomic
status on quality measures,” ASPE commissioned a series of reports from the National
Academies of Science, Engineering, and Medicine who suggested that the term “social risk
factors” was more appropriate and provided a conceptual model that listed the specific
domains and risk factors.
5
ASPE’s Reports to Congress and follow-on work, including this
report, have used the term social risk factors and the specific factors identified.
4
In more
recent years, there has been further discussion on appropriate terminology, including
understanding the distinctions between social determinants of health, social risk factors,
and social needs.
6,7
This continuing discussion shows the interconnectedness of these
concepts, while also recognizing that not all characteristics and needs can or should be
addressed in the same way.
The social risk factors identified by the National Academies of Science, Engineering, and
Medicine include the domains of socioeconomic position; race, ethnicity, and cultural
context; gender; social relationships; and residential and community context. These
3
See https://www.federalregister.gov/documents/2021/01/25/2021-01753/advancing-racial-equity-and-
support-for-underserved-communities-through-the-federal-government
4
See all of ASPE’s work on this topic at https://aspe.hhs.gov/social-risk-factors-and-medicares-value-based-
purchasing-programs
5
National Academies of Sciences, Engineering, and Medicine. 2016. Accounting for social risk factors in
Medicare payment: Identifying social risk factors. Washington, DC: The National Academies Press.
6
Alderwick, H. and Gottlieb, L.M., 2019. Meanings and misunderstandings: a social determinants of health
lexicon for health care systems. The Milbank Quarterly, 97(2), p.407.
7
Green, K. and Zook M., 2019. When Talking About Social Determinants, Precision Matters. Health Affairs
Blog, October 29. Available at https://www.healthaffairs.org/do/10.1377/hblog20191025.776011/full/.
v
domains and the individual factors within them were identified based on existing evidence
of the association between the factor and worse health outcomes. We note that the factors
identified include both modifiable social determinants of health, and also additional, non-
modifiable factors such as race and ethnicity, which are themselves not causal factors for
disparities but are subject to structural inequities that produce adverse health outcomes.
The Biden-Harris Administration’s emphasis on health equity brings an additional
perspective to this issue. In addressing health equity, we in the federal government include
many of the same factors that the National Academies of Science, Engineering, and
Medicine identified as social risk factors. We take a slightly different perspective than
presented by National Academies of Science, Engineering, and Medicine and consider non-
modifiable factors such as race, ethnicity, and rural location as associated with health
disparities, but not risk factors themselves or drivers of those disparities. We are interested
in identifying non-modifiable factors, such as race and ethnicity, to assess differential health
outcomes. We also focus on modifiable factors, such as structural racism, that are the
drivers of the outcome differences. Addressing health equity issues requires implementing
interventions to address the drivers of outcome differences and monitoring outcomes to
determine whether equity improved. Such monitoring is built on the health equity
measurement approaches evaluated in this report.

Project Report
Developing Health Equity Measures
Steven C. Martino, Sangeeta Ahluwalia, Jordan Harrison, Alice Kim, Marc N. Elliott
RAND Health Care
January 2021
Prepared for ASPE
vii

viii
Preface
Socially at-risk individuals receive lower-quality health care and experience worse
health outcomes than more advantaged individuals. One way to address this in the
Medicare population is to use Medicare’s value-based purchasing (VBP) programs,
quality reporting efforts, and confidential reports as tools to drive improvements in
quality. In particular, including health equity measurement approaches in VBP
programs and quality reporting could motivate providers to focus on reducing
disparities and to prioritize particular areas for quality improvement. It could also
encourage providers to improve health equity through service enhancements, patient
engagement activities, and adoption of best practices.
In this project, RAND Corporation researchers identified existing health equity
measurement approaches that might fit with Medicare’s VBP programs, quality
reporting efforts, and confidential reports. The project had two objectives: (1) identify
health equity measurement approaches, and (2) decide which of these approaches
merit consideration for inclusion in Medicare’s VBP programs, quality reporting efforts,
and confidential reports. This report describes the methods and findings of the project
and delineates potential first steps for the U.S. Department of Health and Human
Services to consider as it continues to evaluate the prospect of incorporating health
equity measures and domains in Medicare’s VBP and reporting programs.
This research was funded by the Office of the Assistant Secretary for Evaluation and
Planning in the U.S. Department of Health and Human Services and carried out within
the Payment, Cost, and Coverage Program in RAND Health Care.
RAND Health Care, a division of the RAND Corporation, promotes healthier societies
by improving health care systems in the United States and other countries. We do this
by providing health care decisionmakers, practitioners, and consumers with actionable,
rigorous, objective evidence to support their most complex decisions. For more
information, see www.rand.org/health-care or contact
RAND Health Care Communications
1776 Main Street
P.O. Box 2138
Santa Monica, CA 90407-2138
(310) 393-0411, ext. 7775
RAND_Health-[email protected]

Contents
Preface ................................................................................................. Error! Bookmark not defined.ii
Contents ................................................................................................................................................................ ix
Figures ................................................................................................................................................................... xi
Ta bles ................................................................................................................................................................... xii
Abbreviations ................................................................................................................................................... xiii
Summary ............................................................................................................................................................ xiv
1. Background and Purpose ........................................................................................................................... 1
!"#$%&'()* ...................................................................................................................................................... 1
+&',-#./ 01,-#.23-4 ........................................................................................................................................... 2
2. Literature Review Methods and Results ............................................................................................. 4
Definition of a Health Equity Measurement Approach to Assess Organizational
Contributions ........................................................................................................................................... 4
Search Strategy .............................................................................................................................................. 4
562%21262.7/ 8&2.-&2" .......................................................................................................................................... 5
9&.2#6-:;-<'&. /=#&--)2)% ............................................................................................................................ 5
3. Detailed Information on Identified Approaches ........................................................................... 12
Measurement Framework for Evaluating How Well an Organization Meets National
CLAS Standards (HHS OMH) .......................................................................................................... 12
NQF Disparities-Sensitive Measure Assessment .......................................................................... 14
AHRQ >".2')"6/ ?-"6.@#"&-/ A("62.7/ ")* /B24<"&2.2-4 /;-<'&. ...................................................... 16
CM S OMH Mapping Medicare Disparities Tool ............................................................................. 18
CMS OMH Reporting of CAHPS and HEDIS Data Stratified by Race and Ethnicity for
Medicare Beneficiaries ..................................................................................................................... 19
C2))-4'." /?-"6.@#"&-/ B24<"&2.2-4 /;-<'&. ......................................................................................... 20
CMS Assessment of Hospital Disparities for Dual-Eligible Patients ..................................... 22
CMS OMH Health Equity Summary Score ........................................................................................ 24
Zimmerman Health-Related Quality of Life Approach to Assessing Health Equity ...... 27
Zimmerman and Anderson Approach to Evaluating Trends over Time in Health
Equity ....................................................................................................................................................... 28
4. Summary of Identified Health Equity Measurement Approaches ........................................ 29
5. Technical Expert Panel Process and Members .............................................................................. 33
6. TEP Input on Project Framing and Approach ................................................................................ 34
Inp ut on Definition of a Health Equity Measurement Approach ........................................... 34
Input on Premise of the Project ........................................................................................................... 35
Input on Evaluation Criteria .................................................................................................................. 35
7. Detailed Assessment of Identified Approaches ............................................................................. 38
Measurement Framework for Evaluating How Well an Organization Meets National
CLAS Standards .................................................................................................................................... 38
NQF Disparities-Sensitive Measure Assessment .......................................................................... 41
9?;A />".2')"6 /?-"6.@#"&-/ A("62.7/ ")* /B24<"&2.2-4 /;-<'&. ....................................................... 42
CM S OMH Mapping Medicare Disparities Tool ............................................................................. 44
CMS OMH Reporting of CAHPS and HEDIS Data, Stratified by Race and Ethnicity, for
Medicare Beneficiaries ..................................................................................................................... 46
C2))-4'." /?-"6.@#"&-/ B24<"&2.2-4 /;-<'&. ......................................................................................... 48
CMS Assessment of Hospital Disparities for Dual-Eligible Patients ..................................... 50
ix
CMS OMH Health Equity Summary Score ........................................................................................ 52
Zimmerman Health-Related Quality of Life Approach to Assessing Health Equity ...... 54
Zimmerman and Anderson Approach to Evaluating Trends over Time in Health
Equity ....................................................................................................................................................... 56
8. Summary and Key Takeaways .............................................................................................................. 59
=(DD"&7 ........................................................................................................................................................ 59
E-7/ F"$-"G"74 ............................................................................................................................................. 60
Appendix A. Ambulatory, Hospital, Behavioral Health, and Public Health Measures
Identified as Part of the Measurement Framework for Evaluating How Well an
Organization Meets National CLAS Standards (HHS OMH) ................................................... 62
Appendix B. Measures Identified as Disparities-Sensitive According to the NQF
Disparities-Sensitive Measure Assessment .................................................................................. 64
Appendix C. Biographical Information on Expert Panelists ......................................................... 67
x

Figures
Figure 2. 1. Literature Review F low Diagram ...................................................................................... 10
Figure 3.1. NQF Disparities-Sensitive Measure Identification................................ ..................... 15
Figure 4.2. Components of the HESS ....................................................................................................... 26
Figure 4.3. HESS: Blending Scheme ......................................................................................................... 26
xi

Tables
Ta ble S.1. Ten Identified Approaches to Health Equity Measurement ................................... xix
Ta ble 2.1. Database Search Strategy ......................................................................................................... 7
Table 2.2. Summary of the Health Equity Measurement Approaches Identified by the
Literature Review .................................................................................................................................. 11
Table 3.1. Cross-Cutting Measures to Evaluate How Well an Organization Meets National
CLAS Standards ...................................................................................................................................... 13
Ta ble 4.1. Summary of Identified Approaches to Health Equity Measurement ................... 32
Table 7.1. TEP Ratings of Measurement Framework for Evaluating How Well an
Organization Meets National CLAS Standards .......................................................................... 40
Table 7.2. TEP Ratings of NQF Disparities-Sensitive Measure Assessment .......................... 42
Table 7.3. TEP Ratings of 9?;A/ >".2')"6/ ?-"6.@#"&-/ A("62.7/ ")*/ B24<"&2.2-4/ ;-<'&. ....... 44
Table 7.4. TEP Rat ings of CMS O MH Mapping Medicare Disparities Tool .............................. 46
Table 7.5. TEP Ratings of CMS OMH Reporting of CAHPS and HEDIS Data Stratified by
Race and Ethnicity for Medicare Beneficiaries ......................................................................... 48
Ta ble 7.6. TEP Ratings of Minnesota Healthcare Di sparities Report ........................................ 50
Table 7.7. TEP Ratings of CMS Assessment of Hospital Disparities for Dual-Eligible
Patients ...................................................................................................................................................... 52
Table 7.8. TEP Ratin gs of CMS OMH Health Equity Summary Score ........................................ 54
Table 7.9. TEP Ratings of Zimmerman Health-Related Quality of Life Approach to
Assessing Health Equity ..................................................................................................................... 56
Table 7.10. TEP Ratings of Zimmerman and Anderson Approach to Evaluating Trends
over Time in Health Equity ............................................................................................................... 58
xii

Abbreviations
AAC average annual change
AHRQ Agency for Healthcare Research and Quality
ASPE Assistant Secretary for Planning and Evaluation
CAHPS Consumer Assessment of Healthcare Providers and Systems
CINAHL Cumulative Index to Nursing and Allied Health Literature
CLAS Culturally and Linguistically Appropriate Services
CMS Centers for Medicare & Medicaid Se rvices
FFS fee- for -service
HEDIS Healthcare Effectiveness Data and Information Set
HESS Health Equity Summary Score
HHS U.S. Department of Health and Human Services
LIS Low -Income Subsidy
MA Medicare Advantage
MeSH Medical Subject Headings
MMD Mapping Me dicare D isparities
NQF National Quality Forum
OMH Office o f Mi nority Health
PDP prescription drug plan
RSRR risk -standardized readmission rate
TEP technical expert p anel
VBP value- based purchasing
xiii
- -
-
-
-

xiv
Summary
There is growing recognition that social risk factors
8
—such as income, education, race
and ethnicity, and community resources—play a major role in health.
9
Despite ongoing
efforts to address inequities, evidence suggests that socially at-risk individuals receive
lower-quality health care and experience worse health outcomes than more-advantaged
individuals. Medicare’s value-based purchasing (VBP) programs, quality reporting
efforts, and confidential reports to providers of their performance on quality measures
could be powerful tools to drive improvements in the quality of care provided to
socially at-risk individuals. In particular, including health equity measurement
approaches in VBP programs and quality reporting efforts could motivate a focus on
reducing disparities and help providers prioritize particular areas for quality
improvement. It could also encourage providers to improve health equity through
service enhancements, patient engagement activities, and adoption of best practices.
Toward that end, the Office of the Assistant Secretary for Planning and Evaluation
(ASPE) asked the RAND Corporation to identify existing health equity measurement
approaches that may be suitable for inclusion in Medicare’s VBP programs, quality
reporting efforts, and confidential reports. This project had two objectives: (1) identify
health equity measurement approaches, and (2) decide which of these approaches
merit consideration for inclusion in Medicare’s VBP programs, quality reporting efforts,
and confidential reports. To meet these objectives, the project team conducted a
literature review to identify health equity measurement approaches developed or used
for the purpose of systematic performance assessment and convened a technical expert
panel (TEP) to consider the use of these health equity measurement approaches in VBP
programs, quality reporting efforts, and confidential reports. The project team
synthesized feedback from the TEP to identify the most promising health equity
measurement approaches and inform the U.S. Department of Health and Human
Services (HHS) about which approaches could be incorporated in Medicare’s VBP
programs, quality reporting efforts, and confidential reports.
A formal definition of a health equity measurement approach was developed to
define the scope of the literature search and help specify the TEP’s evaluation of the
identified approaches. The definition, which was first developed iteratively by RAND
and ASPE and then further shaped by the TEP, is as follows: an approach to illustrating
or summarizing the extent to which the quality of health care provided by an
organization contributes to reducing disparities in health and health care at the
8
Though many people use the term social risk factor to refer to mechanisms that foster inequities in
health or health care—e.g., food insecurity or language barriers—we use the term here to refer to groups
that tend to bear a disproportionate share of social risk factor burden, e.g., racial and ethnic minorities. In
that sense, we are conceptualizing group membership as a proxy for social risk factors. By using the term
social risk factor to refer to membership in certain groups, we do not mean to imply that risk or
disadvantage is inherent in people, homogeneous within groupings (e.g., a particular race) or across
geography, or immutable over time. Rather, it is the result of past and present inequities in our society.
9
National Academies of Science, Engineering, and Medicine, Accounting for Social Risk Factors in Medicare
Payment: Identifying Social Risk Factors, Washington, D.C.: National Academies Press, 2016; United States
Department of Health and Human Services, “Healthy People 2020: Social Determinants of Health,”
webpage, 2014. As of May 11, 2020: https://www.healthypeople.gov/2020/topics-
objectives/topic/social-determinants-of-health
xv
population level for those patients with greater social risk factor burden by improving
the care and health of those patients.
Ten such approaches were identified. These ten approaches fit within three broad
categories of approaches: (1) approaches focused on determining which existing
quality measures are suitable for health equity comparisons (i.e., permit reliable and
valid comparisons among social risk factor groups) or for measuring organizational
structures, systems, and processes hypothesized to promote the delivery of high-quality
care for all; (2) approaches that engaged in particular kinds of comparisons of measures
(not necessarily statistical comparisons), on a measure-by-measure basis, between
groups of patients with greater versus lesser social risk factor burden; and (3)
approaches that developed a system for combining different dimensions of health
equity into a single summary index. Table S.1 lists these ten approaches and provides
summary information about them, including whether the approach focused on measure
identification (Category 1), measure-by-measure comparisons (Category 2), or creating
a summary index (Category 3).
This project also identified a set of guidelines for health equity measurement. A
health equity measurement approach should, ideally,
• be based on measures on which disparities in care are known to exist for certain
populations or that address health care disparities and culturally appropriate
care
• reflect available evidence on the relationship between a social risk factor and
health or health care outcome
• be designed to incentivize achievement or improvement for at-risk beneficiaries,
including having a valid and appropriate benchmark and/or reference group if
comparisons to benchmarks and/or reference groups are made
• include design features that guard against unintended consequences of
worsening quality or access or disincentivizing resources for any beneficiaries,
including the at-risk beneficiaries who are the focus of health equity
measurement
• establish measurability requirements that ensure the ability to make reliable
distinctions between health care providers in their performance in the domain of
health equity
• capture information about small subgroups where possible while limiting the
influence of imprecise estimates of provider performance.
In the case of a summary index, the measure should additionally
• summarize information in a way that is psychometrically sound
• allow for disaggregation of information to permit easy identification of quality
improvement targets.
Two of the identified approaches—the Measurement Framework for Evaluating
Organizational Compliance with Standards for National Culturally and Linguistically
Appropriate Services (CLAS) and the National Quality Forum’s (NQF) Disparities-
Sensitive Measure Assessment—determined whether existing quality measures were
suitable for health equity comparisons or for measuring organizational structures,
systems, and processes hypothesized to promote delivery of high-quality care for all
(Category 1).
Two approaches—the Agency for Healthcare Research and Quality’s (AHRQ) National
Healthcare Quality and Disparities Report and the Mapping Medicare Disparities (MMD)

xvi
Tool developed by the Centers for Medicare & Medicaid Services Office of Minority
Health (CMS OMH)—focused on performance comparisons by social risk-factor groups
either nationally or at a smaller geographical unit. Each of these two approaches
included a broad array of measures, treating each measure separately (the hallmark of
Category 2), though only the AHRQ approach involved statistical comparisons.
Two approaches—the CMS OMH stratified reporting of Medicare Advantage (MA),
prescription drug plan (PDP), and Medicare Fee-for-Service (FFS) performance data by
beneficiary race and ethnicity and the Minnesota Healthcare Disparities Report—
involved stratified reporting of data on patient experience and/or clinical care by social
risk factors with statistical comparisons to benchmarks. The CMS Office of Minority
Health’s approach involved reporting performance at the level of MA contracts, PDP
contracts, and states (for Medicare FFS), and the Minnesota Healthcare Disparities
Report involved reporting performance both statewide and at the level of individual
medical groups. Under these approaches, comparison of performance by contract, state,
or medical group was done on a measure-by-measure basis (Category 2).
The CMS Assessment of Hospital Disparities for Dual-Eligible Patients involved two
complementary methods for assessing hospital performance in the realm of health
equity. The Within-Hospital Disparity Method was used to measure the difference in a
health outcome between patients who are dually eligible for Medicare and Medicaid
(referred to as dual-eligible patients)
10
and patients who are not dually eligible within a
hospital. The Dual Eligible Outcome Method was used to compare performance for dual-
eligible patients across hospitals. In each case, the outcome measure of interest was 30-
day all-cause unplanned readmission following hospitalization for pneumonia. Because
this approach involved only one social risk factor and one outcome measure and the
two types of comparisons were kept separate, it fits within Category 2.
Two approaches were identified within Category 3. The CMS OMH’s Health Equity
Summary Score (HESS) approach identified patient experience and clinical care
measures specifically suitable for health equity comparisons and used data on those
measures to assess the extent to which care provided through MA contracts was
equitable based on race and ethnicity as well as dual/low-income subsidy (LIS)
eligibility status. The HESS combined data across multiple performance measures,
multiple social risk factors, and multiple types of comparisons, i.e., both within- and
between-provider comparisons and comparisons focused on both cross-sectional
performance and improvement in performance to create a summary index of health
equity (Category 3).
Zimmerman’s Health-Related Quality of Life Approach to Measuring Health Equity
synthesized information across multiple measures (Category 3). Zimmerman’s measure
is oriented toward assessing the total deviation from a defined privileged group and
allows disaggregation from the national level to the level of states and smaller
geographic areas. Zimmerman and Anderson developed a related approach that
generates trend information to characterize disparities in self-rated health and healthy
days in the past month as either decreasing, increasing, or not changing (this approach
involved both Category 2 and Category 3 assessments).
Of approaches focused on measure identification (Category 1), the NQF Disparities-
Sensitive Measure Assessment was viewed most favorably by the TEP. Using a set of
carefully established criteria and an easy-to-understand point system, this approach
10
The demonstration of this approach focused on full dual-eligible beneficiaries aged 65 and older.

xvii
identified 76 existing NQF-endorsed measures as disparities-sensitive.
11
Although
considerable work would be needed to determine whether and how these measures
could be linked to social risk data and whether and how valid comparisons could be
made, this approach was viewed as a valuable initial step toward measuring health
equity and disparities in health care quality. It is potentially applicable to any Medicare
VBP or quality reporting program that collects one or more of the disparities-sensitive
measures.
Of approaches focused on measure-by-measure comparisons (Category 2), the
approach underlying the Minnesota Healthcare Disparities Report was judged
most favorably by the TEP. The perceived advantages of this approach include its
thoughtfully chosen group of measures, incorporation of multiple important social risk
factors (i.e., race, ethnicity, preferred language, and country of origin), ability to reliably
distinguish performance among providers, clear focus on incentivizing achievement for
at-risk beneficiaries, and choice to anchor disparities to the overall state average rather
than the performance of a predetermined group. Although some additional work would
be needed to transfer this approach to a broader setting, including making careful
considerations about sample sizes required for accurate comparisons and determining
the availability of data on social risk factors, the method itself is readily applicable to all
Medicare VBP and quality reporting programs.
Of approaches focused on summary indices (Category 3), the CMS OMH HESS was
judged most favorably by the TEP. The perceived advantages of this approach include
its joint consideration of cross-sectional performance and improvement in
performance, focus on patient experience and clinical quality, careful attention to
reliability and the sample size required to achieve it, direct applicability to certain VBP
and quality reporting programs, and transferability to other programs. CMS is currently
developing a dashboard to provide confidential HESS data to MA contracts in the near
future. Scores on this metric could potentially be incorporated into the Medicare Plan
Finder and the MA Quality Star Ratings Program. This approach could easily be
extended to other social risk factors and measures, and there are plans to test the
feasibility of extending this approach to settings beyond MA.
Of the ten approaches evaluated, the HESS received the highest ratings from the TEP
overall. Given the high ratings it received, the HESS may be closest to meeting the full
scope of goals outlined by ASPE for incorporating a measure of health equity into a
Medicare VBP or quality reporting program. If HHS were to move forward with this
approach, it could consider possible refinements to the approach based on the practices
established by the NQF Disparities-Sensitive Measure Assessment and the Minnesota
Healthcare Disparities Report and the guidelines for health equity measurement
outlined by the TEP. Several of the measures that are included in the HESS are among
the 76 measures identified as disparities-sensitive by NQF. It might be possible to
include in the HESS additional measures from the set identified by NQF, provided that
the measures are collected for MA plans and meet the reliability and sample size
requirements established for the HESS. The analyses that underlie the Minnesota
Disparities Report are similar to the analyses that underlie the cross-sectional
component of the HESS. In the Minnesota Healthcare Disparities Report, plan
11
Disparities-sensitive measures were defined as measures of conditions that are prevalent among at-risk
groups, measures assessing a high-impact aspect of health care (i.e., conditions affecting large numbers of
people, leading causes of morbidity and mortality, conditions leading to high resource use, and severe
illnesses), measures on which a substantial disparity has been identified, and measures that map to an
NQF-endorsed communication-sensitive practice for care coordination or cultural competency.
xviii
performance by patients’ preferred language and country of origin are considered in
addition to race and ethnicity. Information on country of origin is not available for MA
beneficiaries, but information about Spanish preference is available. Thus, Spanish
preference could be considered as a possible third social risk factor for the HESS.

Table S.1. Ten Identified Approaches to Health Equity Measurement
Measurement Approach Setting/Population Social Risk Factor(s) Focus
1. Measurement Framework for Evaluating How Well an Health care organizations Race/ethnicity; limited English Measure identification
Organization Meets National Standards for Culturally proficiency; low literacy
and Linguistically Appropriate Services (HHS OMH)
2. NQF Disparities-Sensitive Measure Assessment Cross-cutting Race/ethnicity Measure identification
3. AHRQ National Healthcare Quality and Disparities Overall U.S. population Age; sex, race/ethnicity Measure-by-measure
Report comparisons
4. CMS OMH Mapping Medicare Disparities Tool Medicare FFS Race/ethnicity; dual eligibility; Measure-by-measure
sex; age comparisons
5. CMS OMH Reporting of CAHPS and HEDIS Data by MA and prescription drug Race/ethnicity Measure-by-measure
Race/Ethnicity for Medicare Beneficiaries plans, Medicare FFS comparisons
6. Minnesota Healthcare Disparities Report Minnesota health plan Race, ethnicity, preferred Measure-by-measure
enrollees language, country of origin comparisons
7. CMS Assessment of Hospital Disparities for Dual- Hospitals Dual eligibility Measure-by-measure
Eligible Patients comparisons
8. CMS OMH Health Equity Summary Score Medicare Advantage plans Race/ethnicity; dual eligibility Summary index
9. Zimmerman Health-Related Quality of Life Approach to General adult U.S. population Race/ethnicity; sex; income Summary index
Assessing Health Equity
10. Zimmerman and Anderson Approach to Evaluating General adult U.S. population Race/ethnicity; sex; income Measure-by-measure
Trends over Time in Health Equity comparisons; summary index
NOTE: CAHPS = Consumer Assessment of Healthcare Providers and Systems; CMS = Centers for Medicare & Medicaid Services; HHS = U.S. Department of
Health and Human Services; FFS = fee-for-service; HEDIS = Healthcare Effectiveness Data and Information Set; MA = Medicare Advantage; NQF = National
Quality Forum; OMH = Office of Minority Health.
xix

1
1. Background and Purpose
Background
There is growing recognition that social risk factors
12
—such as income, education, race and
ethnicity, and community resources—play a major role in health.
13
Despite ongoing efforts
to address inequities, evidence suggests that socially at-risk individuals receive lower-
quality health care and experience worse health outcomes than more-advantaged
individuals.
14
Medicare’s value-based purchasing (VBP) programs, which link reimbursement to the
quality and efficiency of health care delivered, could be a powerful tool to drive
improvements in the quality of care provided to patients with social risk factors, which
could potentially improve health outcomes among patients with social risk factors and
reduce health disparities. Medicare’s VBP programs include pay-for-performance programs
in each health care setting that reward providers on quality and cost, as well as Alternative
Payment Models, such as Accountable Care Organizations, or state population–based
models in which providers are at financial risk for lowering costs and improving quality of
care. The scope of this report is focused mainly on pay-for-performance programs. Quality
reporting efforts and confidential reports to providers may have similar incentivizing
effects. The National Academy of Medicine identified the following social risk factors as
likely to be important to health outcomes for Medicare beneficiaries: socioeconomic
position; race, ethnicity, and cultural context; gender; social relationships; and residential
and community context.
15
Including health equity measurement approaches in VBP and
quality reporting programs could motivate a focus on reducing disparities and help
providers prioritize particular areas for quality improvement activities. It could also
encourage providers to address health equity through service enhancements, patient
12
Though many people use the term social risk factor to refer to mechanisms that foster inequities in health
or health care—e.g., food insecurity or language barriers—we use the term here to refer to groups that tend
to bear a disproportionate share of social risk factor burden, e.g., racial and ethnic minorities. In that sense,
we are conceptualizing group membership as a proxy for social risk factors. By using the term social risk
factor to refer to membership in certain groups, we do not mean to imply that risk or disadvantage is inherent
in people, homogeneous within groupings (e.g., a particular race) or across geography, or immutable over
time. Rather, it is the result of past and present inequities in our society.
13
National Academies of Science, Engineering, and Medicine, Accounting for Social Risk Factors in Medicare
Payment: Identifying Social Risk Factors, Washington, D.C.: The National Academies Press, 2016; U.S.
Department of Health and Human Services (HHS), “Healthy People 2020: Social Determinants of Health,”
webpage, 2014. As of May 11, 2020: https://www.healthypeople.gov/2020/topics-objectives/topic/social-
determinants-of-health
14
Institute of Medicine, How Far Have We Come in Reducing Health Disparities? Progress Since 2000:
Workshop Summary, Washington, D.C.: National Academies Press. 2012.
15
Assistant Secretary for Planning and Evaluation, Social Risk Factors and Performance Under Medicare’s
Value-Based Purchasing Programs, Washington, D.C.: HHS, 2016; National Academies of Science, Engineering,
and Medicine, Accounting for Social Risk Factors in Medicare Payment: Identifying Social Risk Factors,
Washington, D.C.: National Academies Press, 2016.

2
engagement activities, and adoption of best practices to improve performance in the health
equity domain. The use of health equity measurement approaches as part of VBP and
quality reporting sends a strong signal that health equity is an important component of
delivery system transformation.
However, if beneficiaries with social risk factors have worse outcomes because of elements
beyond the control of health care providers, the inclusion of health equity measurement
approaches in VBP and quality reporting programs could make providers reluctant to care
for beneficiaries with social risk factors, out of fear of incurring penalties, not achieving
bonuses, or having their reputations damaged due to factors they have limited ability to
influence.
In 2014, under the Improving Medicare Post-Acute Care Act, Congress asked that the
Assistant Secretary for Planning and Evaluation (ASPE) study the relationship between
social risk factors and Medicare’s VBP programs. ASPE wrote two Reports to Congress
(referred to as Study A and Study B), making recommendations based on the study’s
findings. These reports outline multiple strategies for accounting for social risk factors in
Medicare’s VBP programs.
17
Although the reports recommend including health equity
measures in Medicare’s VBP programs, they do so cautiously, outlining several
considerations that need to be addressed first. For example, the reports stress that the
design of any such measurement approach needs to be informed by careful consideration
of the linkage between social risk factors and the outcome or outcomes measured. They
also highlight the need to consider whether score adjustments are needed to account for
factors outside the control of providers. Steps such as these ensure that health equity
measurement approaches can be used in VBP programs to incentivize improvements for
beneficiaries with social risk factors while guarding against any real or perceived
disincentives to care for these beneficiaries.
16
Project Objectives
ASPE asked the RAND Corporation to identify existing health equity measurement
approaches that may be suitable for inclusion in Medicare’s VBP programs, quality
rep
orting efforts, and confidential reports. This project had two objectives:
1. Identify and describe health equity measurement approaches.
2. Decide which of these merit consideration for inclusion in Medicare’s VBP
programs, quality reporting efforts, and confidential reports.
In August 2020, the project team conducted a literature review to identify health equity
measurement approaches developed or used for the purpose of systematic performance
assessment. In September 2020, the project team convened a technical expert panel (TEP)
with experts on social risk factors, health disparities, health equity, quality measurement,
and Medicare’s VBP programs and quality reporting efforts to consider the use of these
16
113
th
Congress of the United States, “H.R.4994 - IMPACT Act of 2014,” webpage, 2014. As of January 11,
2021: https://www.congress.gov/bill/113th-congress/house-bill/4994
17
ASPE, Social Risk Factors and Performance Under Medicare’s Value-Based Purchasing Programs, Washington,
D.C.: HHS, 2016; ASPE, Social Risk Factors and Performance Under Medicare’s Value-Based Purchasing
Programs, Washington, D.C.: HHS, 2020.
3
health equity measurement approaches in VBP programs, quality reporting efforts, and
confidential reports.
The objectives of the TEP were to (1) provide feedback on the project team’s proposed
definition of a health equity measure and identification of features of health equity
measurement approaches; (2) reach consensus on a set of criteria for evaluating health
equity measurement approaches for potential inclusion in Medicare’s VBP programs,
quality reporting efforts, and confidential reports; and (3) evaluate the set of health equity
measurement approaches identified by the team according to these criteria.
The project team synthesized feedback from the TEP to identify the most promising health
equity measurement approaches in development and inform potential next steps toward
incorporating health equity measures and domains in Medicare’s VBP programs, quality
reporting efforts, and confidential reports.
The rest of this report is organized as follows. Chapter 2 describes the literature review
methods and results. Chapter 3 provides detailed information on each of the identified
health equity measurement approaches, and Chapter 4 provides an integrative summary of
these approaches. Chapter 5 provides information about how the TEP was convened and
conducted. Chapter 6 describes the input provided by the TEP on the project framing and
approach. Chapter 7 describes TEP members’ assessment of and commentary on each of
the identified health equity measurement approaches. Chapter 8 provides a summary of
the findings of this project and key takeaways for the U.S. Department of Health and Human
Services (HHS).

4
2. Literature Review Methods and Results
The project team conducted a review of articles and reports on health equity measurement
approaches developed or intended for use in systematic performance assessment.
Definition of a Health Equity Measurement Approach to Assess
Organizational Contributions
We developed a formal definition of a health equity measure to guide our search. The
definition, which emphasizes performance assessment, is as follows: an approach to
illustrating or summarizing the extent to which the quality of health care provided by an
organization contributes to reducing disparities in health and health care at the population
level for those patients with greater social risk factor burden by improving the care and
health of those patients.
18
Though such an approach is not centered on performance
assessment per se, we agreed that an approach focused on structural measures—measures
of the extent to which structures, systems, or processes hypothesized to promote the
delivery of equitable care are in place within a health care organization—was in scope,
given that such measures capture potentially important mechanisms for aligning care and
resources with physical, mental, and social needs to optimize health outcomes for all.
Search Strategy
Our search strategy included three approaches. First, we used a structured database search
on Ovid MEDLINE and Cumulative Index to Nursing and Allied Health Literature (CINAHL)
to identify English-language, peer-reviewed articles published from January 2010 to
August 2020. We identified articles using Medical Subject Headings (MeSH) and keywords
with at least (1) one health equity or social risk keyword and (2) one performance
measurement keyword. Table 2.1 lists the search terms by category. Second, we used a
purposive “snowball” approach to identify potentially relevant documents by reference-
mining seminal reports (see List 2.1). These are reports that were identified or suggested
by health equity measurement experts within the project team and at ASPE. Third, we
conducted a gray literature search to identify relevant documents from websites of federal
agencies (Centers for Medicare & Medicaid Services [CMS] and ASPE), the National
Academy of Medicine, the National Quality Forum (NQF) Quality Positioning System, and
the National Quality Measures Clearinghouse. After removing duplicates, our search
yielded 783 records, including both published peer-reviewed journal articles and gray
literature reports (Figure 2.1).
18
The National Academy of Medicine (2016) identified five social risk factors that are conceptually likely to
be of importance to health outcomes of Medicare beneficiaries: socioeconomic position; race, ethnicity, and
cultural context; gender; social relationships; and residential and community context.
5
Eligibility Criteria
Because our aim was to identify health equity measurement approaches, we sought to
exclude articles and reports if they (1) did not describe a specific health equity
measurement approach developed or used for the purpose of systematic performance
assessment; or (2) were focused on risk adjustment. These exclusions were applied during
the article/report screening process described next.
Article/Report Screening
Figure 2.1 illustrates the article/report screening process. We first reviewed titles and
abstracts of the 783 documents we identified. To ensure consistent application of our
eligibility criteria, three reviewers first independently coded 60 articles across three
separate rounds (i.e., 20 articles in each round). Between rounds, reviewers met to discuss
independent review outcomes and discrepancies and their application of the criteria, as
well as to further refine the definition of each criterion. Disagreements were resolved
through discussion or by involving the principal investigator until consensus was reached.
Subsequent titles/abstracts were divided, and each was reviewed by one of the three
reviewers. Any uncertainties were discussed by the project team together, and all abstracts
marked for inclusion were also reviewed by the project team before proceeding to full-text
review. We excluded 647 documents at the title/abstract stage that did not meet eligibility
criteria.
We then undertook a full text review of 136 documents to identify measurement
approaches that would allow health plans or providers to identify areas in which they are
performing well or poorly at providing high-quality care to patients with greater social risk
factor burden.
Upon full text review, we applied additional exclusions, with the aim of excluding
documents that did not articulate a specific health equity measurement approach.
Specifically, we excluded (a) documents that described theoretical approaches or
frameworks to health equity measurement not currently in development or in use; (b)
documents that proposed adjustments to scores or adjustments to payment allocations
within an incentive scheme; (c) documents that simply detailed the existence of disparities
without the use of a specific measure of disparity; and (d) documents that described the
effect of an incentive scheme on disparities. At this stage, we excluded an additional 114
documents that did not meet the eligibility criteria.
Of the 22 documents that met our eligibility criteria, eight fit the fifth category of
measurement approaches described above (i.e., measures of the extent to which structures,
systems, or processes hypothesized to promote the delivery of equitable care are in place
within a health care organization). Because these eight documents all described similar
approaches, we opted to include only the most comprehensive of them in our final results.
The document that was kept describes a measurement framework for evaluating how well
health care organizations comply with national standards for providing culturally and

6
linguistically appropriate services. This document was authored by Davis et al.
19
and
describes the results of research commissioned by HHS’s Office of Minority Health (HHS
OMH). The seven documents that we did not include in our final results are in List 2.2.
Similarly, four of the 22 documents that met our eligibility criteria were reports of national
disparities on patient experience, clinical process and outcome, and patient safety
measures. Because these four reports all describe similar approaches to the analysis of
disparities, we opted to include just one in our final results. The report that was included is
the Agency for Healthcare Research and Quality (AHRQ) National Healthcare Quality and
Disparities Report.
20
The three documents that we did not include in our final results are
also in List 2.2. Thus, a total of 11 articles/reports were selected for inclusion in our final
results. One of the 11 articles/reports selected for inclusion
21
describes the analytic
foundation underlying another of the reports.
22
Thus, although 11 articles/reports were
identified, they pertain to only ten total approaches (see Table 2.4 for a summary).
In the following chapters, we describe in detail the ten approaches to health equity
measurement described in each of these 11 articles/reports. The description includes
information about the approach, the setting and population in which the approach was
initially evaluated (if applicable), the social risk factors encompassed by the approach, the
outcome measures that factor into the approach, and any available psychometric
information reported in the article/report. The description also indicates the features of
the approach (see Features of Health Equity Measurement Approaches above) and whether
the approach has been endorsed by a measure endorsement body or is currently in use in a
Medicare VBP or quality reporting program.
19
L. M. Davis, L. T. Martin, A. Fremont, R. Weech-Maldonado, M. V. Williams, and A. Kim, Development of a
Long-Term Evaluation Framework for the National Standards for Culturally and Linguistically Appropriate
Services (CLAS) in Health and Health Care, Santa Monica, Calif.: RAND Corporation, EP-68215, 2018.
20
AHRQ, 2018 National Healthcare Quality and Disparities Report, Rockville, Md., 2019. As of January 4, 2021:
https://www.ahrq.gov/research/findings/nhqrdr/nhqdr18/index.html
21
S. C. Martino, R. M. Weinick, D. E. Kanouse, J. A. Brown, A. M. Haviland, E. Goldstein, J. L. Adams, K.
Hambarsoomian, D. J. Klein, and M. N. Elliott, “Reporting CAHPS and HEDIS Data by Race/Ethnicity for
Medicare Beneficiaries,” Health Services Research Vol. 48, No. 2 Pt 1, 2013, pp. 417–434.
22
OMH, “Part C and D Performance Data Stratified by Race, Ethnicity, and Gender,” database, Centers for
Medicare and Medicaid Services, 2020. As of January 4, 2020: https://www.cms.gov/About-CMS/Agency-
Information/OMH/research-and-data/statistics-and-data/stratified-reporting.html

7
Table 2.1. Database Search Strategy
Concept MeSH Search Terms
Health equity Health equity; healthcare disparities Equity; disparit*
Social risk Social determinants of health;
socioeconomic factors; safety-net
providers
Social determinants; social risk;
safety net; race; ethnicity
Performance measurement Value-based purchasing; incentive
reimbursement
Performance measure; quality
measure; value-based purchasing;
pay for performance; quality
reporting; public reporting; CAHPS;
HEDIS
NOTE: The search syntax was as follows:
1. "health equity".sh,kf.
2. "healthcare disparities".sh.
3. "equity".ti,ab.
4. "disparit*".ti,ab.
5. "social determinants of health".sh.
6. "social determinants".ti,ab.
7. "social risk".ti,ab.
8. "socioeconomic factors".sh.
9. "safety-net providers".sh.
10. "safety net".ti,ab.
11. "race".ti,ab.
12. "ethnicity".ti,ab.
13. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12
14. "value-based purchasing".ti,ab,sh.
15. "reimbursement, incentive".sh.
16. "performance measure".ti,ab,kf.
17. "quality measure".ti,ab,kf.
18. "pay for performance".ti,ab.
19. "quality reporting".ti,ab.
20. "public reporting".ti,ab.
21. "CAHPS".ti,ab.
22. "HEDIS".ti,ab.
23. 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22
24. 13 and 23
25. limit 24 to English language
26. limit 25 to yr="2010-Current"

8
List 2.1. Seminal Reports Mined as Part of Our Purposive Snowball Approach
Anderson, A. C., E. O’Rourke, M. H. Chin, N. A. Ponce, S. M. Bernheim, and H. Burstin, “Promoting Health
Equity and Eliminating Disparities Through Performance Measurement and Payment,” Health Affairs, Vol. 37,
No. 3, 2018, pp. 371–377.
ASPE Report to Congress: Social Risk Factors and Performance Under Medicare’s Value-Based Purchasing
Programs (Study A), 2016.
ASPE Report to Congress: Social Risk Factors and Performance Under Medicare’s Value-Based Purchasing
Programs (Study B), 2020.
Damberg, C. L., M. N. Elliott, and B. A. Ewing, “Pay-for-Performance Schemes That Use Patient and Provider
Categories Would Reduce Payment Disparities,” Health Affairs, Vol. 34, No. 1, 2015, pp. 134–142.
Hughes, D., J. Levi, J. Heinrich, and H. Mittmann, Developing a Framework to Measure the Health Equity
Impact of Accountable Communities for Health, Washington, D.C.: Funders Forum on Accountable Health,
2020.
National Academies of Science, Engineering, and Medicine, Accounting for Social Risk Factors in Medicare
Payment: Identifying Social Risk Factors, Washington, D.C.: National Academies Press and HHS, 2016.

9
List 2.2. Articles and Reports That Met Eligibility Criteria but Were Not Included in the Final
Results
Articles and reports describing measures of structures, systems, and processes within a health care
organization that promote delivery of equitable care
• Hughes, D., J. Levi, J. Heinrich, and H. Mittmann, Developing a Framework to Measure the Health Equity
Impact of Accountable Communities for Health, Washington, D.C.: Funders Forum on Accountable Health,
2020.
• Cultural Competency 2010 Measures and Implementation Strategies, Washington, D.C.: NQF, 2011.
• Healthcare Disparities and Cultural Competency Consensus Standards Technical Report, Washington
D.C.: NQF, 2012.
• Ng, J. H., M. A. Tirodkar, J. B. French, H. E. Spalt, L. M. Ward, S. C. Haffer, N. Hewitt, D. Rey, and S. H.
Scholle, “Health Quality Measures Addressing Disparities in Culturally and Linguistically Appropriate
Services: What are Current Gaps?” Journal of Health Care for the Poor and Underserved, Vol. 28, No. 3,
2017, pp. 1012–1029.
• Weech-Maldonado, R., A. Carle, B. Weidmer, M. Hurtado, Q. Ngo-Metzger, and R. D. Hays, “The
Consumer Assessment of Healthcare Providers and Systems (CAHPS) Cultural Competence (CC) Item
Set,” Medical Care, Vol. 50, No. 9, Suppl 2, 2012, pp. S22–S31.
• Weech-Maldonado, R., J. Dreachslin, J. Brown, R. Pradhan, K. L. Rubin, C. Schiller, and R. D. Hays,
“Cultural Competency Assessment Tool for Hospitals (CCATH): Evaluating Hospitals' Adherence to the
CLAS Standards,” Health Care Management Review, Vol. 37, No. 1, 2012, pp. 54–66.
• Weech-Maldonado, R., M. N. Elliott, J. L. Adams, A. M. Haviland, D. J. Klein, K. Hambarsoomian, C.
Edwards, J. W. Dembosky, and S. Gaillot, “Do Racial/Ethnic Disparities in Quality and Patient Experience
Within Medicare Plans Generalize Across Measures and Racial/Ethnic Groups?” Health Services
Research, Vol. 50, No. 6, 2015, pp. 1829–1849.
• Weech-Maldonado, R., M. Elliott, et al. “Can Hospital Cultural Competency Reduce Disparities in Patient
Experiences with Care?” Medical Care, Vol. 50, 2012, pp. S48–S55.
Reports of national disparities in health care
• The National Impact Assessment of CMS Quality Measures Reports, Baltimore, Md.: CMS, February
2020.
• Martino, S. C., M. N. Elliott, J. W. Dembosky, K. Hambarsoomian, Q. Burkhart, D. J. Klein, J. Gildner, and
A. M. Haviland, Racial, Ethnic, and Gender Disparities in Health Care in Medicare Advantage, Baltimore,
Md: CMS OMH, 2020.
• Martino, S. C., M. N. Elliott, J. W. Dembosky, K. Hambarsoomian, Q. Burkhart, D. J. Klein, J. Gildner, and
A. M. Haviland, Rural-Urban Disparities in Health Care in Medicare, Baltimore, Md.: CMS OMH, 2019.

10
Figure 2.1. Literature Review Flow Diagram
Records identified in
MEDLINE/CINAHL
(n = 675)
Records identified through other
sources
(n = 128)
Records after duplicates removed
(n = 783)
Records screened
(n = 783)
Records excluded
(n = 647)
Full-text articles/reports
assessed for eligibility
(n = 136)
Full-text articles/reports
excluded
(n = 125)
Articles/reports included in
synthesis
(n = 11)
Records identified in
MEDLINE/CINAHL
(n = 675)
Records identified through other
sources
(n = 128)
Records after duplicates removed
(n = 783)
Records screened
(n = 783)
Records excluded
(n = 647)
Full-text articles/reports
assessed for eligibility
(n = 136)
Full-text articles/reports
excluded
(n = 125)
Articles/reports included in
synthesis
(n = 11)
Identification
Screening
Eligibility
Included

11
Table 2.2. Summary of the Health Equity Measurement Approaches Identified by the Literature Review
Measurement Approach Setting/Population Social Risk Factor(s)
1. Measurement Framework for Evaluating How Well an Organization Meets
National Standards for Culturally and Linguistically Appropriate Services
(HHS OMH)
Health care organizations Race/ethnicity; limited English
proficiency; low literacy
2. NQF Disparities-Sensitive Measure Assessment Cross-cutting Race/ethnicity
3. AHRQ National Healthcare Quality and Disparities Report Overall U.S. population Age; sex, race/ethnicity
4. CMS OMH Mapping Medicare Disparities Tool Medicare FFS Race/ethnicity; dual eligibility; sex; age
5. CMS OMH Reporting of CAHPS and HEDIS Data by Race/Ethnicity for
Medicare Beneficiaries
MA and prescription drug plans,
Medicare FFS
Race/ethnicity
6. Minnesota Healthcare Disparities Report Minnesota health plan enrollees Race, ethnicity, preferred language,
country of origin
7. CMS Assessment of Hospital Disparities for Dual-Eligible Patients Hospitals Dual eligibility
8. CMS OMH Health Equity Summary Score Medicare Advantage plans Race/ethnicity; dual eligibility
9. Zimmerman Health-Related Quality of Life Approach to Assessing Health
Equity
General adult U.S. population Race/ethnicity; sex; income
10. Zimmerman and Anderson Approach to Evaluating Trends over Time in
Health Equity
General adult U.S. population Race/ethnicity; sex; income
NOTE: CAHPS = Consumer Assessment of Healthcare Providers and Systems; CMS = Centers for Medicare & Medicaid Services; DHHS = U.S. Department of
Health and Human Services; FFS = fee-for-service; HEDIS = Healthcare Effectiveness Data and Information Set; MA = Medicare Advantage; NQF = National
Quality Forum; OMH = Office of Minority Health.

12
3. Detailed Information on Identified Approaches
In this chapter, we describe in detail the health equity measurement approaches that were
identified by the literature described in the preceding chapter. A summary of these
measurement approaches appears in the following chapter, which also introduces a
categorization scheme by which the measurement approaches are ordered here and
elsewhere.
Measurement Framework for Evaluating How Well an Organization Meets
National CLAS Standards (HHS OMH)
Overview. This report—which was commissioned by HHS OMH— describes a framework
for measuring whether structures, systems, or processes hypothesized to promote health
equity are in place within a health care organization or system.
23
Background. The National CLAS Standards are a set of 15 standards intended to advance
health equity and help eliminate health care disparities by providing a blueprint for health
care organizations to implement culturally and linguistically appropriate services. The
essential goal of the standards is framed in the Principal Standard: Provide effective,
equitable, understandable, and respectful quality care and services that are responsive to
diverse cultural health beliefs and practices, preferred languages, health literacy, and other
communication needs. The other 14 standards address domains of governance, leadership,
and workforce; communication and language assistance; and engagement, continuous
improvement, and accountability.
Design and methods. The goal of this approach is to identify a set of well-constructed and
validated health equity process and impact measures that could be applied to four settings
of care—ambulatory care, hospitals, behavioral health, and public health—to evaluate how
well a health care organization meets the National CLAS Standards. Specific criteria were
used by the authors of this framework to identify salient measures to consider, including
whether the measure (a) assesses cultural competency; (b) captures language needs or
preferences and/or is linked to other CLAS-related issues; (c) documents disparities; (d) is
validated and/or psychometrically tested; (e) is widely used or suitable for use by a range
of health care organizations; (f) has been previously endorsed in commissioned projects or
reports for evaluating disparities; and (g) cuts across conditions and/or settings. Measures
were categorized as cross-cutting (i.e., applicable across multiple settings) or setting-
specific. Based on the criteria, the authors identified six cross-cutting measures (see Table
3.1), six ambulatory-specific measures, nine hospital-specific measures, five behavioral
health–specific measures, and six public health–specific measures. Appendix A shows
measures that fit the latter four categories.
23
L. M. Davis, L. T. Martin, A. Fremont, R. Weech-Maldonado, M. V. Williams, and A. Kim, Development of a
Long-Term Evaluation Framework for the National Standards for Culturally and Linguistically Appropriate
Services (CLAS) in Health and Health Care, Santa Monica, Calif.: RAND Corporation, EP-68215, 2018.

13
Table 3.1. Cross-Cutting Measures to Evaluate How Well an Organization Meets National CLAS
Standards
Measure Description
Clinician/group’s cultural
competence based on the CAHPS
Cultural Competence Item Set
Domains from CAHPS Cultural Competence Item Set: patient-provider
communication; complementary and alternative medicine; experiences of
discrimination due to race/ethnicity, insurance, or language; experiences leading
to trust or distrust, including level of trust, caring, and confidence in the
truthfulness of a provider; and linguistic competency (access to language
services)
Clinician/group’s health literacy
practices based on the CAHPS
Item Set for Addressing Health
Literacy
Domains from CAHPS Item Set for Addressing Health Literacy: communication
with provider, disease self-management, communication about medicines,
communication about test results, and communication about forms.
Patients receiving language
services supported by qualified
language services providers
Percentage of patients with limited English proficiency receiving both initial
assessment and discharge instructions supported by assessed and trained
interpreters or from bilingual providers and bilingual workers/employees assessed
for language proficiency
Screening for preferred spoken
language for health care
Percentage of patient visits and admissions in which the preferred spoken
language for health care is screened and recorded.
Cultural Competency
Implementation Measure
Survey of degree to which health care organizations are providing culturally
competent care and addressing the needs of diverse populations, as well as their
adherence to 12 of the 45 NQF-endorsed cultural competency practices.
Communication Climate
Assessment Toolkit
360-degree organizational assessment using coordinated patient, staff, and
leadership surveys, as well as an organizational workbook that collects important
information on the organization’s policies and practices.

14
NQF Disparities-Sensitive Measure Assessment
Overview. This report presents a protocol to systematically screen and identify NQF-
endorsed measures as disparities-sensitive.
24
The set of measures identified by this
approach was developed for use across health care settings.
Background. To establish a platform for addressing health care disparities and cultural
competency in measurement, NQF sought to identify measures from within its existing
portfolio of endorsed measures that might be disparities-sensitive (see below). In
particular, NQF sought to identify measures sensitive to health care disparities and cultural
competency for racial and ethnic minority populations. They established criteria to
evaluate measures for how sensitive they were to disparities, assigned points to each
measure based on these criteria, and set point thresholds and other rules to identify
disparities-sensitive measures.
Design and methods. To evaluate existing measures for disparities sensitivity, two tiers of
criteria were established that placed emphasis on prevalence and impact of the condition,
quality gap, and impact of the quality process.
25
The first-tier criteria—applied to
condition-specific measures and measures of health care access and quality—included the
prevalence of the condition among minority groups, the size of the gap in the quality of care
between disadvantaged and advantaged groups, and the impact the condition has
financially or societally. The second-tier criteria—applied to process measures that could
be used to improve performance in health equity—included communication-sensitive
practices; specifically, whether the measure mapped to either the NQF-endorsed
competency framework domain or the care coordination framework domain.
Based on these criteria, a simple scoring system was applied to evaluate over 500 measures
in the existing NQF portfolio. For condition-specific measures, 3 points were given for
specific conditions such as cancer, diabetes, and heart disease and 2 points for measures on
a list of top 20 conditions among Medicare beneficiaries, such as substance abuse or
obesity. Cross-cutting areas, such as patient safety, functional status, or pain management,
were given 3 points. All other condition-specific measures were given 1 point. Similarly, the
greater the size of the quality gap between disadvantaged and advantaged groups, the
more points were assigned; e.g., a 0-percent to 2-percent quality gap was assigned 1 point,
while a quality gap greater than 14 percent was given 4 points. To reflect impact, 1 point
was assigned for each National Quality Strategy priority area or goal addressed, and 1 point
each for whether a condition was a leading cause of morbidity/mortality overall, was
associated with high resource use, had high severity of illness, or was one for which poor
24
Healthcare Disparities and Cultural Competency Consensus Standards: Disparities Sensitive Measure
Assessment, NQF Technical Report, Washington, D.C., 2012. As of January 4, 2021:
https://www.qualityforum.org/Publications/2012/11/Healthcare_Disparities_and_Cultural_Competency_Co
nsensus_Standards__Disparities-Sensitive_Measure_Assessment.aspx. Also see NQF, A Roadmap for Promoting
Health Equity and Eliminating Disparities: The Four I’s for Health Equity, Washington, D.C., 2017. As of January
4, 2021:
http://www.qualityforum.org/Publications/2017/09/A_Roadmap_for_Promoting_Health_Equity_and_Elimin
ating_Disparities__The_Four_I_s_for_Health_Equity.aspx
25
Measures addressing the National Quality Strategy priority areas or goals were judged to fit this criterion,
as were measures assessing a high-impact aspect of health care (e.g., conditions affecting large numbers,
leading causes of morbidity and mortality, conditions leading to high resource use, and severe illnesses).

quality would be consequential. Finally, 2 points were given to any measures that mapped
to the two NQF-endorsed framework domains.
To select measures, NQF emphasized prevalence, the threshold of the quality gap, impact,
and whether a measure could be mapped to an NQF-endorsed framework domain
addressing care coordination or cultural competency (Figure 3.1). If the measure scored 9
or higher on the first-tier criteria, the measure was considered disparities-sensitive.
Further, if the quality gap was 14 percent or higher, the measure was also automatically
considered disparities-sensitive. The NQF analysis found that measures that fit within the
highest quality-gap quartile also had the highest first-tier score, which identified an initial
set of 62 measures deemed disparities-sensitive. Additional analysis of whether a measure
mapped to an NQF-endorsed framework domain identified another 14 measures, for a total
of 76 disparities-sensitive measures. These measures are listed in Appendix B.
Figure 3.1. NQF Disparities-Sensitive Measure Identification
15

16
AHRQ National Healthcare Quality and Disparities Report
Overview. This report describes approaches to measuring and reporting providers’
performance for patients with social risk factors versus without them, and also measures
health disparities specifically using methods for formally comparing performance between
patients with social risk factors versus without them.
26
The approaches are applied to the
overall U.S. population. Data come from a large number of national surveys and databases
maintained by several federal agencies, including AHRQ, CMS, the Centers for Disease
Control and Prevention, the Indian Health Service, the National Institutes of Health, the
Substance Abuse and Mental Health Services Administration, and the Health Resources and
Services Administration.
27
Background. The AHRQ National Healthcare Quality and Disparities Report is an annual
report mandated by Congress to provide a comprehensive overview of the quality of health
care received by the general U.S. population and disparities in care experienced by
different racial and socioeconomic groups. It includes information on disparities in access
to care and quality of care in the most recent data year, as well as changes in disparities
over time. The report also includes information on federal initiatives to reduce disparities.
The social risk factors addressed include age, sex, and race and ethnicity. In this report,
comparisons are made between a reference group
28
and a priority population group based
on a population characteristic, such as sex (i.e., women versus men) or minority racial and
ethnic groups versus Whites. The report includes more than 250 structure, process, and
outcome measures covering a broad array of health care services and settings. For
example, the report provides data on access to health care, patient experience, patient
safety, maternal and child health, functional status preservation and rehabilitation,
supportive and palliative care, health promotion, clinical preventive services, use of
effective treatments, care coordination, care affordability, morbidity, and mortality.
Design and methods. All measures are scored as percentages. Two criteria are applied to
identify meaningful differences in measure performance between two groups in the single
current, or most recent, data year. First, the absolute difference in measure performance
between the priority population group and the reference group must be statistically
significant with p < 0.05 on a two-tailed test. Second, the relative difference between the
two groups must be at least 10 percent when framed positively or negatively (i.e., in either
direction). For example, performance on the measure could be 10 percent higher in the
reference group than the priority group, and that would be characterized as a meaningful
difference, or disparity.
To evaluate changes in disparities over time, the average annual change (AAC) in measure
performance for each group is first calculated as the coefficient in an unweighted
regression analysis that estimates performance in at least four time points between 2000
and the most recent data year for both the priority and the reference groups. Then, the AAC
26
AHRQ, 2018 National Healthcare Quality and Disparities Report, Rockville, Md., 2019. As of January 4, 2021:
https://www.ahrq.gov/research/findings/nhqrdr/nhqdr18/index.html
27
More information about data sources can be found in the 2018 National Healthcare Quality and Disparities
Report Data Sources, Rockville, Md.: AHRQ, October 2019. As of January 4, 2021:
https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/2018qdr-datasources.pdf
28
Use of the term reference group here mirrors that found in the AHRQ report.
17
of the reference group is subtracted from the AAC for the priority group, and the difference
is tested for statistical significance. The disparity is characterized as improving over time if
the difference between the AAC of the priority population and reference group was less
than –1 percentage point (i.e., in a favorable direction), and the test of the difference had a
p-value < 0.10. The disparity is characterized as worsening if the difference in the AAC
between the groups was more than 1 percentage point and the test of the difference had a
p-value < 0.10. Finally, the disparity is characterized as not changing if the absolute value of
the AAC difference was less than 1 percentage point or the absolute value of the difference
in the AAC was greater than 1 percentage point and the p-value of the test of the difference
was ≥ 0.10.

18
CMS OMH Mapping Medicare Disparities Tool
Overview. This tool was developed to measure and report providers’ performance for
Medicare FFS beneficiaries with social risk factors versus without them. Social risk factors
addressed include race, ethnicity, dual eligibility, sex, and age. The Mapping Medicare
Disparities (MMD) Tool is published on the CMS OMH website.
29
Background. The CMS OMH MMD Tool is an online interactive map that illustrates
comparisons of disparities between groups of Medicare beneficiaries (e.g., racial and ethnic
groups) in health outcomes, utilization, and spending. The tool offers two types of
comparisons: The Hospital View visually compares hospital performance on a range of
metrics and performance scores categorized by geography (e.g., county, state, and
national), hospital type (e.g., acute care and critical access), hospital ownership (e.g.,
government, physician, proprietary, tribal, and voluntary), and/or hospital size (i.e.,
number of beds). This view does not allow comparisons of hospital performance
specifically for different social risk factor groups; it allows comparisons only of hospital
performance overall. However, pertinent to the current effort, the Population View
compares groups according to social risk factors (such as race and ethnicity, age, sex) on
their condition prevalence and on health care utilization, quality, and spending.
Design and methods. The MMD Tool draws on data from CMS administrative enrollment
and claims data for Medicare beneficiaries enrolled in Medicare FFS and includes hundreds
of measures over three dozen conditions.
30
The Population View provides descriptive
statistics by social risk factor group on indicators such as Medicare spending, hospital and
emergency department utilization, preventable hospitalizations, readmission rates, risk-
standardized,30-day,all-cause,
mortality rates for acute myocardial infarction and heart
failure, and discharge destinations for a range of conditions. In this Population View,
measures can be examined at both state and county levels, or by urban versus rural
locations. Comparisons can be made against the national, state, or county average for a
given measure. However, no statistical comparisons are made.
29
Office of Minority Health, “Mapping Medicare Disparities,” online tool, Centers for Medicare and Medicaid
Services, 2020. As of January 4, 2021: https://www.cms.gov/About-CMS/Agency-Information/OMH/OMH-
Mapping-Medicare-Disparities
30
Detail on these measures can be found in NORC at the University of Chicago, “The Mapping Medical
Disparities Tool: Technical Documentation,” Version 8.0, HHS OMH, July 30, 2020. As of January 4, 2021:
https://www.cms.gov/About-CMS/Agency-Information/OMH/Downloads/Mapping-Technical-
Documentation.pdf

19
CMS OMH Reporting of CAHPS and HEDIS Data Stratified by Race and
Ethnicity for Medicare Beneficiaries
Overview. This is an approach to measuring and reporting care provided to Medicare
beneficiaries with social risk factors versus without them. This approach is currently used
to report Medicare Part C and D performance data at contract and state levels stratified by
race and ethnicity on the CMS OMH website.
31
This stratified reporting will be extended to
include rural and urban comparisons in 2021.
Background. The CMS OMH has reported Medicare FFS, Part C, and Part D performance
data, stratified by race and ethnicity (specifically, Asian or Pacific Islander, Black, Hispanic,
and White) annually since 2015. The purpose of stratified reporting in this context is to
provide information for targeting quality improvement activities and resources, to monitor
MA and prescription drug plan (PDP) performance, and to advance the development of
culturally and linguistically appropriate quality improvement strategies. Stratified
estimates of performance by social risk factor are provided for individual MA contracts,
individual PDP contracts, and states (FFS). Statistical comparisons of contract scores are
made to the national average for a particular racial or ethnic group.
Design and methods. Under this stratified reporting approach, patient experience (from the
CAHPS survey) and clinical quality (from HEDIS) measures are evaluated for inclusion in
reporting according to two criteria: reliability, which is the extent to which a given measure
is able to distinguish true differences among plans for a given racial or ethnic group, and
informativeness, which reflects the amount of information about minority group scores that
are not contained in scores for Whites.
32
This latter criterion assesses whether
stratification of data by racial and ethnic groups provides enough new information about
plan performance to justify the loss in precision that comes from basing estimates on fewer
observations (i.e., a smaller sample). The approach imposes certain minimum sample
requirements for reporting a measure; specifically, at least 100 measure completes for MA
contracts and 200 measure completes for individual PDP contracts for a given racial or
ethnic group. Two years of data are combined in each report to increase sample sizes.
Scores that do not meet the minimum sample size threshold or for which reliability is <
0.60 are not reported; scores that meet the sample size requirement and for which
reliability is between 0.60 and 0.70 are reported but flagged as having low reliability.
31
OMH, “Part C and D Performance Data Stratified by Race, Ethnicity, and Gender,” database, CMS, 2020. As of
January 4, 2021: https://www.cms.gov/About-CMS/Agency-Information/OMH/research-and-data/statistics-
and-data/stratified-reporting.html
32
S. C. Martino, R. M. Weinick, D. E. Kanouse, J. A. Brown, A. M. Haviland, E. Goldstein, J. L. Adams, K.
Hambarsoomian, D. J. Klein, and M. N. Elliott, “Reporting CAHPS and HEDIS Data By Race/Ethnicity For
Medicare Beneficiaries, Health Services Research, Vol. 48, No. 2 Pt 1, 2013, pp. 417–434.

20
Minnesota Healthcare Disparities Report
Overview. This measurement approach pertains to Minnesota health plan enrollees and is
used to measure, formally compare, and report providers’ performance for plan members
with social risk factors versus without them. Key social risk factors addressed include race
and ethnicity, preferred language, and country of origin. The report is authored by MN
Community Measurement—an independent collaborative organization that collects,
analyzes, and reports regional data on health care quality and cost—and is published on
this organization’s website.
33
Background. MN Community Measurement publicly reports comparative data on health
care performance for Minnesota patients enrolled in state and federally funded public
programs and private or Medicare-managed programs.
34
Their Minnesota Healthcare
Disparities Report describes medical group performance on health care process and
outcomes using 12 HEDIS measures, stratified by race, Hispanic ethnicity, preferred
language, and country of origin. These measures include
• optimal diabetes care (HEDIS composite measure)
• optimal vascular care (HEDIS composite measure)
• optimal asthma control, adults
• optimal asthma control, children
• colorectal cancer screening
• adolescent mental health and/or depression screening
• adult depression: follow-up at six and 12 months; response at six and 12 months;
remission at six and 12 months.
Composites comprise multiple standard HEDIS measures. For example, optimal diabetes
care is defined as achieving or meeting all of the following: (a) HbA1c less than 8.0 mg/dL;
(b) blood pressure less than 140/90 mm Hg; (c) on a statin medication, unless allowed
contraindications or exceptions are present; (d) non–tobacco user; and (e) patient with
ischemic vascular disease on daily aspirin or antiplatelets, unless allowed contraindications
or exceptions are present.
Design and methods. In this approach, data are reported at two levels. At the state level,
social risk factor groups are compared with each other (e.g., White females versus White
males, non–English-speaking Black patients versus English-speaking Black patients) and
with the overall state average and state average for the social risk factor group for each
measure. At the medical group level, social risk factor groups are compared with the
overall state average and state average for the social risk factor group. Minimum sample
sizes are required to permit reporting; for standard HEDIS measures, a minimum threshold
of 30 patients per medical group is required for public recording. For composite measures,
the minimum threshold for reporting is 60 patients per medical group.
33
MN Community Measurement, Minnesota Health Care Disparities by Race, Hispanic Ethnicity, Language and
Country of Origin: 2019 Report, Minneapolis, Minn., May 2020. As of January 4, 2021:
https://mncmsecure.org/website/Reports/Community%20Reports/Disparities%20by%20RELC/2019%20
Disparities%20by%20RELC%20Chartbook%20-%20FINAL.pdf
34
A. M. Snowden, V. Kunerth, A. M. Carlson, J. A. McRae, and E. Vetta, “Addressing Health Care Disparities
Using Public Reporting,” American Journal of Medical Quality, November 19, 2011.
21
Race, ethnicity, language, and country of origin data are submitted by medical groups and
clinics directly to Minnesota Community Measurement for analysis and reporting, utilizing
an extensive extraction and validation process to ensure that medical groups collect these
data elements from patients using best practices. The best practices include that
• patients self-report their race and Hispanic ethnicity
• patients have the option to select one or more categories for race (i.e., medical
groups/clinics do not collect data using a multiracial category).
Medical groups and clinics must adhere to all of the above best practices for collecting
these social risk factor data to be included in the rate calculation.

22
CMS Assessment of Hospital Disparities for Dual-Eligible Patients
Overview. This approach
35
compares outcomes of care for dual-eligible Medicare
beneficiaries across hospitals and quantifies disparities between dual-eligible and non–
dual-eligible beneficiaries within the same hospital. It focuses on one specific social risk
indicator, dual eligibility status, and one outcome measure, unplanned readmission
following hospitalization for pneumonia.
Background. This approach is used in confidential reporting to hospitals and focuses on
reporting disparities in performance to inform quality improvement efforts. The outcome
measure is specified as the number of unplanned readmissions within 30 days of discharge
for Medicare beneficiaries 65 years and older who were hospitalized at short-term acute
care hospitals following an index admission for pneumonia. The pneumonia measure
cohort includes patients aged 65 years or older enrolled in Medicare FFS in the prior year
with a principal discharge diagnosis of pneumonia or sepsis with secondary discharge
diagnosis of pneumonia coded present on admission. The measure is constructed using
Medicare administrative claims and enrollment data.
Design and methods. Hospital performance on this measure is calculated using two
complementary approaches: The Within-Hospital Disparity Method measures the
difference in outcomes between patients who are dually eligible
36
and patients who are not
dually eligible within a hospital; the Dual Eligible Outcome Method compares performance
on the outcome for dually eligible patients across hospitals. For both approaches, the
outcome is adjusted for patient age and medical conditions at the time of admission and 12
months prior. Results are reported for hospitals with at least 25 patients overall and 12
patients per group (dual-eligible and non–dual-eligible patients).
The Within-Hospital Disparity Method calculates, for each hospital, an absolute rate
difference in the outcomes between patients who are dual-eligible versus those who are
not, within that hospital. As an absolute value, this method does not consider the direction
of the disparity. Under this method, levels of hospital performance are characterized in two
ways: (1) the distribution of the absolute value of the absolute rate difference is divided
into ten equal categories; hospitals falling in higher deciles have larger within-hospital
disparity; and (2) a statistical test of the difference of the disparity from zero.
The Dual Eligible Outcome Method measures and compares hospital performance for the
subgroup of patients who are dual-eligible by calculating a risk-standardized readmission
rate (RSRR) for dual-eligible patients for each hospital. This method also characterizes
performance levels in two ways: (1) the distribution of the dual-eligible specific RSRRs is
divided into ten equal categories; hospitals falling in higher deciles have high dual-specific
RSRRs; and (2) a statistical test of the difference of the RSRR from the national readmission
35
Yale New Haven Health Services Corporation/Center for Outcomes Research and Evaluation, Assessing
Hospital Disparities for Dual Eligible Patients: Thirty-Day All-Cause Unplanned Readmission Following
Pneumonia Hospitalization, New Haven, Conn., 2018. Disparity methods confidential reporting overview, as of
January 5, 2021: https://www.qualitynet.org/inpatient/measures/disparity-methods; disparity methods
confidential reporting methodology, as of January 5, 2021: qualitynet.org/inpatient/measures/disparity-
methods/methodology
36
The demonstration of this approach was focused on full dual eligible beneficiaries.
23
rate of dual-eligible patients, such that performance is worse, no different, or better than
the national rate for dual-eligible patients.

24
CMS OMH Health Equity Summary Score
Overview. The Health Equity Summary Score (HESS)
37
is a summary health equity metric
that is designed to promote and incentivize excellent care for racial and ethnic minorities
and dual- and Low-Income-Subsidy (LIS)–eligible MA beneficiaries. The HESS can be used
to compare performance for patients with social risk factors across providers or assess
improvement in performance for providers’ socially at-risk populations over time, both
within contracts and between contracts.
Background. The HESS is designed to measure both current (cross-sectional) quality of care
and quality improvement and to incentivize good care to both racial and ethnic minorities
and beneficiaries who are dually eligible for Medicare and Medicaid or eligible for a LIS
under Medicare Part D (referred to as DE/LIS eligible). The HESS summarizes performance
across two types of data: (1) patient experience, as measured by CAHPS: doctor
communication, ease of getting needed care, getting care quickly, ease of getting needed
prescription drugs, customer service, care coordination, and flu immunization; and (2)
clinical care, as measured by HEDIS: breast cancer screening, colorectal cancer screening,
diabetes care (both nephropathy and retinal exam), and adult body mass index assessment.
Both types of data are linkable to social risk factors at the level of the individual Medicare
beneficiary, and the measures that are included in the HESS are continually evaluated for
their suitability for inclusion.
Design and methods. The cross-sectional component of the HESS combines the two most
recent years of data, while the improvement (i.e., performance over time) score compares
performance in the two most recent years with performance in the two years prior. To
assure accurate measurement, a plan’s HESS is based only on the combination of social risk
factor groups and measures for which there is sufficient sample size of 100 and reliability
greater than or equal to 0.7. For improvement measures, this must hold at both baseline
and follow-up. For each measurable MA contract, the HESS is based on however many
social risk factor groups can be reliably measured, and information is combined to give
equal weight to each social risk factor group. To be eligible to receive a HESS score, an MA
contract must have a minimum of 500 enrollees and publicly reported quality scores,
including a Medicare Part C summary rating and at least one CAHPS or HEDIS Medicare
Star rating.
The process for calculating the HESS is visually depicted in Figure 4.2. Cross-sectional
performance for each measurable racial and ethnic minority group and for DE/LIS-eligible
beneficiaries is estimated using linear models, yielding one score for each social risk factor
group for each measure. All measures are rescaled to a 0–100 scale and modeled
separately, and estimates are standardized to put them on a common scale across
measures and groups. The standardized estimates are then combined across measures and
social risk factor groups to yield a single cross-sectional performance score for each MA
contract. Performance scores are converted to a five-star scale using the Medicare Part C
37
D. Agniel, S. C. Martino, Q. Burkhart, K. Hambarsoomian, N. Orr, M. K. Beckett, C. James, S. H. Scholle, S.
Wilson-Frederick, J. Ng, and M. N. Elliott, “Incentivizing Excellent Care to At-Risk Groups with a Health Equity
Summary Score,” Journal of General Internal Medicine, November 2019
.

25
clustering algorithm.
38
Improvement scores combine both a within-plan component and a
between-plan, or benchmarked, component. The within-plan component measures the
narrowing or widening of within-plan disparities (between the two-year baseline period
and the two-year performance period) and compares—measure by measure—
performance for all lagging groups to performance for the leading group (i.e., the group
with the highest baseline score on a measure) of each contract. The between-plan or
nationally benchmarked component measures the improvement of each social risk factor
group compared with that group’s national average improvement. As with the cross-
sectional score, this procedure is undertaken for each measurable racial and ethnic
minority group and for DE/LIS beneficiaries. Cross-sectional and improvement scores are
blended according to the scheme in Figure 4.3. As the figure shows, low improvement
scores cannot result in a blended score lower than a plan’s cross-sectional score, which
prevents high-performing plans from being penalized for what may be necessarily limited
improvement. By design, improvement counts more toward a contract’s HESS when cross-
sectional performance is lower, to encourage and reward improvement for low-performing
plans. For example, as can be seen in Figure 4.3, a contract that scores one star on the
cross-sectional component of the HESS can earn an additional blended star if it achieves
four stars for improvement, and it can earn two additional blended stars if it achieves five
stars for improvement. Finally, a contract’s HESS is computed by averaging its blended
score for race and ethnicity and its blended score for DE/LIS to produce a final composite
score. Composite HESS scores are generated separately for clinical care and patient
experience.
38
CMS, “Medicare 2020 Part C & D Star Ratings Technical Notes,” October 2019. As of January 5, 2021:
https://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovGenIn/Downloads/Star-
Ratings-Technical-Notes-Oct-10-2019.pdf

Figure 4.2. Components of the HESS
Within-Plan Improvement:
Race and Ethnicity
Nationally-Benchmarked
Improvement:
Race and Ethnicity
Within-Plan Improvement:
DE/LIS
Nationally-Benchmarked
Improvement:
DE/LIS
Cross-Sectional Score:
Race and Ethnicity
Improvement Score:
Race and Ethnicity
Cross-Sectional Score:
DE/LIS
Improvement Score:
DE/LIS
Blended Score:
Race and Ethnicity
Blended Score:
DE/LIS
HESS Score:
Race/Ethnicity and DE/LIS
Cross-
sectional
stars
Figure 4.3. HESS: Blending Scheme
Improvement stars
missing 1 2 3 4 5
1
2
3
4
5
1 1 1 1 2 3
2 2 2 2 3 3
3 3 3 3 3 4
4 4 4 4 4 5
5 5 5 5 5 5
26

27
Zimmerman Health-Related Quality of Life Approach to Assessing Health
Equity
Overview. Like the HESS, this approach by Zimmerman
39
synthesizes information across
multiple measures, in this case using a health-related quality of life criterion. The approach
is oriented toward quantifying the total deviation of a population from a defined privileged
group and allows disaggregation, e.g., to the level of states.
Background. This health equity measure compares the average health-related quality of life
of individuals within numerous social categories (race, ethnicity, sex, and income) to the
average quality of life of individuals from a privileged social category: specifically, high-
income White men. The assumption undergirding this measure is that wealthy White men
hold the highest social privilege in the United States, and therefore it is their experience
that is the relevant comparison standard. Moreover, while the identities of socially
marginalized groups have changed over time, as have the ways in which marginalization
translates into health outcomes, the privileged status of upper-income White men has been
stable for decades. In using wealthy White men as the comparator, the measure implicitly
treats gender, race, and income as the social risk factors of interest. The health experiences
of all those who do not belong to the privileged group are included in the computation of
the measure, though scores for specific subgroups (e.g., low-income Black women) can be
derived.
Design and methods. The proposed measure conceptually defines health disutility as the
“distastefulness” associated with one’s health falling short of the optimal achievable health.
To build this approach, 2017 Behavioral Risk Factor Surveillance System data were used
from adults aged 18 to 64 years from all 50 states and the District of Columbia. The key
outcome is a measure of healthy days derived from the Centers for Disease Control and
Prevention’s health-related quality of life scale. This scale was constructed by summing the
answers to two questions about how many days in the previous 30 days the respondent felt
that their mental or physical health was not good, rescaled such that higher scores equal
more healthy days and age-adjusted. To calculate the measure, for each state, a health
deficit was defined for each individual in the group as the amount by which their health
falls below the average health in the most privileged group. The metric can be summed
over the total state population to get the mean value of distastefulness for the state or can
be summed over specific social groups, for example, to show how the health of low-income
Black women compares with the health of the privileged group within that state.
39
F. J. Zimmerman, “A Robust Health Equity Metric,” Public Health, Vol. 175, 2019, pp. 68–78.

28
Zimmerman and Anderson Approach to Evaluating Trends over Time in
Health Equity
Overview. This approach by Zimmerman and Anderson
40
focuses on changes in patterns of
health disparities and health equity over a 25-year period at different geographic levels and
summarizes that information using a health-related quality of life criterion. In many ways,
this is a longitudinal counterpart to the approach described on the previous page. Here, too,
the social risk factors encompassed by the method are race and ethnicity, sex, and income.
Background. Health equity is defined across multiple dimensions, including health
disparities, or differences in health outcomes among groups; health inequality, or the
overall variation in health across individuals without regard to social group; and health
justice, or the correlation of health outcomes with social attributes, e.g., economic status.
Design and methods. To build the approach, 25 years of Behavioral Risk Factor Surveillance
System data from adults aged 18 to 64 years were used to assess two key outcomes: self-
reported general health on a 5-point scale (excellent, very good, good, fair, poor) and
healthy days, which is the mean number of self-reported healthy days for physical and
mental health during the past 30 days. For each of these two outcomes, four different
measures of health equity are assessed: (1) Black-White disparity: mean difference in the
health outcome between White and Black individuals; (2) income disparity: mean
difference in the health outcome between top, middle, and bottom income categories; (3)
health justice: variation in health outcome that is not explained by sex, income, or
race/ethnicity; and (4) a summary health equity measure that is the mean weighted
departure of individual health from best achievable health. The summary health equity
measure is the only one of the three that combines information across the self-reported–
health and healthy days outcomes. This summary measure is weighted such that larger
departures from the best achievable health are weighted more heavily than smaller
departures, and best achievable health is defined as the average outcome of the most
privileged identifiable group (White men in top income category). Each measure is
calculated for the nation overall, as well as for each state and year combination for which
data were available. This approach provides information about trends in health equity
(across the four dimensions) over time.
40
F. J. Zimmerman and N. W. Anderson, “Trends in Health Equity in the United States by Race/Ethnicity, Sex,
and Income, 1993–2017,” JAMA Network Open, Vol. 2, No. 6, 2019, pp. e196386.

29
4. Summary of Identified Health Equity Measurement Approaches
Table 4.1 summarizes the ten approaches that were identified. Some of the identified
approaches focused primarily on determining which existing quality measures are suitable
for health equity comparisons (i.e., permit reliable and valid comparisons among social risk
factor groups) or for measuring organizational structures, systems, and processes
hypothesized to promote the delivery of high-quality care for all. Other approaches focused
primarily on making measure-by-measure comparisons, either making comparisons
between providers in how they stack up against a higher-level standard or making
comparisons within a provider or other reporting unit. Finally, some of the identified
approaches focused on developing a system for combining different dimensions of health
equity into a single summary index. Table 4.1 identifies the primary focus of each measure
and further characterizes measures within those three primary categories.
The Measurement Framework for Evaluating How Well an Organization Meets National
CLAS Standards (HHS OMH) and the NQF Disparities-Sensitive Measure Assessment
both
identified existing measures of processes for improving health equity, including
organizational structures, systems, and processes that are hypothesized to promote the
delivery of equitable care. The underlying assumption of these approaches is that such
measures provide an assessment of how committed health care organizations are to the
goal of providing equitable care and how equipped they are to meet the needs of a
culturally and demographically diverse mix of patients. As mentioned above, our literature
review identified several other articles and reports that similarly described such measures.
Because there was a large degree of overlap among the specific measures identified in
these articles and reports, we decided to bring only these two reports to the TEP for their
evaluation, in the interest of expediency. The HHS OMH approach was the most recent and
comprehensive of the articles and reports that we identified, and the NQF Disparities-
Sensitive Measure Assessment identified additional categories of quality measures (e.g.,
preventive care, processes of care, and health outcome measures) above and beyond what
fit under the CLAS rubric (and thus was of additional value).
Two approaches—the AHRQ National Healthcare Quality and Disparities Report and the
CMS OMH MMD Tool—focused on making performance comparisons by social risk factor
groups within a reporting unit on a measure-by-measure basis. In the case of the AHRQ
National Disparities Report, the reporting unit is the nation, and the broad array of
measures included access to care, processes of care, outcomes of care, and patient
experiences of care (CAHPS). The AHRQ report focuses both on current cross-sectional
performance and improvement in performance over time, using both statistical significance
and magnitude criteria to identify meaningful differences in care across social risk factor
groups. The CMS OMH MMD Tool focuses, one-by-one, on an even broader array of
measures, all of which are derived from Medicare claims data and thus pertain to Medicare
FFS only. The measures include chronic disease prevalence, health care utilization and
spending, mortality rates, and patient safety measures but do not involve tests of statistical
significance or magnitude criteria for identifying meaningful differences. The CMS OMH
30
MMD Tool does, however, allow users to view disparities data at more granular levels of
geography, including state and county levels.
CMS OMH reports scores from the CAHPS and HEDIS, stratified by race, ethnicity, and
gender, and also provides two separate views of this information. One view facilitates
comparisons of performance of MA and PDP contracts and states in the quality of care they
provide to a particular racial or ethnic group or to rural or urban residents. The other view
facilitates comparisons of performance within MA and PDP contracts and states in the
quality of care provided to different racial and ethnic groups and in urban versus rural
areas. In each case, the focus is on cross-sectional performance, comparisons are made
measure-by-measure, and statistical comparisons to the national average for each social
risk factor group are provided.
The Minnesota Healthcare Disparities Report, issued annually by Minnesota Community
Measurement, presents data on a set of clinical process of care measures (HEDIS) stratified
by race, ethnicity, preferred language, and country of origin. Stratified data are presented at
the state level and at the medical group level. This approach, too, focuses on measure-by-
measure comparisons. At the state level, scores for social risk factor groups are compared
with each other and to overall statewide averages on each measure. The state-level
reporting is similar to one of the options provided by the CMS OMH MMD Tool and to the
CMS OMH stratified reporting of Medicare FFS data at the state level. At the medical group
level, scores for social risk factor groups are compared with overall statewide averages and
state averages specific to the social risk factor group. The medical group–level reporting is
similar to the CMS OMH stratified reporting of MA and PDP performance data at the
contract level, in that both present between- and within-provider comparisons. However,
the data presented by the CMS OMH span the nation, whereas the data presented in the
Minnesota Healthcare Disparities Report is limited to the state of Minnesota. Like the CMS
OMH MMD Tool and the CMS OMH stratified reporting approach, the Minnesota Healthcare
Disparities Report focuses on cross-sectional performance.
The CMS Assessment of Hospital Disparities for Dual-Eligible Patients focuses on a single
social risk indicator, dual-eligibility status, and a single outcome measure, 30-day all-cause
unplanned readmission following hospitalization for pneumonia, but the principles of this
approach could be applied more broadly. Performance for dual-eligible patients is
compared across hospitals using criteria of statistical significance and magnitude of
differences. Performance is also compared within hospitals for dual-eligible and non–dual-
eligible beneficiaries, again using criteria of statistical significance and magnitude of
differences. This approach is one of only three identified approaches that include a
magnitude criterion for distinguishing ten levels of performance. The other two approaches
that use such a criterion are the AHRQ National Disparities Report and the CMS OMH HESS.
The CMS OMH HESS approach identified CAHPS and HEDIS measures suitable for health
equity comparisons (based on criteria of reliability and reportability) and uses data on
those measures to assess the extent to which care provided through MA contracts was
equitable according to race and ethnicity and dual/LIS-eligibility status. This approach
compares both cross-sectional performance and improvement in performance for racial
and ethnic minority groups and for dual/LIS-eligible beneficiaries across contracts relative
to national averages for each group. This approach also compares performance for
different racial and ethnic groups and for dual/LIS eligible and noneligible beneficiaries
within contracts. The HESS is one of three identified approaches that developed a system
31
for combining different dimensions of health equity into a single equity measure (the other
two being the approaches by Zimmerman and by Zimmerman and Anderson, described
next). In particular, the HESS combines data across multiple measures, multiple social risk
factors, and across multiple types of comparisons, i.e., both within- and between-provider
comparisons and comparisons focused on both cross-sectional performance and
improvement in performance. Performance is summarized on a 1-to-5-star scale. A
dashboard for presenting HESS data to MA contracts confidentially is under development.
On that dashboard, contracts can drill down to see data for each measure and group to
pinpoint their areas of strength and weakness.
Like the CMS OMH HESS, the Zimmerman Health-Related Quality of Life Approach to
Assessing Health Equity synthesizes information across more than one measure rather
than examining the measures individually, as is done, e.g., in the AHRQ and CMS OMH
stratified reporting approaches. Zimmerman’s approach is oriented toward assessing the
total deviation from a defined privileged group (high-income White males) and allows
disaggregation from the national level to the level of states and smaller geographic areas.
Although this approach—which focuses on cross-sectional performance only—implicitly
describes being female, low-income, and non-White as risk factors, it does not allow for
making distinctions among these groups, i.e., it treats them collectively as a singular
disadvantaged group.
In part, the Zimmerman and Anderson Approach to Evaluating Trends over Time in Health
Equity is comparable to the approach taken in the AHRQ National Disparities Report to look
at trends over time. It uses 25 years of Behavioral Risk Factor Surveillance System data to
examine trends in health disparities by race (Black versus White individuals) and income
and uses statistical tests of trend information to characterize disparities in self-rated health
and healthy days in the past month as either decreasing, increasing, or not changing (no
trend identified). The Zimmerman and Anderson approach is also similar to the
Zimmerman Health-Related Quality of Life Approach to Assessing Health Equity and the
CMS OMH HESS, in that it combines information on multiple measures and summarizes
information on equity across social risk factors (race and ethnicity, sex, and income).
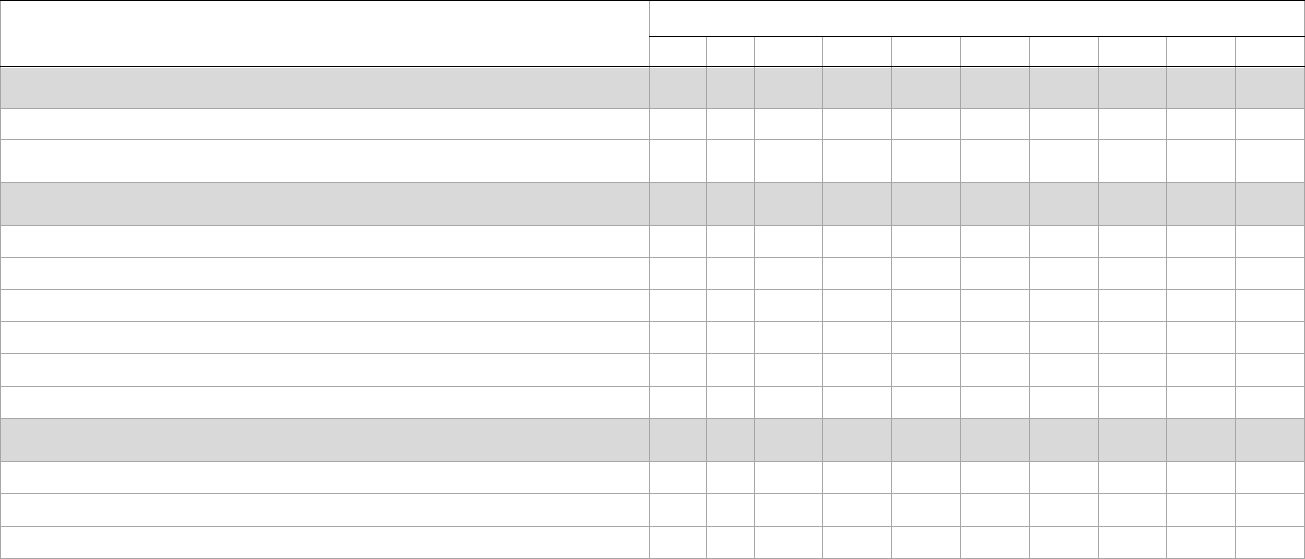
Table 4.1. Summary of Identified Approaches to Health Equity Measurement
Approach (see key below)
1 2 3 4 5 6 7 8 9 10
Approach focused primarily on measure identification
x x
Identified existing measures of processes for improving health equity
x x
Assessed suitability of existing quality measures for health equity
comparisons
x x
Approach focused primarily on measure-by-measure comparisons
x x x x x x
Made between-provider (or other reporting unit) comparisons
x x x x x
Made within-provider (or other reporting unit) comparisons
x x x x x x x
Examined cross-sectional (point-in-time) performance
x x x x x x x
Examined on improvement in performance
x x x
Included use of statistical tests of differences
x x x x x
Included consideration of magnitude of differences
x x x
Summary indices of health equity
x x x
Combined information on multiple measures
x x x
Combined information on multiple social risk factors
x x x
Combined information on multiple types of comparisons
a
x
a
For example, between- and within-unit comparisons or comparisons focused on cross-sectional performance and improvement in performance.
NOTES: Approach 1 = Measurement Framework for Evaluating How Well an Organization Meets National CLAS Standards (HHS OMH); Approach 2 = NQF Disparities-
Sensitive Measure Assessment; Approach 3 = AHRQ National Healthcare Quality and Disparities Report; Approach 4 = CMS OMH Mapping Medicare Disparities Tool;
Approach 5 = CMS OMH Reporting of CAHPS and HEDIS Data by Race/Ethnicity for Medicare Beneficiaries; Approach 6 = Minnesota Healthcare Disparities Report;
Approach 7 = CMS Assessment of Hospital Disparities for Dual-Eligible Patients; Approach 8 = CMS OMH Health Equity Summary Score; Approach 9 = Zimmerman Health-
Related Quality of Life Approach to Assessing Health Equity; Approach 10 = Zimmerman and Anderson Approach to Evaluating Trends Over Time in Health Equity.
32

33
5. Technical Expert Panel Process and Members
The project team convened a TEP via videoconference to discuss the measurement of
health disparities and health equity and incorporation of health equity measures or
domains in Medicare VBP and quality reporting programs. RAND researchers constructed
an initial list of potential panelists with expertise in social risk factors, health disparities,
health equity, risk adjustment, value-based and alternative payment models, and
Medicare’s VBP programs. This initial list was founded on the team’s knowledge of the field
and a preliminary review of recent literature on the topics of health disparities and health
equity measurement. A final list was constructed in consultation with ASPE. The final list
consisted of eight first-choice experts and eight alternates. All eight first-choice experts
agreed to participate on the panel. Biographical information about each of the expert
panelists is provided in Appendix C.
The project team developed a TEP notebook, which was shared with panelists five days
prior to the first of two meetings held eight days apart. The notebook consisted of a TEP
charter; biographies of the participating panelists; project background, objectives, and
methods used to identify health equity measures and approaches; descriptions of each of
the ten approaches to health equity measurement that were identified via the literature
review; and preliminary criteria for evaluating those approaches. The team also distributed
rating sheets to facilitate the assessment of each approach according to the rating criteria
and to solicit additional commentary from the panelists.
During the initial meeting, the TEP was asked to provide feedback on the team’s proposed
definition of a health equity measure and categorization of features of health equity
measures. At that initial meeting, the panel was also tasked with coming to a consensus on
a final set of criteria for evaluating the identified approaches to health equity measurement
and to begin discussing the identified approaches. Approaches that were not discussed at
the initial meeting were discussed at the second meeting. To facilitate the discussion, the
team presented an overview of each approach and invited the TEP members to engage in a
focused discussion following each overview. Each meeting lasted two hours. A project team
member took notes during the discussion, and the meetings were audio recorded for
additional notetaking afterward.
The team updated the rating criteria in response to the feedback given during the initial
meeting and distributed the revised rating sheet directly following the first meeting. TEP
members submitted their ratings for all ten approaches to health equity measurement
using the updated rating criteria within ten days of the second meeting. The team drew on
the input provided by the TEP via the rating sheets, verbal comments made during the
meetings, comments submitted using the teleconferencing platform’s chat function, and
email messages sent after the meetings to provide the following assessment.

34
6. TEP Input on Project Framing and Approach
Input on Definition of a Health Equity Measurement Approach
TEP members pointed out that membership in defined “at-risk” groups is often not a direct
mechanism for risk of receiving poor quality care but a proxy for more direct risk factors,
such as food insecurity and homelessness. The group acknowledged, however, that
researchers tend to rely on group membership as a proxy for direct mechanisms when
constructing equity measures or assessing disparities because data on direct mechanisms
is often unavailable. Moreover, members of some “at-risk” groups—e.g., racial and ethnic
minorities—are especially likely to experience discrimination and other inequities based
on group membership; in such instances, group membership on its own is a direct
mechanism of interest. Nevertheless, the TEP emphasized the importance of encouraging
organizations to collect additional data about risk factors rather than relying solely on data
about group membership to assess equity and identify targets for improvement.
Relatedly, the TEP counseled that a measure of health equity should not be limited to
comparing quality of care provided to groups predetermined to be disadvantaged, e.g.,
racial and ethnic minority patients to a reference group that is predetermined to be
advantaged, e.g., White patients. Keeping with the racial/ethnic example, one issue is that
White patients may not be the group for which performance is highest on a measure. Even
if White patients are the group for which performance is highest on a measure, they may
still be getting suboptimal care. In either case, using care received by White patients as the
benchmark for racial and ethnic minority patients would not encourage the highest-quality
care possible for racial and ethnic minority patients. Moreover, the practice of defining and
comparing to a reference group may imply a standard for nonreference groups, suggest that
those groups are nonnormative, and promote a need for assimilation and acculturation.
Rather than using the quality of care provided to one prespecified group as the benchmark
for other groups, the TEP advocated adopting a framework for equity that focuses on
making sure that all groups and people are provided with the care and resources they need
to achieve optimal health. In practice, this could mean comparing all other groups with the
highest-performing group, regardless of whether the highest-performing group is
nominally “at risk,” comparing all groups to an overall state or national average, or
adopting an approach that focuses on improvement rather than on point-in-time
performance for a group. The TEP also emphasized that achieving high-quality care for all
groups requires aligning care and resources with patient needs and preferences to
optimize their health rather than defining outcomes based on a predetermined reference
group that has certain advantages along one or more dimensions. Furthermore, the TEP
encouraged adopting a framework for equity that sets a universal target of excellent care
for all groups and all people but that recognizes that the best care for a given group or
person may require tailoring and customization of care.
This view of health equity as maximizing opportunities for all to be healthy is reflected in
the philosophy of the Robert Wood Johnson Foundation’s Health Opportunity and Equity

35
(HOPE) Initiative.
41
The HOPE Initiative tracks social and economic factors, community and
safety factors, physical environment factors, access to health care, and a limited set of
health outcomes (infant mortality, low birthweight, premature mortality, and self-rated
health) by race and ethnicity and socioeconomic status for tracking progress toward health
equity at the state and national level. Although this framework does not fit with the
definition of a health equity measurement approach developed for this project, it is one
that merits future consideration for its applicability to the assessment of health care
organizations.
Input on Premise of the Project
TEP members also felt it was important for the research team to acknowledge that there is
currently little empirical evidence that pay-for-performance and quality reporting
strategies translate into reduction of disparities. Thus, if CMS were to incorporate one or
more of the health equity measurement approaches identified by this project in a VBP or
reporting program, it would be important to evaluate the impact on health equity so that
this evidence base can be established. TEP members also advised that careful consideration
should be given to the way payment is tied to performance on health equity measures.
Consistent with our definition of a health equity measurement approach, TEP members felt
that payment on the equitable delivery of care should be reserved for the purpose of
improving care for at-risk populations and that the number of high-risk patients that an
organization serves should be considered as part of any payment scheme, as this partly
determines the magnitude of an organization’s contribution to health equity nationally.
Input on Evaluation Criteria
The research team developed a preliminary set of criteria for evaluating the health equity
measurement approaches identified by the literature review. The TEP provided input on
those criteria during the first TEP meeting. The revised set of criteria, which incorporates
the TEP’s feedback, is shown in Table 6.1.
The criterion that social risk factor groups be measured at the most granular level possible
did not appear in the preliminary set developed by the research team. This criterion was
discussed in the context of race and ethnicity, with TEP members emphasizing the
importance of characterizing the needs of smaller groups when possible and distinguishing
the needs of subgroups who are sometimes combined to boost sample sizes, e.g., Asians
and Pacific Islanders. TEP members acknowledged that most organizations are unlikely to
have the sample sizes required for stable, meaningful measurement of small groups but
that developers of health equity measurement approaches should at least attempt
measurement of care for small groups (perhaps by pooling data across years or reporting
units) and report on any trade-offs involved in doing so. The TEP also emphasized the
importance of having accurate data on patient race and ethnicity. Self-report is the gold
41
Robert Wood Johnson Foundation, “Measures to Advance Health and Opportunity,” HOPE Initiative
homepage, undated. As of January 7, 2021: https://www.hopeinitiative.org/

36
standard for collecting data on race and ethnicity,
42
but the process for eliciting information
about race and ethnicity in a way that best captures how Medicare beneficiaries identify
themselves has evolved over time and will require continued attention to keep pace with
demographic and cultural trends in the United States.
43
Another criterion that did not
appear in the preliminary set is the one pertaining to the likely impact of adopting an
approach into a Medicare VBP or reporting program on how equitably organizations
provide care to their patients. The TEP felt that it was important to add such an overall
evaluation of whether implementing an approach in its currently specified form would help
achieve the goal of health equity.
42
D. J. Klein, M. N. Elliott, A. M. Haviland, P. A. Morrison, N. Orr, S. Gaillot, and R. Weech-Maldonado, “A
Comparison of Methods for Classifying and Modeling Respondents Who Endorse Multiple Racial/Ethnic
Categories,” Medical Care, Vol. 57, 2019, pp. e34–e41.
43
U.S. Census Bureau, “Research to Improve Data on Race and Ethnicity,” webpage, U.S. Department of
Commerce, 2017. As of January 7, 2021: https://www.census.gov/about/our-research/race-ethnicity.html
37
List 6.1. Revised Criteria for Evaluating Health Equity Measurement Approaches
Evidence-based
Is the approach based on available evidence of the relationship between the social risk factor and outcome?
Usability
Is the approach designed to incentivize achievement or improvement for at-risk beneficiaries?
Does the approach guard against unintended consequences of worsening quality or access or disincentivizing
resources for any beneficiaries?
Measurement Equivalence
Is the approach appropriate for use with all social risk factor groups, or is it applicable only to certain groups?
Breadth of Applicability
Is the approach suitable only to a specific VBP or quality reporting program, or can it be more to multiple
providers and settings?
Reliability
Is the approach able to distinguish performance between providers/programs?
Does the approach capture granular subgroups where possible while limiting the influence of imprecise
estimates?
Impact
How likely is it that incorporating this measure or approach in a VBP or quality reporting program would result in
a noticeable improvement in health equity?

38
7. Detailed Assessment of Identified Approaches
Measurement Framework for Evaluating How Well an Organization Meets
National CLAS Standards
TEP members’ ratings of this approach are shown in Table 7.1. A majority of members
(five) fully agreed that this approach is evidence-based, and all either fully or partially
agreed that the approach is designed to incentivize achievement or improvement for at-
risk beneficiaries. Members were divided in their assessment of whether the approach
guards against unintended consequences of worsening access or resources for at-risk
beneficiaries and whether the approach is able to reliably distinguish performance among
providers; in each case, four members said that the approach either fully or partially meets
the criterion, three said that there is not enough information to tell, and one member said
that the approach does not meet the criterion. Most members (five) said that the approach
is applicable to particular groups, several specifically highlighting applicability to people
with limited English proficiency and racial and ethnic minority groups. Four of seven
members
44
said that the approach is applicable to multiple VBP or reporting programs. A
majority of members (five) felt that incorporation of the approach in a VBP or reporting
program would somewhat or very likely result in a noticeable improvement in health
equity.
In discussing this approach, TEP members pointed out that much is still unknown about
the structures, processes, and systems that are necessary to foster health equity. One
member referenced a study by Blustein and colleagues
45
that demonstrated that a hospital
could perform well on structural measures thought to facilitate high-quality care for racial
and ethnic minority patients but not make a significant contribution to reducing racial and
ethnic disparities in hospital care. Given such findings, TEP members felt that further
evidence of the direct impact of constructs included in the National CLAS Standards on
health equity would be needed before they could confidently say that incorporation of this
approach into a VBP or reporting program would have the desired impact on health equity.
TEP members felt that some of the cross-cutting measures identified by Davis and
colleagues would be more likely to foster health equity than others if tied to an incentive
scheme. For example, one member mentioned that the CAHPS Cultural Competence Item
Set, the CAHPS Item Set for Addressing Health Literacy, and a measure of the percentage of
patients with limited English proficiency who get appropriate linguistic support are
valuable in that they measure the desired outcome—provision of culturally and
linguistically appropriate services—directly. On the contrary, some members felt that
process measures, such as screening for and recording cultural and language issues, are
less useful in that the absence of such documentation does not mean that services were not
44
One member did not complete this rating for this measurement approach. Two members did not complete
the rating of whether this approach captures granular subgroups where possible. Otherwise, all eight
members completed every rating for every approach.
45
J. Blustein, J. S. Weissman, A. M. Ryan, T. Doran, and R. Hasnain-Wynia, “Performance in Medicaid Can
Efficiently Reduce Racial and Ethnic Disparities,” Health Affairs, Vol. 30, No. 6, 2011, pp. 1165–1175.
39
provided, and the presence of such documentation does not necessarily mean that patients
got more appropriate care. This is not to say that these measures are not valuable, just that
they should not be used as proxies for the quality of care that is delivered.
Another disadvantage of this approach identified by one TEP member is that it does not
recognize or reward the ability of an organization to address patient needs by financial
situation or, more generally, by social class. Finally, one member felt that collection of the
data needed for this approach would be “exceedingly burdensome” for organizations,
particularly given that the impact of assessing adherence to CLAS standards is still largely
unknown.

Table 7.1. TEP Ratings of Measurement Framework for Evaluating How Well an Organization
Meets National CLAS Standards
Not Enough
Meets Partially Meets Does Not Meet
Criterion Information to
Criterion Criterion Criterion
Determine
Is the approach based on available evidence
of the relationship between the social risk 5
factor and outcome?
Is the approach designed to incentivize
achievement or improvement for at-risk 3
beneficiaries?
Does the approach guard against
unintended consequences for at-risk 2
beneficiaries?
Is the approach able to reliably distinguish
2
performance between providers?
2 1
5
2 1 4
2 1 3
Appropriate Not Enough
Appropriate
for Particular Information to
for All Groups
Groups Determine
Is the approach appropriate for use with all
5 2 1
social risk factor groups?
Applicable to Applicable to Not Enough
Multiple One Program Information to
Programs Only Determine
Is the approach applicable only to a specific
VBP or reporting program, or can it be 4 3
applied more broadly?
Not Enough
Yes No Information to
Determine
Does the approach capture granular
1 5
subgroups where possible?
Somewhat Somewhat
Very Likely Very Unlikely
Likely Unlikely
How likely is it that incorporating this
approach into a VBP or reporting program
1 4 1 2
would result in a noticeable improvement in
health equity?
NOTE: Values are the number of experts who gave a particular rating. Model response is shown in bold.
40
41
NQF Disparities-Sensitive Measure Assessment
TEP members’ ratings of this approach are shown in Table 7.2. Nearly all members (seven)
fully agreed that this approach is evidence-based, and nearly all (seven) either fully or
partially agreed that the approach is designed to incentivize achievement or improvement
for at-risk beneficiaries. Members were divided in their assessment of whether the
approach guards against unintended consequences of worsening access or resources for at-
risk beneficiaries, with four members saying that there is not enough information to tell,
and four saying that the approach either fully or partially fulfills this criterion. A majority of
members (five) fully or partially agreed that the approach is able to reliably distinguish
performance among providers. A majority (five) also said the approach is applicable to
particular groups, sometimes noting a particular focus on racial and ethnic minority
groups, and that the approach is applicable to multiple VBP or reporting programs. Nearly
all members (seven) felt that incorporation of the approach in a VBP or reporting program
would somewhat or very likely result in a noticeable improvement in health equity.
In commenting on this approach, most TEP members felt that its principal advantage is in
the way that it formally and rigorously vetted a large group of measures for possible
inclusion in a stratified reporting scheme or other approach to health equity measurement.
Many also emphasized the advantage of the measures being NQF-endorsed, and several
highlighted that some of the measures are based on claims data, which alleviates data
collection burden. Most members commented that the usability, applicability, and
reliability of the approach would depend on how the disparities-sensitive measures were
used in a health equity metric or reporting program. Even so, nearly all felt that
incorporating measures determined to be disparities-sensitive into a more complete
approach to health equity measurement could have a noticeable impact on health equity,
particularly if rewards are focused on improvements for at-risk populations toward
feasible and desired benchmarks.

Table 7.2. TEP Ratings of NQF Disparities-Sensitive Measure Assessment
Not Enough
Meets Partially Meets Does Not Meet
Criterion Information to
Criterion Criterion Criterion
Determine
Is the approach based on available evidence
of the relationship between the social risk 7 1
factor and outcome?
Is the approach designed to incentivize
achievement or improvement for at-risk 4 3 1
beneficiaries?
Does the approach guard against
unintended consequences for at-risk 2 2 4
beneficiaries?
Is the approach able to reliably distinguish
performance between providers?
4 1 1 1
Appropriate
for Particular
Groups
Appropriate
for All Groups
Not Enough
Information to
Determine
Is the approach appropriate for use with all
social risk factor groups?
5 3
Applicable to
Multiple
Programs
Applicable to
One Program
Only
Not Enough
Information to
Determine
Is the approach applicable only to a specific
VBP or reporting program, or can it be
applied more broadly?
5 3
Yes No
Not Enough
Information to
Determine
Does the approach capture granular
subgroups where possible?
4 1 1
Very Likely
Somewhat
Likely
Somewhat
Unlikely
Very Unlikely
How likely is it that incorporating this
approach into a VBP or reporting program
would result in a noticeable improvement in
health equity?
1 6 1
NOTE: Values are the number of experts who gave a particular rating. Model response is shown in bold.
AHRQ National Healthcare Quality and Disparities Report
TEP members’ ratings of this approach are shown in Table 7.3. Nearly all members (seven)
fully agreed that this approach is evidence-based, but there was considerable uncertainty
about whether the approach is designed to incentivize achievement or improvement for at-
risk beneficiaries. There was also considerable uncertainty about whether the approach
42
43
guards against unintended consequences of worsening access or resources for at-risk
beneficiaries, with five members saying that there is not enough information to tell and two
saying that the approach does not meet this criterion. Only two members fully or partially
agreed that the approach is able to reliably distinguish performance among providers—
one member commented that there is likely too little data to make this approach feasible at
the level of individual providers—but a majority (five) said the approach is applicable to all
social risk factor groups. Six members said that the applicability to VBP or reporting
programs is uncertain. Members were divided about whether incorporation of the
approach in a VBP or reporting program would result in a noticeable improvement in
health equity; five said that such an outcome would be somewhat likely, one said that it
would be somewhat unlikely, and two said that it would be very unlikely.
Some TEP members commented that the major limitation of this approach is the
heterogeneity of the measures included and their selection based on availability in federal
data sets. It was noted that some of the measures are relevant only at the population level
but that many are applicable to hospitals, plans, and other health care organizations, and
thus are potentially useful for one or more Medicare VBP and quality reporting programs.
However, the majority opinion was that additional work would be needed to determine
exactly how this approach could be operationalized at these finer levels of analysis. One
member commented that although the analytic methods are robust, the approach does not
appear applicable to the task of comparing provider performance or showing providers
their performance relative to peers or benchmarks. Several members questioned the
appropriateness of comparing groups of patients to predefined reference groups and
pointed out that catching disadvantaged patients up to a predefined reference group is only
a small part of achieving health equity. One member expressed a strong preference for an
approach that rewards any meaningful improvement for a high-risk group, stating that,
absent such a criterion, providers could be rewarded for providing substandard care to all
groups equally or worsening care for leading groups. Some also expressed concerns about
the degree of risk adjustment involved in this approach, with a couple commenting that
some measures used in this approach could be heavily influenced by social factors for
which adjustments are not currently being made.

Table 7.3. TEP Ratings of AHRQ National Healthcare Quality and Disparities Report
Not Enough
Meets Partially Meets Does Not Meet
Criterion Information to
Criterion Criterion Criterion
Determine
Is the approach based on available evidence
of the relationship between the social risk 7
factor and outcome?
Is the approach designed to incentivize
achievement or improvement for at-risk 2
beneficiaries?
Does the approach guard against
unintended consequences for at-risk 1
beneficiaries?
Is the approach able to reliably distinguish
1
performance between providers?
1
2 2 2
2 5
1 3 3
Appropriate Not Enough
Appropriate
for Particular Information to
for All Groups
Groups Determine
Is the approach appropriate for use with all
2 5 1
social risk factor groups?
Applicable to Applicable to Not Enough
Multiple One Program Information to
Programs Only Determine
Is the approach applicable only to a specific
VBP or reporting program, or can it be 2 6
applied more broadly?
Not Enough
Yes No Information to
Determine
Does the approach capture granular
5 1 2
subgroups where possible?
Somewhat Somewhat
Very Likely Very Unlikely
Likely Unlikely
How likely is it that incorporating this
approach into a VBP or reporting program
5 1 2
would result in a noticeable improvement in
health equity?
NOTE: Values are the number of experts who gave a particular rating. Model response is shown in bold.
CMS OMH Mapping Medicare Disparities Tool
TEP members’ ratings of this approach are shown in Table 7.4. A majority of members
(five) fully agreed that this approach is evidence-based, but there was considerable
uncertainty about whether the approach is designed to incentivize achievement or
improvement for at-risk beneficiaries, with three members saying that the approach does
not meet this criterion. There was also considerable uncertainty about whether the
approach guards against unintended consequences of worsening access or resources for at-
44
45
risk beneficiaries, with three saying that the approach does not meet this criterion, two
saying that it partially meets this criterion, and three saying that there is not enough
information to tell. A majority of members (five) said that the approach is unable to reliably
distinguish performance among providers. Most members (five) saw the approach as being
applicable to particular social risk factor groups, but some (three members) saw it as more
broadly applicable. Members were divided in their opinion of the applicability to VBP or
reporting programs, with three saying that it is applicable to multiple programs, three
saying that there is not enough information to decide, and two saying that it is applicable to
one program only (without specifying which program). Six members said that this
approach would be either somewhat or very unlikely to result in a noticeable improvement
in health equity if incorporated into a VBP or reporting program.
Several TEP members commented that this approach is not likely to incentivize
achievement or improvement for at-risk beneficiaries as it is currently designed, citing
both its descriptive purpose (i.e., lack of statistical comparisons) and focus on comparing
performance across geographic areas rather than providers. The majority opinion was that
significant work would need to be done to convert the approach into an equity quality
metric and that issues of risk adjustment (beyond age), sample size, and ability to reliably
discriminate performance across providers would need to be addressed. One member
commented that exclusion of the MA population, due to lack of necessary data, is a
significant limitation of the tool. During the discussion, it was noted that CMS is considering
incorporating other programs’ data sources into to the MMD Tool, which would increase
the scope but not address the main limitations of the tool as seen by the TEP.

Table 7.4. TEP Ratings of CMS OMH Mapping Medicare Disparities Tool
Not Enough
Meets Partially Meets Does Not Meet
Criterion Information to
Criterion Criterion Criterion
Determine
Is the approach based on available evidence
of the relationship between the social risk 5 2 1
factor and outcome?
Is the approach designed to incentivize
achievement or improvement for at-risk 1 3 3 1
beneficiaries?
Does the approach guard against
unintended consequences for at-risk 2 3 3
beneficiaries?
Is the approach able to reliably distinguish
1 1 5 1
performance between providers?
Appropriate Not Enough
Appropriate
for Particular Information to
for All Groups
Groups Determine
Is the approach appropriate for use with all
5 3
social risk factor groups?
Applicable to Applicable to Not Enough
Multiple One Program Information to
Programs Only Determine
Is the approach applicable only to a specific
VBP or reporting program or can it be 3 2 3
applied more broadly?
Not Enough
Yes No Information to
Determine
Does the approach capture granular
2 3 3
subgroups where possible?
Somewhat Somewhat
Very Likely Very Unlikely
Likely Unlikely
How likely is it that incorporating this
approach into a VBP or reporting program
2 3 3
would result in a noticeable improvement in
health equity?
NOTE: Values are the number of experts who gave a particular rating. Model response is shown in bold.
CMS OMH Reporting of CAHPS and HEDIS Data, Stratified by Race and
Ethnicity, for Medicare Beneficiaries
TEP members’ ratings of this approach are shown in Table 7.5. Six members fully agreed
that this approach is evidence-based, while two said that it partially meets this criterion.
Nearly all (seven) either fully or partially agreed that the approach is designed to
incentivize achievement or improvement for at-risk beneficiaries. There was, however,
46
47
considerable uncertainty about whether the approach guards against unintended
consequences of worsening access or resources for at-risk beneficiaries, with four
members saying that there is not enough information to decide and two saying that the
approach does not meet this criterion. Six members either fully or partially agreed that the
approach is able to reliably distinguish performance among providers. Four members said
the approach is applicable to all social risk factor groups, and half said it is applicable to
particular groups. Six members said that the approach is applicable to multiple VBP or
reporting programs, while two said that there is not enough information to decide. A
majority of members (five) said that this approach would be either somewhat or very likely
to result in a noticeable improvement in health equity if incorporated into a VBP or
reporting program, but two members said that it would be very unlikely to have such an
effect.
One TEP member commented that this was among the stronger approaches in the set
identified, and another said that this was the most robust approach in attending to
adequacy of sample size and reliability of scores for making between-provider
comparisons. One member commented that, in its current form, this approach is best suited
for incentivizing improvement via public reporting (its current use) and that additional risk
adjustment might be needed before payment could be fairly tied to performance. A couple
of members pointed out that some of the measures used in this approach are collected via
survey and mentioned that there are limitations to this mode of data collection, e.g., low
response rates and sample sizes and the possibility of recall bias. Relatedly, a couple of
members suggested that this approach could be improved by incorporating outcome
measures, e.g., by supplementing the current set of measures with encounter data. Several
members observed that many MA and PDP contracts are unmeasurable for at least some
racial and ethnic minority groups and measures. One member suggested that more years of
data could be pooled to gain insight into performance for smaller populations, such as
American Indians and Alaska Natives and Asian and Latino subgroups.

Table 7.5. TEP Ratings of CMS OMH Reporting of CAHPS and HEDIS Data Stratified by Race and
Ethnicity for Medicare Beneficiaries
Not Enough
Meets Partially Meets Does Not Meet
Criterion Information to
Criterion Criterion Criterion
Determine
Is the approach based on available evidence
of the relationship between the social risk
factor and outcome?
6 2
Is the approach designed to incentivize
achievement or improvement for at-risk
beneficiaries?
4 3 1
Does the approach guard against
unintended consequences for at-risk
beneficiaries?
2 2 4
Is the approach able to reliably distinguish
performance between providers?
4 2 1 1
Appropriate
for Particular
Groups
Appropriate
for All Groups
Not Enough
Information to
Determine
Is the approach appropriate for use with all
social risk factor groups?
4 4
Applicable to
Multiple
Programs
Applicable to
One Program
Only
Not Enough
Information to
Determine
Is the approach applicable only to a specific
VBP or reporting program, or can it be
applied more broadly?
6 2
Yes No
Not Enough
Information to
Determine
Does the approach capture granular
subgroups where possible?
3 3 2
Very Likely
Somewhat
Likely
Somewhat
Unlikely
Very Unlikely
How likely is it that incorporating this
approach into a VBP or reporting program
would result in a noticeable improvement in
health equity?
1 4 1 2
NOTE: Values are the number of experts who gave a particular rating. Model response is shown in bold.
Minnesota Healthcare Disparities Report
TEP members’ ratings of this approach are shown in Table 7.6. Six members fully agreed
that this approach is evidence-based, while two said that it partially meets this criterion.
Nearly all (seven) fully agreed that the approach is designed to incentivize achievement or
improvement for at-risk beneficiaries. A majority (five) felt that there was not enough
information to determine whether the approach guards against unintended consequences
of worsening access or resources for at-risk beneficiaries, though three members said that
48
49
the approach either fully or partially meets this criterion. Six members either fully or
partially agreed that the approach is able to reliably distinguish performance among
providers. A majority of members (five) said the approach is applicable to particular social
risk factor groups, and the remainder said it is applicable to all groups. Nearly all (seven)
said that the approach is applicable to multiple VBP or reporting programs. All members
said that this approach would be either somewhat or very likely to result in a noticeable
improvement in health equity if incorporated into a VBP or reporting program.
Several members commented that this approach uses a thoughtfully chosen group of
measures focused on processes and outcomes of care for specific, common conditions. One
member highlighted the focus on disparities by language and country of origin as a
particularly strong feature. Two members commented that some of the measures could be
strongly influenced by social determinants of health and that there should be further
consideration given to risk adjustment; although this concern was raised in the context of
this approach, it may be applicable to other approaches involving similar measures. Three
members expressed concern that insufficient attention had been given to the sample size
required for reliable provider-based measurement and that each measure should have
undergone testing to determine the sample size needed for reliability of 0.70 or higher.
Most members, though, felt that this approach was a strong building block for a more
broadly applicable approach, with one member commenting specifically about the benefit
of anchoring disparities to the overall state average rather than the performance of a
predetermined group.

Table 7.6. TEP Ratings of Minnesota Healthcare Disparities Report
Not Enough
Meets Partially Meets Does Not Meet
Criterion Information to
Criterion Criterion Criterion
Determine
Is the approach based on available evidence
of the relationship between the social risk 6
factor and outcome?
Is the approach designed to incentivize
achievement or improvement for at-risk 7
beneficiaries?
Does the approach guard against
unintended consequences for at-risk 1
beneficiaries?
Is the approach able to reliably distinguish
1
performance between providers?
2
1
2 5
5 1 1
Appropriate Not Enough
Appropriate
for Particular Information to
for All Groups
Groups Determine
Is the approach appropriate for use with all
5 3
social risk factor groups?
Applicable to Applicable to Not Enough
Multiple One Program Information to
Programs Only Determine
Is the approach applicable only to a specific
VBP or reporting program, or can it be 7 1
applied more broadly?
Not Enough
Yes No Information to
Determine
Does the approach capture granular
3 1 4
subgroups where possible?
Somewhat Somewhat
Very Likely Very Unlikely
Likely Unlikely
How likely is it that incorporating this
approach into a VBP or reporting program
1 7
would result in a noticeable improvement in
health equity?
NOTE: Values are the number of experts who gave a particular rating. Model response is shown in bold.
CMS Assessment of Hospital Disparities for Dual-Eligible Patients
TEP members’ ratings of this approach are shown in Table 7.7. All members either fully or
partially agreed that this approach is evidence-based and that it is designed to incentivize
achievement or improvement for at-risk beneficiaries. Members were divided about
whether the approach guards against unintended consequences of worsening access or
resources for at-risk beneficiaries, with four saying that it fully or partially meets this
50
51
criterion, two saying that it does not meet this criterion, and two saying that there is not
enough information to judge. Nearly all (seven) either fully or partially agreed that the
approach is able to reliably distinguish performance among providers. Four members said
the approach is applicable to all social risk factor groups, while three said it is applicable to
particular groups (citing dual-eligible beneficiaries as the applicable group). Four members
felt that the approach is applicable to multiple VBP or reporting programs, while three
members felt that it was applicable to one program only. Members were divided in their
judgment of the likelihood that this approach would result in a noticeable improvement in
health equity if incorporated into a VBP or reporting program: One member said that such
a result is very likely, four said somewhat likely, and three said somewhat unlikely.
A couple of TEP members commented about the narrowness of this assessment, but both
conceded that the approach seems broadly applicable to social risk factor groups and
measures and so could be extended in those ways to increase impact. It was also noted that
the within-hospital component of this approach does not distinguish the direction of
differences. This could create a scenario in which worsening care for dual-eligible patients
(or other at-risk patients if this approach were to be extended to other groups) results in a
higher score on the measure (and an incentive if the approach were linked to an incentive
scheme). A couple of TEP members also commented that there is insufficient evidence that
having just 12 patients in each group for a within-plan comparison can result in a
meaningfully informative estimate. One member commented that with such small samples,
even large inequities are likely to lead to a null finding, which is potentially misleading.
Finally, almost all TEP members preferred an approach in which additional casemix
adjustment for contextual factors such as housing and food instability were incorporated.

Table 7.7. TEP Ratings of CMS Assessment of Hospital Disparities for Dual-Eligible Patients
Not Enough
Meets Partially Meets Does Not Meet
Criterion Information to
Criterion Criterion Criterion
Determine
Is the approach based on available evidence
of the relationship between the social risk 6
factor and outcome?
Is the approach designed to incentivize
achievement or improvement for at-risk 5
beneficiaries?
Does the approach guard against
unintended consequences for at-risk 3
beneficiaries?
Is the approach able to reliably distinguish
1
performance between providers?
2
3
1 2 2
6 1
Appropriate Not Enough
Appropriate
for Particular Information to
for All Groups
Groups Determine
Is the approach appropriate for use with all
3 4 1
social risk factor groups?
Applicable to Applicable to Not Enough
Multiple One Program Information to
Programs Only Determine
Is the approach applicable only to a specific
VBP or reporting program, or can it be 4 3 1
applied more broadly?
Not Enough
Yes No Information to
Determine
Does the approach capture granular
1 3 4
subgroups where possible?
Somewhat Somewhat
Very Likely Very Unlikely
Likely Unlikely
How likely is it that incorporating this
approach into a VBP or reporting program
1 4 3
would result in a noticeable improvement in
health equity?
NOTE: Values are the number of experts who gave a particular rating. Model response is shown in bold.
CMS OMH Health Equity Summary Score
TEP members’ ratings of this approach are shown in Table 7.8. Nearly all members (seven)
fully agreed that this approach is evidence-based and that it is designed to incentivize
achievement or improvement for at-risk beneficiaries. Nearly all (seven) either fully or
partially agreed that the approach guards against unintended consequences of worsening
access or resources for at-risk beneficiaries, with one member specifically commenting that
the HESS is built to incentivize rather than penalize providers. Again, nearly all members
(seven) fully agreed that the approach is able to reliably distinguish performance among
52
53
providers. Four members said the approach is applicable to particular social risk factor
groups, and four said it is applicable to all groups, with one member commenting that the
HESS was explicitly designed to be able to add other social risk factors as more information
about their relationship to quality becomes available. Nearly all members (seven) said that
the approach is applicable to multiple VBP or reporting programs. All members said that
this approach would be either somewhat or very likely to result in a noticeable
improvement in health equity if incorporated into a VBP or reporting program.
Two members commented that, unlike other measures, the HESS is precisely suited for
inclusion in VBP programs, increasing the likelihood that it would have an impact on
equity. Three members specifically commented that it is among the better approaches
identified, particularly given its joint consideration of cross-sectional performance and
improvement in performance. One member highlighted its focus on patient experience and
clinical quality measures as a positive feature, another highlighted its careful attention to
reliability and the sample size required to achieve it (though one member commented that
the strict reliability standards might not allow for including small subgroups in reporting),
and yet another commented that data collection burden is not an issue because this is a
secondary use of the data summarized by the metric. The consensus opinion was that this
is a sound summary measure of health equity that produces information that is actionable
and important.

Table 7.8. TEP Ratings of CMS OMH Health Equity Summary Score
Criterion
Meets
Criterion
Partially Meets
Criterion
Does Not Meet
Criterion
Not Enough
Information to
Determine
Is the approach based on available evidence
of the relationship between the social risk
factor and outcome?
7 1
Is the approach designed to incentivize
achievement or improvement for at-risk
beneficiaries?
7 1
Does the approach guard against
unintended consequences for at-risk
beneficiaries?
3 4 1
Is the approach able to reliably distinguish
performance between providers?
7 1
Appropriate
for Particular
Groups
Appropriate
for All Groups
Not Enough
Information to
Determine
Is the approach appropriate for use with all
social risk factor groups?
4 4
Applicable to
Multiple
Programs
Applicable to
One Program
Only
Not Enough
Information to
Determine
Is the approach applicable only to a specific
VBP or reporting program, or can it be
applied more broadly?
7 1
Yes No
Not enough
information to
determine
Does the approach capture granular
subgroups where possible?
3 2 3
Very Likely
Somewhat
Likely
Somewhat
Unlikely
Very Unlikely
How likely is it that incorporating this
approach into a VBP or reporting program
would result in a noticeable improvement in
health equity?
2 6
NOTE: Values are the number of experts who gave a particular rating. Model response is shown in bold.
Zimmerman Health-Related Quality of Life Approach to Assessing Health
Equity
TEP members’ ratings of this approach are shown in Table 7.9. All members either fully or
partially agreed that this approach is evidence-based. Members were divided about
whether the approach is designed to incentivize achievement or improvement for at-risk
beneficiaries, with four saying that it fully or partially meets this criterion, two saying that
it does not meet this criterion, and two saying that there is not enough information to
judge. Four members said that this approach does not guard against unintended
54
55
consequences of worsening access or resources for at-risk beneficiaries, and three said that
there is not enough information to make this determination. Four members said that the
approach is not able to reliably distinguish performance among providers, and two said
that there is not enough information to make this determination. A majority of members
(five) said the approach is applicable to all social risk factor groups, while two said it is
applicable to particular groups. Though two members said that the approach is applicable
to multiple VBP or reporting programs, six said there was not enough information to make
this determination. A majority of members (five) said that it was somewhat or very
unlikely that this approach would result in a noticeable improvement in health equity if
incorporated into a VBP or reporting program.
The consensus opinion was that this is an interesting approach for describing full
population equity issues, but a lot of work would be required to adapt this approach for
incorporation into a VBP or quality reporting program, and there are potential barriers to
making such an adaptation. Several members raised concerns about the measures that are
summarized by this approach, citing evidence that different racial and ethnic groups use
the self-rated health scale differently and that some minority groups have lower
expectations about overall health. Members also raised concerns about the use of White
men as the reference group. Although White men are a standard for privilege, they do not
represent optimal health on many measures. Using White men as the reference group for
calculating this measure thus sets a low bar for assessing equity. A couple of TEP members
pointed out that the approach depends on collecting or having available the Behavioral
Risk Factor Surveillance Survey measures on which the measure is based and that there
would be significant logistical challenges to ensuring consistent data quality and
completeness if one were to collect these data from patients or plan members. A couple of
members also commented that the required sample size for making accurate comparisons
using this approach is unknown, as is the time frame in which one might expect meaningful
changes in this score as a result of organizational changes. Finally, one member pointed out
that there is a potentially serious patient-mix issue to address, in that an organization could
score well on this metric simply by serving a large proportion of patients who are counted
among the disadvantaged but for whom disparities relative to high-income White males are
small.

Table 7.9. TEP Ratings of Zimmerman Health-Related Quality of Life Approach to Assessing
Health Equity
Not Enough
Meets Partially Meets Does Not Meet
Criterion Information to
Criterion Criterion Criterion
Determine
Is the approach based on available evidence
of the relationship between the social risk 6
factor and outcome?
Is the approach designed to incentivize
achievement or improvement for at-risk 2
beneficiaries?
Does the approach guard against
unintended consequences for at-risk 1
beneficiaries?
Is the approach able to reliably distinguish
2
performance between providers?
2
2 2 2
4 3
4 2
Appropriate Not Enough
Appropriate
for Particular Information to
for All Groups
Groups Determine
Is the approach appropriate for use with all
2 5 1
social risk factor groups?
Applicable to Applicable to Not Enough
Multiple One Program Information to
Programs Only Determine
Is the approach applicable only to a specific
VBP or reporting program, or can it be 2 6
applied more broadly?
Not Enough
Yes No Information to
Determine
Does the approach capture granular
3 2 3
subgroups where possible?
Somewhat Somewhat
Very Likely Very Unlikely
Likely Unlikely
How likely is it that incorporating this
approach into a VBP or reporting program
1 2 3 2
would result in a noticeable improvement in
health equity?
NOTE: Values are the number of experts who gave a particular rating. Model response is shown in bold.
Zimmerman and Anderson Approach to Evaluating Trends over Time in
Health Equity
TEP members’ ratings of this approach are shown in Table 7.10. All members either fully or
partially agreed that this approach is evidence-based. Members were divided about
56
57
whether the approach is designed to incentivize achievement or improvement for at-risk
beneficiaries, with four saying that it fully or partially meets this criterion, two saying that
it does not meet this criterion, and two saying that there is not enough information to
judge. Four members said that there was not enough information to determine whether
this approach guards against unintended consequences of worsening access or resources
for at-risk beneficiaries, and two said that the approach does not satisfy this criterion. The
majority of members (five) said either that the approach is unable to distinguish
performance among providers or that there is not enough information to tell. Members
were divided about the applicability of this approach to different social risk factor groups,
with two saying that it is appropriate for particular groups, three saying that it is
appropriate to all groups, and three saying that there is not enough information to tell.
Though two members said that the approach is applicable to multiple VBP or reporting
programs, six said there was not enough information to make this determination. A
majority of members (five) said that it was somewhat or very unlikely that this approach
would result in a noticeable improvement in health equity if incorporated into a VBP or
reporting program.
All of the same critiques that were applied to the Zimmerman (2019) approach were raised
about this approach. One member commented that the focus on change over time is
advantageous in that it provides potential to reward an organization for improving the
health of a currently disadvantaged group. One member commented that the distinction
made between health disparities, inequality, and justice is unusual and unhelpful, while
another commented that a measure that simply compares care for Black and White
patients is limited in that it pegs the care of Black patients to that of White patients.

Table 7.10. TEP Ratings of Zimmerman and Anderson Approach to Evaluating Trends over Time in
Health Equity
Not Enough
Meets Partially Meets Does Not Meet
Criterion Information to
Criterion Criterion Criterion
Determine
Is the approach based on available evidence
of the relationship between the social risk 5
factor and outcome?
Is the approach designed to incentivize
achievement or improvement for at-risk 2
beneficiaries?
Does the approach guard against
unintended consequences for at-risk 1
beneficiaries?
Is the approach able to reliably distinguish
1
performance between providers?
3
2 2 2
1 2 4
1 3 3
Appropriate Not Enough
Appropriate
for Particular Information to
for All Groups
Groups Determine
Is the approach appropriate for use with all
2 3 3
social risk factor groups?
Applicable to Applicable to Not Enough
Multiple One Program Information to
Programs Only Determine
Is the approach applicable only to a specific
VBP or reporting program, or can it be 2 6
applied more broadly?
Not Enough
Yes No Information to
Determine
Does the approach capture granular
1 3 4
subgroups where possible?
Somewhat Somewhat
Very Likely Very Unlikely
Likely Unlikely
How likely is it that incorporating this
approach into a VBP or reporting program
1 2 2 3
would result in a noticeable improvement in
health equity?
NOTE: Values are the number of experts who gave a particular rating. Model response is shown in bold.
58

59
8. Summary and Key Takeaways
Summary
The objectives of this project were to search for existing health equity measurement
approaches and consider their suitability for inclusion in Medicare’s VBP programs, quality
reporting efforts, and confidential reports as a way to incentivize health equity. A formal
definition of a health&equity&measurement&approach was developed to guide the search:
an approach to illustrating or summarizing the extent to which the quality of health care
provided by an organization contributes to reducing disparities in health and health care at
the population level for those patients with greater social risk factor burden by improving
the care and health of those patients.
Ten such approaches were identified and evaluated by a panel of experts on social risk
factors, health disparities, health equity, risk adjustment, value-based and alternative
payment models, and Medicare’s VBP programs. These ten approaches, which generated
varying levels of enthusiasm among the panel, fit within three broad categories of
approaches: (1) approaches focused on determining which existing quality measures are
suitable for health equity comparisons (i.e., permit reliable and valid comparisons among
social risk factor groups) or for measuring organizational structures, systems, and
processes hypothesized to promote the delivery of high-quality care for all; (2) approaches
that engaged in particular kinds of comparisons of measures (not necessarily statistical
comparisons), on a measure-by-measure basis, between groups of patients with greater
versus lesser social risk factor burden; and (3) approaches that developed a system for
combining different dimensions of health equity into a single summary index.
This project also identified a set of guidelines for health equity measurement. A
health equity measurement approach should, ideally,
• be based on measures on which disparities in care are known to exist for certain
populations or that address health care disparities and culturally appropriate care
• reflect available evidence bearing on the relationship between a social risk factor
and health or health care outcome
• be designed to incentivize achievement or improvement for at-risk beneficiaries,
including having a valid and appropriate benchmark and/or reference group if
comparisons to benchmarks and/or reference groups are made
• include design features that guard against unintended consequences of worsening
quality or access or disincentivizing resources for any beneficiaries, including the at-
risk beneficiaries who are the focus of health equity measurement
• establish measurability requirements that ensure the ability to make reliable
distinctions between health care providers in their performance in the domain of
health equity
• capture information about small subgroups, where possible, while limiting the
influence of imprecise estimates of provider performance.
In the case of a summary index, the measure should also
60
• summarize information in a way that is psychometrically sound
• allow for disaggregation of information to permit easy identification of quality
improvement targets.
Key Takeaways
The ten approaches that the TEP evaluated were judged to meet these requirements to
widely varying degrees. Of approaches focused on measure identification (Category 1), the
NQF Disparities-Sensitive Measure Assessment was viewed most favorably by the TEP.
Using a set of carefully established criteria and an easy-to-understand point system, this
approach identified 32 NQF-endorsed measures as disparities-sensitive. Although
considerable work would be needed to determine whether and how these measures could
be linked to social risk data and whether and how valid comparisons could be made, this
approach was viewed as a valuable initial step toward measuring health equity and
disparities in health care quality. It is potentially applicable to any Medicare VBP or quality
reporting program that collects one or more of the 32 disparities-sensitive measures.
Furthermore, there may be the potential to enhance the favored approaches to be
described next by incorporating one or more of the disparities-sensitive measures
identified by this NQF approach.
Of approaches focused on measure-by-measure comparisons (Category 2), the approach
underlying the Minnesota&Healthcare&Disparities&Report was judged most favorably by
the TEP. The perceived advantages of this approach include its thoughtfully chosen group
of measures, incorporation of multiple important social risk factors, ability to reliably
distinguish performance among providers, clear focus on incentivizing achievement for at-
risk beneficiaries, and choice to anchor disparities to the overall state average rather than
the performance of a predetermined group. Although some additional work would be
needed to transfer this approach to a broader setting, including making careful
considerations about sample sizes required for accurate comparisons and determining the
availability of data on social risk factors, the method itself is readily applicable to all
Medicare VBP and quality reporting programs.
Of approaches focused on summary indices (Category 3), the CMS OMH HESS was judged
most favorably by the TEP. The perceived advantages of this approach include its joint
consideration of cross-sectional performance and improvement in performance, focus on
patient experience and clinical quality, careful attention to reliability and the sample size
required to achieve it, direct applicability to certain VBP and quality reporting programs,
and transferability to other programs. CMS OMH has designed a dashboard to provide
confidential HESS data to MA contracts, though that dashboard has not yet been fully
implemented. Scores on this metric could easily be incorporated into the Medicare Plan
Finder and the MA Quality Star Ratings Program if doing so aligned with CMS’s strategic
priorities. This approach also could easily be extended to other social risk factors and
measures, and there are plans to test the feasibility of extending this approach to settings
beyond MA.
Of the ten approaches evaluated, the HESS received the highest ratings from the TEP
overall. Given the high ratings it received, the HESS may be closest to meeting the full scope
of goals outlined by ASPE for incorporating a measure of health equity into a Medicare VBP
or quality reporting program. If HHS were to move forward with this approach, it could
61
consider possible refinements to the approach based on the practices established by the
NQF Disparities-Sensitive Measure Assessment and the Minnesota Healthcare Disparities
Report and the guidelines for health equity measurement outlined by the TEP. Several of
the measures that are included in the HESS are among the 76 measures identified as
disparities-sensitive by NQF. It might be possible to include in the HESS additional
measures from the set identified by NQF, provided that the measures are collected for MA
plans and meet the reliability and sample size requirements established for the HESS. The
analyses that underlie the Minnesota Disparities Report are similar to the analyses that
underlie the cross-sectional component of the HESS. In the Minnesota Healthcare
Disparities Report, plan performance by patients’ preferred language and country of origin
are considered in addition to race and ethnicity. Information on country of origin is not
available for Medicare Advantage beneficiaries, but information about Spanish preference
is available. Thus, Spanish preference could be considered as a possible third social risk
factor for the HESS.

62
Appendix A. Ambulatory, Hospital, Behavioral Health, and Public
Health Measures Identified as Part of the Measurement
Framework for Evaluating How Well an Organization Meets
National CLAS Standards (HHS OMH)
Ambulatory Care Measures
CAHPS Cultural Competence Item Set
CAHPS Clinician/Group Survey
Disparities-Sensitive or CLAS-Salient Measures
Controlling High Blood Pressure
Hemoglobin A1c Poor Control
Uncontrolled Diabetes Admission Rate
Diabetes Short-Term Complications Admission Rate
Hospital Measures
Hospital CAHPS Survey
Hospital CAHPS Survey Health Literacy Item Set
Cultural Competency Assessment Tool for Hospitals
Joint Commission Standards for Hospital Accreditation and Elements of Performance
Joint Commission 2016 Measure List for Accreditation Chart-Abstracted Process Measures
Disparities-Sensitive or CLAS-Salient Measures
30-Day, All-Cause, Risk-Standardized Readmission Rate Following Pneumonia Hospitalization
Median Time to ECG for Acute Myocardial Infarction or Chest Pain Patients
30-Day, All-Cause, Risk-Standardized Readmission Rate Following Coronary Artery Bypass Graft Surgery
Risk-Adjusted Deep Sternal Wound Infection
Behavioral Health Measures
Experience of Care and Health Outcomes (ECHO) Survey
Disparities-Sensitive or CLAS-Salient Measures
Alcohol Screening and Follow-Up for People With Serious Mental Illness
Initiation and Engagement of Alcohol and Other Drug Dependence Treatment
Antidepressant Medication Management
30-Day All-cause Unplanned Readmission Following Psychiatric Hospitalization In An Inpatient Psychiatric
Facility
Public Health Measures
Developing a Self-Assessment Tool for CLAS in Local Public Health Agencies
CAHPS Clinician/Group Survey

63
Disparities-Sensitive or CLAS-Salient Measures
Flu Vaccinations for Adults Ages 18 and Older
Asthma Emergency Department Visits
Depression Screening, Adolescents 18 Years of Age
Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention

64
Appendix B. Measures Identified as Disparities-Sensitive
According to the NQF Disparities-Sensitive Measure Assessment
Measures Identified Through First-Tier Review
Perinatal Care
Exclusive Breast Milk Feeding
Cesarean Section
Pediatric Care
Developmental Screening by 2 Years of Age
Children Who Received Preventive Dental Care
Children Who Receive Family-Centered Care
Children Who Receive Effective Care Coordination of Healthcare Services When Needed
Children With Special Health Care Needs Who Receive Services Needed for Transition to Adult Care
Children With Inconsistent Health Insurance Coverage in the Past 12 Months
Children Who Have Inadequate Insurance Coverage for Optimal Health
Children Who Attend Schools Perceived as Safe
Children Who Live in Communities Perceived as Safe
Utilization/Appropriateness of Use
Relative Resource Use for People with Asthma
Relative Resource Use for People with COPD
Relative Resource Use for People with Diabetes
Relative Resource Use for People with Cardiovascular Conditions
Asthma Emergency Department Visits
Prostate Cancer: Avoidance of Overuse Measure—Bone Scan for Staging Low-Risk Patients
Screening and Prevention
Cervical Cancer Screening
Preventive Care and Screening: Body Mass Index Screening and Follow-Up
Depression Screening by 13 Years of Age
Depression Screening by 18 Years of Age
Pneumonia Vaccination Status for Older Adults
Pneumococcal Immunization (PPV 23)
High Risk for Pneumococcal Disease—Pneumococcal Vaccination
Pneumococcal Vaccination of Nursing Home/Skilled Nursing Facility Residents
Pneumococcal Polysaccharide Vaccine Ever Received (Home Health)
Influenza Immunization: Outpatient
Influenza Immunization: Inpatient
Flu Shots for Adults Ages 50 and Over
Influenza Vaccination of Nursing Home/Skilled Nursing Facility Residents
65
Percentage of LTC Residents Assessed and Appropriately Given the Seasonal Influenza Vaccine
Diabetes Care
Hemoglobin A1c Testing
Hemoglobin A1c Control (<8.0%)
Hemoglobin A1c Poor Control (>9.0%)
Diabetes and Elevated HbA1C—Use of Diabetes Medications
Adults Taking Insulin with Evidence of Self-Monitoring Blood Glucose Testing
Patients Who Had a Serum Creatinine in Past 12 Reported Months
Diabetic Foot and Ankle Care, Peripheral Neuropathy—Neurological Evaluation
Diabetic Foot Care and Patient Education Implemented
Diabetes Mellitus and Medication Possession Ratio for Chronic Medications
Cardiovascular Care
Controlling High Blood Pressure
Coronary Artery Disease and Medication Possession Ratio for Statin Therapy
Fibrinolytic Therapy Received Within 30 Minutes of Hospital Arrival
Median Time to ECG for Acute Myocardial Infarction (AMI) or Chest Pain Patients
Heart Failure: ACE Inhibitor or ARB Therapy for Left Ventricular Systolic Dysfunction
30-Day, All-Cause, Risk-Standardized Mortality Rate Following AMI Hospitalization for Adult Patients
Survival Predictor for Abdominal Aortic Aneurysm
Atrial Fibrillation—Warfarin Therapy
Deep Vein Thrombosis Anticoagulation >= 3 Months
Adherence to Statin Treatment for Hyperlipidemia
Proportion of Patients with Hypercalcemia
Cancer Care
Oncology: Cancer Stage Documented
Prostate Cancer: Adjuvant Hormonal Therapy for High-Risk Patients
Risk-Adjusted Morbidity and Mortality for Esophagectomy for Cancer
Multiple Myeloma—Treatment with Bisphosphonates
Hospice and Palliative Care
Proportion of Patients Who Died from Cancer Not Admitted to Hospice
Hospice and Palliative Care—Treatment Preferences
Hospice and Palliative Care—Pain Screening
Hospice and Palliative Care—Pain Assessment
Rehabilitation/Restorative Care
Physical Therapy or Rehabilitation/Restorative Care for Long-Stay Patients with New Balance Problem

66
Measures Identified Through Second-Tier Review (Communication/Care Coordination)
Clinician/Group Health Literacy Practices Based on CAHPS Item Set for Addressing Health Literacy
Clinician/Group’s Cultural Competence Based on the CAHPS Cultural Competence Item Set
Patients Receiving Language Services Supported by Qualified Language Services Providers
Screening for Preferred Spoken Language for Health Care
Experience of Care and Health Outcomes (ECHO) Survey
Advance Care Plan
Reconciled Medication List Received by Discharged Patients
Transition Record with Specified Elements Received by Discharged Patients (Discharges from an Inpatient Facility
to Home/Self Care or Any Other Site of Care)
Transition Record with Specified Elements Received by Discharged Patients (Emergency Department Discharges
to Ambulatory Care [Home/Self Care] or Home Health Care)
Timely Transmission of Transition Record (Discharges from an Inpatient Facility to Home/Self Care or Any Other
Site of Care)
Proportion of Cancer Patients Admitted to the ICU in the Last 30 Days of Life
Percentage of Hospice Patients with Documentation of a Discussion of Spiritual/Religious Concerns or
Documentation That the Patient/Caregiver Did Not Want to Discuss
Diabetes Short-Term Complications Admission Rate (PQI 1)
Diabetes Long-Term Complications Admission Rate (PQI 3)
Uncontrolled Diabetes Admission Rate (PQI 14)
Rate of Lower-Extremity Amputation Among Patients with Diabetes (PQI 16)

67
Appendix C. Biographical Information on Expert Panelists
Arlene Ash, Ph.D., is Professor and Division Chief of Biostatistics and Health Services
Research in the Department of Population and Quantitative Health Sciences at the
University of Massachusetts Medical School. She is an elected fellow of the American
Statistical Association, the American Association for the Advancement of Science, and the
International Statistical Institute. Dr. Ash pioneered tools for using administrative data to
monitor and manage health care delivery systems, including those now widely used by the
Medicare program and the Department of Health and Human Services. In 1996, she
cofounded DxCG (now part of Cotiviti, Inc.) to promote “fair and efficient health care”
through predictive software. In 2008, Dr. Ash’s risk-based predictive modeling work was
honored by AcademyHealth with its Health Services Research Impact Award. Since 2014,
she has worked with MassHealth (Massachusetts’ Medicaid and Children’s Health
Insurance Program) to develop risk models that account for both medical and social risk
factors when predicting health care utilization and costs. Her more than 200 research
publications reflect long-standing interests in women’s health; gender, age and racial
disparities; and quality, equity and efficiency in health care financing and delivery. She has
also used her statistical expertise to advance gender equity in pay and to improve the
integrity of U.S. elections.
Kevin Fiscella, MD, MPH, is Dean’s Professor of Family Medicine at the University of
Rochester Medical Center. He has worked part-time in federally qualified health centers for
more than 37 years as a family physician, addiction medicine physician, and Human
Immunovirus physician. He is also a health services researcher with more than 250 peer-
reviewed publications largely related to socioeconomic status, race, health, health care, and
equity. Over the past decade, his research has focused on implementation research to
identify pragmatic strategies for promoting health equity through randomized trials.
Examples include community health workers for navigation of patients with cancer,
practice-based outreach strategies to reduce disparities in cancer screening, use of
electronic health record data for interventions and for primary outcomes assessment, peer-
led patient activation trainings for low-income and minority people living with HIV, and
use of academic detailing of clinicians and patient-centered peer coaching to promote
uptake of atherosclerotic cardiovascular disease prevention among low-income and
minority patients. Dr. Fiscella also has two decades of national committee experience
related to measuring and reporting on health disparities and promotion of health, including
two Institutes of Medicine committees, co-chairing two NQF advisory committees—
measures for disparities/cultural and linguistic competency and SES-risk adjustment of
quality measures. He currently represents the American Society of Addiction Medicine on
the Board of the National Commission on Correctional Health Care (that accredits
correctional health care), where he chairs the policy and research committee. He is a
current member of the Disparities Monitoring Committee for NQF and a former member of
the technical Advisory Panel on SES and Blood Pressure for the National Committee for
Quality Assurance and former associate medical director for the local provider
performance system for the New York State Delivery System Reform Incentive Program.

68
Darrell J. Gaskin, Ph.D., MS, is the William C. and Nancy F. Richardson Professor in Health
Policy and Director of the Hopkins Center for Health Disparities Solutions at the Johns
Hopkins Bloomberg School of Public Health in the Department of Health Policy and
Management. Dr. Gaskin is a health services researcher and health economist. He is an
internationally recognized expert in health and health care disparities. He seeks to identify
and understand place-based barriers to care for low-income, minority, and other
vulnerable populations; to develop and promote policies and practices that address the
social determinants of health to improve access to care, quality of care, and health care
outcomes; and to promote equity in well-being, health, and health care by race, ethnicity,
socioeconomic status, and geography. He serves on the Board of Scientific Counselors of the
National Center for Health Statistics of the Centers for Disease Control and Prevention. He
chairs the National Advisory Committee of the Robert Wood Johnson Foundation’s System
for Action program. Also, he serves on the Board of Directors of AcademyHealth and the
American Society of Health Economists. He is a 2019 recipient of the Presidential Early
Career Award for Scientists and Engineers. Dr. Gaskin has a Ph.D. in public health
economics from the Johns Hopkins University. He holds an MS degree in economics from
the Massachusetts Institute of Technology, and a BA degree in economics from Brandeis
University.
Romana Hasnain-Wynia, MS, Ph.D., is the Chief Research Officer at Denver Health, where
she oversees Denver Health’s research and sponsored programs through the Office of
Research and represents research interests as a member of the Executive Leadership Team.
She also actively mentors junior investigators at Denver Health and the University of
Colorado, Anschutz Medical Campus. Prior to joining Denver Health, Dr. Hasnain-Wynia
served as the director of the Addressing Disparities program at the Patient Centered
Outcomes Research Institute (PCORI), where she was responsible for providing strategic
oversight and leadership for the program’s funding priorities. Prior to PCORI, she was the
director of the Center for Health Care Equity and Associate Professor at Northwestern
University Feinberg School of Medicine. She spent a decade at the American Hospital
Association’s Health Research and Educational Trust, where she was Vice President of
Research. She has been the principal investigator for a number of national studies focusing
on advancing equity in health care with an emphasis on developing and integrating equity
measurement in health systems. She uses mixed methods approaches in her research and
has expertise in designing pragmatic trials in “real world settings.” She is a member of
NQF’s Disparities Standing Committee and serves as the Chair of the Board for the Colorado
Health Institute and is a member of the editorial boards of the journals Health Affairs and
Health Services Research.
Sinsi Hernández-Cancio, JD, is a vice president at the National Partnership for Women
and Families, where she leads the Health Justice team. She is a national health and health
care equity policy and advocacy thought leader with 25 years of experience advancing
equal opportunity for women and families of color, and almost 20 years advocating for
increased health care access and improved quality of care for underserved communities.
Sinsi is deeply committed to transforming our health care system to meet the needs of our
rapidly evolving nation so we can all thrive together. She believes that our future
prosperity depends on ensuring that our health care system routinely provides excellent,
comprehensive, culturally centered, and affordable care for every single person, family, and
community, and that this requires the dismantling of structural inequities including racism,

69
sexism, ableism, homophobia, transphobia, xenophobia, and religious bigotry. Sinsi is a
recognized leader in the national health equity movement, a sought-after strategic advisor,
and a dynamic, inspiring speaker. She has presented at national events across the country
and served on numerous advisory committees for organizations including the National
Academy of Medicine, the National Committee for Quality Assurance, the Patient Centered
Outcomes Research Institute, the Robert Wood Johnson Foundation, the National Center
for Complex Health and Social Needs, and the American Association of Pediatrics. She has
published extensively and has appeared in national- and state-level English and Spanish
television, radio, and print media. Her extensive experience in health and health equity
policy and advocacy spans the state government, labor, and nonprofit arenas. Prior to
joining the National Partnership’s staff, she was the founding director of Families USA’s
Center on Health Equity Action for System Transformation, where she led efforts to
advance health equity and reduce disparities in health outcomes and health care access and
quality by leveraging health care and delivery system transformation to reduce persistent
racial, ethnic, and geographic health inequities with an intersectional lens. Prior to that, she
advised and represented two governors of Puerto Rico on federal health and human
services policies, and she worked for the Service Employees International Union as a senior
health policy analyst and national campaign coordinator for their Healthcare Equality
Project campaign to enact the Affordable Care Act. She earned an AB from Princeton
University’s Woodrow Wilson School of Public and International Affairs and a JD from New
York University School of Law, where she was an Arthur Garfield Hays Civil Liberties
Fellow, and won the Georgetown Women’s Law and Public Policy Fellowship.
Cara James, Ph.D., is President and CEO at Grantmakers In Health (GIH). Prior to joining
GIH, she served as Director of the Office of Minority Health at CMS, where she provided
leadership, vision, and direction to advance the HHS and CMS goals related to reducing
disparities and achieving health equity for vulnerable populations, including racial and
ethnic populations, persons with disabilities, sexual and gender minorities, and persons
living in rural communities. Under her guidance, CMS developed its first CMS Equity Plan to
Improve Quality in Medicare and its first Rural Health Strategy, created an ongoing
initiative to help individuals understand their coverage and connect to care, increased the
collection and reporting of demographic data, and developed numerous resources to help
stakeholders in their efforts to reduce disparities. Before joining CMS, Dr. James served as
Director of the Disparities Policy Project and Director of the Barbara Jordan Health Policy
Scholars Program at the Henry J. Kaiser Family Foundation, where she was responsible for
addressing a broad array of health and access to care issues for people of color and other
underserved populations, including the potential impact of the Affordable Care Act,
analyses of state-level disparities in health and access to care, and disparities in access to
care among individuals living in health professional shortage areas. Prior to joining the
foundation, she worked at Harvard University and the Picker Institute. Dr. James is a past
member of the National Academies of Sciences, Engineering and Medicine’s (NASEM)
Health and Medicine Roundtable on the Promotion of Health Equity and has served on
several NASEM committees. She has published a number of peer-reviewed articles. Dr.
James holds her doctorate in health policy and her bachelor’s degree in psychology from
Harvard University.
Ninez Ponce, MPP, Ph.D. (BS University of California Berkeley; MPP Harvard; Ph.D.
University of California Los Angeles [UCLA]), is Professor in the UCLA Fielding School of

70
Public Health and Director of its Center for Health Policy Research. She leads the California
Health Interview Survey (CHIS), the nation’s largest state health survey, recognized as a
national model for data collection on race/ethnicity, sexual orientation and gender identity,
and immigrant health. She is a health services researcher most interested in reducing
transaction costs levied on consumers and providers that produce racial/ethnic disparities.
Her research on health disparities focuses on developing multicultural survey measures,
implementing population-based health surveys in diverse populations, and examining the
intersection of social factors and health policy. In 2019, Dr. Ponce and the CHIS team
received the AcademyHealth Impact award for her contributions to population health
measurement to inform public policies.
Dana Gelb Safran, Sc.D., was most recently Head of Measurement for Haven, the health
care venture formed by Amazon, Berkshire Hathaway, and JPMorgan Chase (ABJ) to
improve health care experiences and costs through transforming health care delivery and
financing. In that role, Dr. Safran was a member of the executive leadership team and
responsible for the company’s data strategy, for guiding the development of a robust
analytics infrastructure, and for applying data, analytics, and measurement to optimize the
venture’s success. Prior to her position at Haven, Dr. Safran was Chief Performance
Measurement and Improvement Officer at Blue Cross Blue Shield of Massachusetts
(BCBSMA). As an architect of the BCBSMA Alternative Quality Contract (AQC) and the
leader responsible for its unique use of behavioral economics and payer-provider
collaboration to reduce cost while improving quality, Dr. Safran is widely recognized as
having contributed to the national push toward value-based payment. Prior to joining
BCBSMA, she led a research institute at Tufts University School of Medicine dedicated to
developing patient-reported measures of health and health care quality. She remains on the
faculty at Tufts and serves on a number of state and national advisory bodies related to
health care quality and affordability. Since 2017, Dr. Safran has served as a Commissioner
on the Medicare Payment Advisory Commission (MedPAC). She earned her Master and
Doctor of Science degrees from the Harvard School of Public Health.
