
Botulinum Toxins A and B
Page 1 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
UnitedHealthcare
®
Commercial
Medical Benefit Drug Policy
Botulinum Toxins A and B
Policy Number: 2024D0017AK
Effective Date: April 1, 2024
Instructions for Use
Table of Contents Page
Coverage Rationale ....................................................................... 1
Applicable Codes .......................................................................... 3
Background.................................................................................. 11
Benefit Considerations ................................................................ 11
Clinical Evidence ......................................................................... 11
U.S. Food and Drug Administration ........................................... 21
References ................................................................................... 22
Policy History/Revision Information ........................................... 27
Instructions for Use ..................................................................... 27
Coverage Rationale
See Benefit Considerations
This policy refers to the following botulinum toxin types A and B:
Dysport
®
(abobotulinumtoxinA)
Daxxify
®
(daxibotulinumtoxinA-lanm)
Xeomin
®
(incobotulinumtoxinA)
Botox
®
(onabotulinumtoxinA)
Myobloc
®
(rimabotulinumtoxinB)
General Requirements (applicable to all requests)
All of the following:
o Diagnosis; and
o Botulinum toxin administration is no more frequent than every 12 weeks, regardless of diagnosis; and
o One of the following:
Prescriber attests dosing is in accordance with the United States Food and Drug Administration (FDA) approved
labeling; or
For indications without FDA approved dosing, prescriber attests there is published clinical evidence to support the
dosing
Diagnosis-Specific Requirements
The information below indicates additional requirements for those indications having specific criteria in the list of proven
indications.
Dysport (abobotulinumtoxinA) is proven in the treatment of the following conditions:
Achalasia
81
Anal fissures, chronic
7,8,81
Blepharospasm associated with dystonia
10,81
Cervical dystonia (also known as spasmodic torticollis)
10,19,81,83,84
Related Commercial Policies
• Occipital Nerve Injections and Ablation (Including
Occipital Neuralgia and Headache)
• Treatment of Temporomandibular Joint Disorders
Community Plan Policy
• Botulinum Toxins A and B

Botulinum Toxins A and B
Page 2 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Detrusor overactivity (also known as detrusor hyperreflexia) or detrusor-sphincter dyssynergia due to spinal cord
injury or disease
15,17,18,53,54,63,81
Hand dystonia (writer's, musician’s, or typist's cramp)
19,81,83
Hand tremor
19,81
Hemifacial spasm (seventh cranial nerve disorders)
19,81
Hyperhidrosis
1,15,81
including gustatory sweating (Frey's Syndrome)
9,15,38
Oromandibular dystonia
Sialorrhea
15,57,81
Spasmodic dysphonia (laryngeal dystonia)
3,19
Spasticity associated with:
1,6,39,81
o Cerebral palsy
o Multiple sclerosis
o Neuromyelitis optica (NMO)
o Stroke
o Other injury, disease, or tumor of the brain or spinal cord
Strabismus
1,19,81
Tongue dystonia
Torsion dystonia
Voice tremor
4
Daxxify (daxibotulinumtoxinA-lanm) is proven in the treatment of the following condition:
Cervical dystonia (also known as spasmodic torticollis)
102
Xeomin (incobotulinumtoxinA) is proven in the treatment of the following conditions:
Blepharospasm associated with dystonia
70,76
Cervical dystonia (spasmodic torticollis)
70,76,83-4
Sialorrhea
70
Spasticity associated with:
65-6,70,76
o Cerebral palsy
o Multiple sclerosis
o Neuromyelitis optica (NMO)
o Stroke
o Other injury, disease, or tumor of the brain or spinal cord
Botox (onabotulinumtoxinA) is proven in the treatment of the following conditions:
Achalasia
80
Anal fissures, chronic
8,80
Blepharospasm associated with dystonia
1,19,80
Cervical dystonia (also known as spasmodic torticollis)
1,10,80,83-4
Detrusor overactivity (also known as detrusor hyperreflexia) or detrusor-sphincter dyssynergia due to spinal cord
injury or disease
15,17,18,53,54,63,80
Hand dystonia (writer's, musician’s, or typist's cramp)
19,80,83
Hand tremor
19,80
Hemifacial spasm (seventh cranial nerve disorders)
19,80
Hyperhidrosis
1,80
including gustatory sweating (Frey's Syndrome)
9,15,38
Migraine headache, chronic
Botox is proven for the prophylaxis of chronic migraine when the following criterion is met:
o Diagnosis of chronic migraine defined by all of the following
1,71,80
:
Greater than or equal to 15 headache days per month
Greater than or equal to 8 migraine days per month
Headaches last 4 hours per day or longer
Oromandibular dystonia
Overactive bladder
1,80
Sialorrhea
15,57,80

Botulinum Toxins A and B
Page 3 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Spasmodic dysphonia (laryngeal dystonia)
3-5,19,80
Spasticity associated with:
1,6,39,80
o Cerebral palsy
o Multiple sclerosis
o Neuromyelitis optica (NMO)
o Stroke
o Other injury, disease, or tumor of the brain or spinal cord
Strabismus
1,19,80
Tongue dystonia
80
Torsion dystonia
80
Voice tremor
4
Myobloc (rimabotulinumtoxinB) is proven in the treatment of the following conditions:
Cervical dystonia (also known as spasmodic torticollis)
2,83-84
Detrusor overactivity (also known as detrusor hyperreflexia)
15,18
Sialorrhea
15,56-7
Spasticity associated with:
89
o Cerebral palsy
o Multiple sclerosis
o Neuromyelitis optica (NMO)
o Stroke
o Other injury, disease, or tumor of the brain or spinal cord
Unproven
Daxxify, Dysport, Myobloc, and Xeomin are unproven and not medically necessary for the treatment of chronic migraine
headache.
14,15,24,25-6,64,75,81
Botox, Daxxify, Dysport, Myobloc, and Xeomin are unproven and not medically necessary for the treatment of the
following conditions:
Acquired nystagmus
Anismus (pelvic floor dyssynergia)
16
Benign prostatic hyperplasia
13,18,33,68,80,81
Brachial plexus palsy
46,80,81
Chronic daily headache
15,36,80,81
Chronic low back pain
36,80
Chronic prostatic pain
18
Cricopharyngeal dysphagia
20-23
Epiphora following salivary gland transplantation
Esophageal spasm
37
Gastroparesis (including diabetic gastroparesis)
58-62, 80,90-91
Gustatory epiphora (Crocodile tears)
Head tremor
Lateral epicondylitis (tennis elbow)
51,52
Lichen simplex
Lower urinary tract (voiding) dysfunction
11,18
Motor tics
Myofascial pain syndrome
45,72,81
Nasal hypersecretion
50,67
Pain and/or wound healing after hemorrhoidectomy
Pancreas divisum
Pelvic floor spasticity (and associated pain conditions)
18
Piriformis syndrome
49
Post-parotidectomy sialoceles
Post-thoracotomy pseudoangina
Proctalgia fugax
18
Severe bruxism
41-42
Severe paradoxical vocal cord movement
40
Sphincter of Oddi dysfunction
12
Stiff-person syndrome
Temporomandibular disorders
43-44,48
Tension headache
15,27,78
Thyroid associated ophthalmopathy
47
Tourette's syndrome
55
Traumatic sixth nerve palsy
Trigeminal neuralgia
32,73-4
Trismus and stridor in amyotrophic lateral sclerosis
Applicable Codes
The following list(s) of procedure and/or diagnosis codes is provided for reference purposes only and may not be all inclusive.
Listing of a code in this policy does not imply that the service described by the code is a covered or non-covered health service.
Benefit coverage for health services is determined by the member specific benefit plan document and applicable laws that may

Botulinum Toxins A and B
Page 4 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
require coverage for a specific service. The inclusion of a code does not imply any right to reimbursement or guarantee claim
payment. Other Policies and Guidelines may apply.
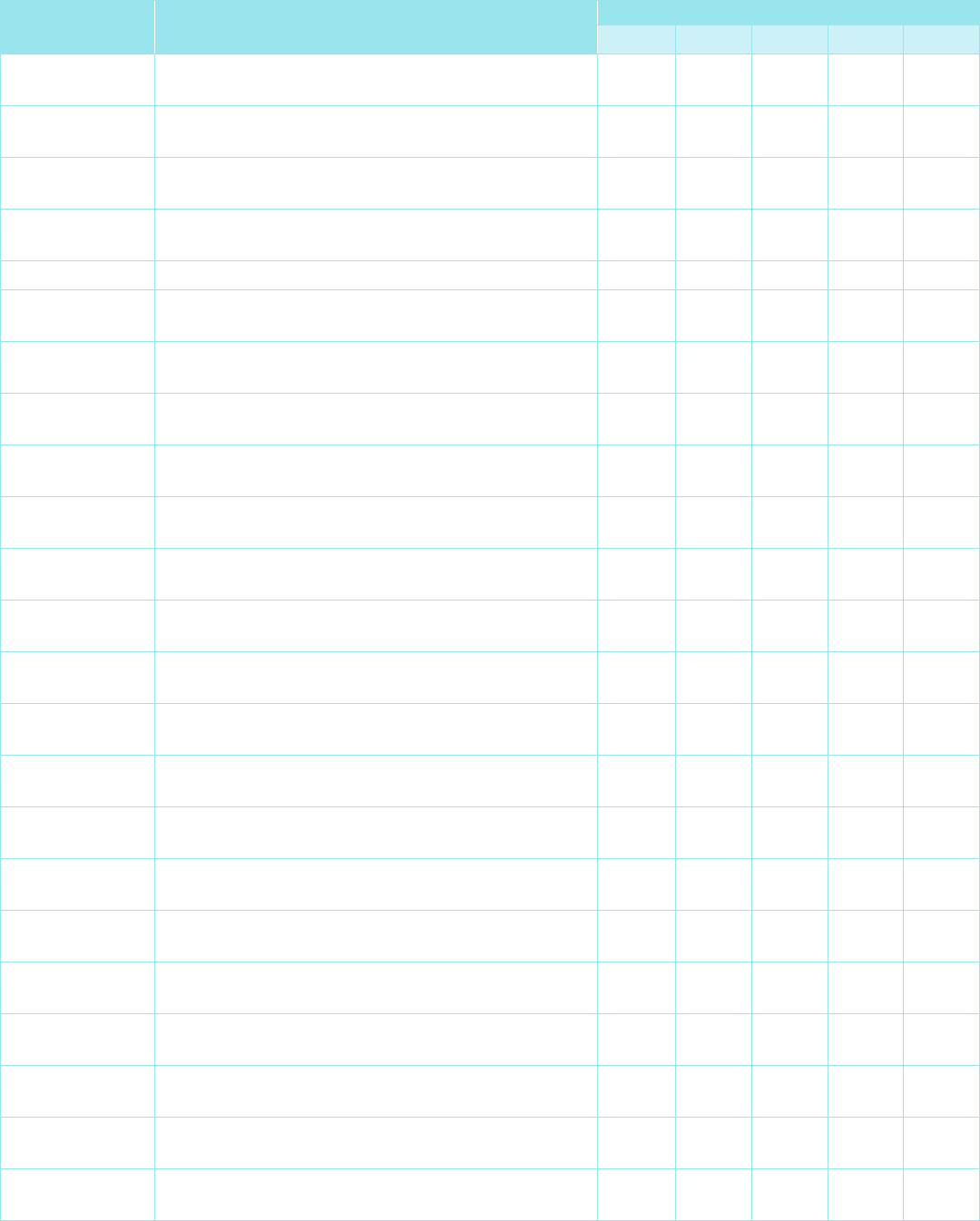
HCPCS Code
Description
Brand Name
J0585 Injection, onabotulinumtoxinA, 1 unit Botox
J0586 Injection, abobotulinumtoxinA, 5 units Dysport
J0587 Injection, rimabotulinumtoxinB, 100 units Myobloc
J0588 Injection, incobotulinumtoxinA, 1 unit Xeomin
J0589 Injection, daxibotulinumtoxina-lanm, 1 unit Daxxify
Diagnosis Code Description
Applies to HCPCS Code
J0585 J0586 J0587 J0588 J0589
C71.0 Malignant neoplasm of cerebrum, except lobes and
ventricles
X X X X
C71.1 Malignant neoplasm of frontal lobe X X X X
C71.2 Malignant neoplasm of temporal lobe X X X X
C71.3 Malignant neoplasm of parietal lobe X X X X
C71.4 Malignant neoplasm of occipital lobe X X X X
C71.5 Malignant neoplasm of cerebral ventricle X X X X
C71.6 Malignant neoplasm of cerebellum X X X X
C71.7 Malignant neoplasm of brain stem X X X X
C71.8 Malignant neoplasm of overlapping sites of brain X X X X
C71.9 Malignant neoplasm of brain, unspecified X X X X
C72.0 Malignant neoplasm of spinal cord X X X X
D33.0 Benign neoplasm of brain, supratentorial X X X X
D33.1 Benign neoplasm of brain, infratentorial X X X X
D33.2 Benign neoplasm of brain, unspecified X X X X
D33.4 Benign neoplasm of spinal cord X X X X
D43.0 Neoplasm of uncertain behavior of brain,
supratentorial
X X X X
D43.1 Neoplasm of uncertain behavior of brain, infratentorial X X X X
D43.2 Neoplasm of uncertain behavior of brain, unspecified X X X X
D43.4 Neoplasm of uncertain behavior of spinal cord X X X X
D49.6 Neoplasm of unspecified behavior of brain X X X X
G04.1 Tropical spastic paraplegia X X X X
G11.4 Hereditary spastic paraplegia X X X X
G24.09 Other drug induced dystonia X X
G24.1 Genetic torsion dystonia X X
G24.2 Idiopathic nonfamilial dystonia X X
G24.3 Spasmodic torticollis X X X X X
G24.4 Idiopathic orofacial dystonia X X
G24.5 Blepharospasm X X X
G24.8 Other dystonia X X
G24.9 Dystonia, unspecified X X

Botulinum Toxins A and B
Page 5 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Diagnosis Code Description
Applies to HCPCS Code
J0585 J0586 J0587 J0588 J0589
G25.89
Other specified extrapyramidal and movement
disorders
X X
G35 Multiple sclerosis X X X X
G36.0 Neuromyelitis optica X X X X
G43.701 Chronic migraine without aura, not intractable, with
status migrainosus
X
G43.709 Chronic migraine without aura, not intractable, without
status migrainosus
X
G43.711 Chronic migraine without aura, intractable, with status
migrainosus
X
G43.719 Chronic migraine without aura, intractable, without
status migrainosus
X
G43.E01 Chronic migraine with aura, not intractable, with status
migrainosus
X
G43.E09 Chronic migraine with aura, not intractable, without
status migrainosus
X
G43.E11 Chronic migraine with aura, intractable, with status
migrainosus
X
G43.E19 Chronic migraine with aura, intractable, without status
migrainosus
X
G51.0 Palsy (spasm) of conjugate gaze X X
G51.1 Geniculate ganglionitis X X
G51.2 Melkersson's syndrome X X
G51.31 Clonic hemifacial spasm, right X X
G51.32 Clonic hemifacial spasm, left X X
G51.33 Clonic hemifacial spasm, bilateral X X
G51.39 Clonic hemifacial spasm, unspecified X X
G51.4 Facial myokymia X X
G51.8 Other disorders of facial nerve X X
G51.9 Disorder of facial nerve, unspecified X X
G80.0 Spastic quadriplegic cerebral palsy X X X X
G80.1 Spastic diplegic cerebral palsy X X X X
G80.2 Spastic hemiplegic cerebral palsy X X X X
G80.3 Athetoid cerebral palsy X X X X
G80.4 Ataxic cerebral palsy X X X X
G80.8 Other cerebral palsy X X X X
G80.9 Cerebral palsy, unspecified X X X X
G81.10 Spastic hemiplegia affecting unspecified side X X X X
G81.11 Spastic hemiplegia affecting right dominant side X X X X
G81.12 Spastic hemiplegia affecting left dominant side X X X X
G81.13 Spastic hemiplegia affecting right nondominant side X X X X
G81.14 Spastic hemiplegia affecting left nondominant side X X X X
G83.4 Cauda equina syndrome X X X

Botulinum Toxins A and B
Page 6 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Diagnosis Code Description
Applies to HCPCS Code
J0585 J0586 J0587 J0588 J0589
H50.89 Other specified strabismus X X
H51.0 Palsy (spasm) of conjugate gaze X X
I60.10 Nontraumatic subarachnoid hemorrhage from
unspecified middle cerebral artery
X X X X
I60.11 Nontraumatic subarachnoid hemorrhage from right
middle cerebral artery
X X X X
I60.12 Nontraumatic subarachnoid hemorrhage from left
middle cerebral artery
X X X X
I61.0 Nontraumatic intracerebral hemorrhage in
hemisphere, subcortical
X X X X
I61.1 Nontraumatic intracerebral hemorrhage in
hemisphere, cortical
X X X X
I61.2 Nontraumatic intracerebral hemorrhage in
hemisphere, unspecified
X X X X
I61.3 Nontraumatic intracerebral hemorrhage in brain stem X X X X
I61.4 Nontraumatic intracerebral hemorrhage in cerebellum X X X X
I61.5 Nontraumatic intracerebral hemorrhage,
intraventricular
X X X X
I61.6
Nontraumatic intracerebral hemorrhage, multiple
localized
X X X X
I61.8 Other nontraumatic intracerebral hemorrhage X X X X
I61.9 Nontraumatic intracerebral hemorrhage, unspecified X X X X
I63.00
Cerebral infarction due to thrombosis of unspecified
precerebral artery
X X X X
I63.011 Cerebral infarction due to thrombosis of right vertebral
artery
X X X X
I63.012
Cerebral infarction due to thrombosis of left vertebral
artery
X X X X
I63.013 Cerebral infarction due to thrombosis of bilateral
vertebral arteries
X X X X
I63.019
Cerebral infarction due to thrombosis of unspecified
vertebral artery
X X X X
I63.02 Cerebral infarction due to thrombosis of basilar artery X X X X
I63.031
Cerebral infarction due to thrombosis of right carotid
artery
X X X X
I63.032 Cerebral infarction due to thrombosis of left carotid
artery
X X X X
I63.033
Cerebral infarction due to thrombosis of bilateral
carotid arteries
X X X X
I63.039 Cerebral infarction due to thrombosis of unspecified
carotid artery
X X X X
I63.09
Cerebral infarction due to thrombosis of other
precerebral artery
X X X X
I63.10 Cerebral infarction due to embolism of unspecified
precerebral artery
X X X X
Botulinum Toxins A and B
Page 7 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Diagnosis Code Description
Applies to HCPCS Code
J0585 J0586 J0587 J0588 J0589
I63.111
Cerebral infarction due to embolism of right vertebral
artery
X X X X
I63.112 Cerebral infarction due to embolism of left vertebral
artery
X X X X
I63.113
Cerebral infarction due to embolism of bilateral
vertebral arteries
X X X X
I63.119 Cerebral infarction due to embolism of unspecified
vertebral artery
X X X X
I63.12 Cerebral infarction due to embolism of basilar artery X X X X
I63.131 Cerebral infarction due to embolism of right carotid
artery
X X X X
I63.132
Cerebral infarction due to embolism of left carotid
artery
X X X X
I63.133 Cerebral infarction due to embolism of bilateral carotid
arteries
X X X X
I63.139
Cerebral infarction due to embolism of unspecified
carotid artery
X X X X
I63.19 Cerebral infarction due to embolism of other
precerebral artery
X X X X
I63.20
Cerebral infarction due to unspecified occlusion or
stenosis of unspecified precerebral arteries
X X X X
I63.211 Cerebral infarction due to unspecified occlusion or
stenosis of right vertebral artery
X X X X
I63.212
Cerebral infarction due to unspecified occlusion or
stenosis of left vertebral artery
X X X X
I63.213 Cerebral infarction due to unspecified occlusion or
stenosis of bilateral vertebral arteries
X X X X
I63.219
Cerebral infarction due to unspecified occlusion or
stenosis of unspecified vertebral artery
X X X X
I63.22 Cerebral infarction due to unspecified occlusion or
stenosis of basilar artery
X X X X
I63.231
Cerebral infarction due to unspecified occlusion or
stenosis of right carotid arteries
X X X X
I63.232 Cerebral infarction due to unspecified occlusion or
stenosis of left carotid arteries
X X X X
I63.233
Cerebral infarction due to unspecified occlusion or
stenosis of bilateral carotid arteries
X X X X
I63.239 Cerebral infarction due to unspecified occlusion or
stenosis of unspecified carotid artery
X X X X
I63.29
Cerebral infarction due to unspecified occlusion or
stenosis of other precerebral arteries
X X X X
I63.30 Cerebral infarction due to thrombosis of unspecified
cerebral artery
X X X X
I63.311
Cerebral infarction due to thrombosis of right middle
cerebral artery
X X X X

Botulinum Toxins A and B
Page 8 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Diagnosis Code Description
Applies to HCPCS Code
J0585 J0586 J0587 J0588 J0589
I63.312
Cerebral infarction due to thrombosis of left middle
cerebral artery
X X X X
I63.313 Cerebral infarction due to thrombosis of bilateral
middle cerebral arteries
X X X X
I63.319
Cerebral infarction due to thrombosis of unspecified
middle cerebral artery
X X X X
I63.321 Cerebral infarction due to thrombosis of right anterior
cerebral artery
X X X X
I63.322
Cerebral infarction due to thrombosis of left anterior
cerebral artery
X X X X
I63.323 Cerebral infarction due to thrombosis of bilateral
anterior cerebral arteries
X X X X
I63.329
Cerebral infarction due to thrombosis of unspecified
anterior cerebral artery
X X X X
I63.331 Cerebral infarction due to thrombosis of right posterior
cerebral artery
X X X X
I63.332
Cerebral infarction due to thrombosis of left posterior
cerebral artery
X X X X
I63.333 Cerebral infarction due to thrombosis of bilateral
posterior cerebral arteries
X X X X
I63.339
Cerebral infarction due to thrombosis of unspecified
posterior cerebral artery
X X X X
I63.341 Cerebral infarction due to thrombosis of right
cerebellar artery
X X X X
I63.342
Cerebral infarction due to thrombosis of left cerebellar
artery
X X X X
I63.343 Cerebral infarction due to thrombosis of bilateral
cerebellar arteries
X X X X
I63.349
Cerebral infarction due to thrombosis of unspecified
cerebellar artery
X X X X
I63.39 Cerebral infarction due to thrombosis of other cerebral
artery
X X X X
I63.40
Cerebral infarction due to embolism of unspecified
cerebral artery
X X X X
I63.411 Cerebral infarction due to embolism of right middle
cerebral artery
X X X X
I63.412
Cerebral infarction due to embolism of left middle
cerebral artery
X X X X
I63.413 Cerebral infarction due to embolism of bilateral middle
cerebral arteries
X X X X
I63.419
Cerebral infarction due to embolism of unspecified
middle cerebral artery
X X X X
I63.421 Cerebral infarction due to embolism of right anterior
cerebral artery
X X X X
I63.422
Cerebral infarction due to embolism of left anterior
cerebral artery
X X X X

Botulinum Toxins A and B
Page 9 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Diagnosis Code Description
Applies to HCPCS Code
J0585 J0586 J0587 J0588 J0589
I63.423
Cerebral infarction due to embolism of bilateral
anterior cerebral arteries
X X X X
I63.429 Cerebral infarction due to embolism of unspecified
anterior cerebral artery
X X X X
I63.431
Cerebral infarction due to embolism of right posterior
cerebral artery
X X X X
I63.432 Cerebral infarction due to embolism of left posterior
cerebral artery
X X X X
I63.433
Cerebral infarction due to embolism of bilateral
posterior cerebral arteries
X X X X
I63.439 Cerebral infarction due to embolism of unspecified
posterior cerebral artery
X X X X
I63.441
Cerebral infarction due to embolism of right cerebellar
artery
X X X X
I63.442 Cerebral infarction due to embolism of left cerebellar
artery
X X X X
I63.443
Cerebral infarction due to embolism of bilateral
cerebellar arteries
X X X X
I63.449 Cerebral infarction due to embolism of unspecified
cerebellar artery
X X X X
I63.49
Cerebral infarction due to embolism of other cerebral
artery
X X X X
I63.50 Cerebral infarction due to unspecified occlusion or
stenosis of unspecified cerebral artery
X X X X
I63.511
Cerebral infarction due to unspecified occlusion or
stenosis of right middle cerebral artery
X X X X
I63.512 Cerebral infarction due to unspecified occlusion or
stenosis of left middle cerebral artery
X X X X
I63.513
Cerebral infarction due to unspecified occlusion or
stenosis of bilateral middle cerebral arteries
X X X X
I63.519 Cerebral infarction due to unspecified occlusion or
stenosis of unspecified middle cerebral artery
X X X X
I63.521
Cerebral infarction due to unspecified occlusion or
stenosis of right anterior cerebral artery
X X X X
I63.522 Cerebral infarction due to unspecified occlusion or
stenosis of left anterior cerebral artery
X X X X
I63.523
Cerebral infarction due to unspecified occlusion or
stenosis of bilateral anterior cerebral arteries
X X X X
I63.529 Cerebral infarction due to unspecified occlusion or
stenosis of unspecified anterior cerebral artery
X X X X
I63.531
Cerebral infarction due to unspecified occlusion or
stenosis of right posterior cerebral artery
X X X X
I63.532 Cerebral infarction due to unspecified occlusion or
stenosis of left posterior cerebral artery
X X X X
I63.533
Cerebral infarction due to unspecified occlusion or
stenosis of bilateral posterior cerebral arteries
X X X X

Botulinum Toxins A and B
Page 10 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Diagnosis Code Description
Applies to HCPCS Code
J0585 J0586 J0587 J0588 J0589
I63.539
Cerebral infarction due to unspecified occlusion or
stenosis of unspecified posterior cerebral artery
X X X X
I63.541 Cerebral infarction due to unspecified occlusion or
stenosis of right cerebellar artery
X X X X
I63.542
Cerebral infarction due to unspecified occlusion or
stenosis of left cerebellar artery
X X X X
I63.543 Cerebral infarction due to unspecified occlusion or
stenosis of bilateral cerebellar arteries
X X X X
I63.549
Cerebral infarction due to unspecified occlusion or
stenosis of unspecified cerebellar artery
X X X X
I63.59 Cerebral infarction due to unspecified occlusion or
stenosis of other cerebral artery
X X X X
I63.6
Cerebral infarction due to cerebral venous thrombosis,
nonpyogenic
X X X X
I63.81 Other cerebral infarction due to occlusion or stenosis
of small artery
X X X X
I63.89 Other cerebral infarction X X X X
I63.9 Cerebral infarction, unspecified X X X X
J38.5 Laryngeal spasm X X
K11.7 Disturbances of salivary secretion X X X X
K22.0 Achalasia of cardia X X
K60.1 Chronic anal fissure X X
K60.2 Anal fissure, unspecified X X
L74.510 Primary focal hyperhidrosis, axilla X X
L74.511 Primary focal hyperhidrosis, face X X
L74.512 Primary focal hyperhidrosis, palms X X
L74.513 Primary focal hyperhidrosis, soles X X
L74.519 Primary focal hyperhidrosis, unspecified X X
L74.52 Secondary focal hyperhidrosis X X
N31.0 Uninhibited neuropathic bladder, not elsewhere
classified
X X X
N31.1 Reflex neuropathic bladder, not elsewhere classified X X X
N31.9 Neuromuscular dysfunction of bladder, unspecified X X X
N32.81 Overactive bladder X
N36.44 Muscular disorders of urethra X X X
N39.41 Urge incontinence X
N39.46 Mixed incontinence X
R13.3 Dysphagia, pharyngeal phase X X
R25.0 Abnormal head movements X X
R25.1 Tremor, unspecified X X
R25.2 Cramp and spasm X X
R25.3 Fasciculation X X
R25.8 Other abnormal involuntary movements X X

Botulinum Toxins A and B
Page 11 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Diagnosis Code Description
Applies to HCPCS Code
J0585 J0586 J0587 J0588 J0589
R25.9 Unspecified abnormal involuntary movements X X
R29.891 Ocular torticollis X X X X
R49.0 Dysphonia X X
R49.9 Unspecified voice and resonance disorder X X
R61 Generalized hyperhidrosis X X
Background
There are seven serologically distinct forms of botulinum toxin, A through G. All seven neurotoxins share a common structure
consisting of one heavy chain and one light chain. They all inhibit acetylcholine release at the neuromuscular junction via the
enzymatic inactivation of a protein that is required for the docking and fusion process involved in the release of acetylcholine.
Each neurotoxin works at a distinct site. Botulinum toxin type A cleaves the protein SNAP-25 and botulinum toxin type B
cleaves synaptobrevin, both of these proteins are part of a protein complex necessary for proper docking and fusion.
1,2,10,70
The potency units of botulinum toxins are specific to the preparation and assay method utilized. They are not interchangeable
and, therefore, the units of biological activity cannot be compared to nor converted into units of any other botulinum toxin
products assessed with any other specific assay method.
1,2,10,70
Benefit Considerations
Botulinum toxin type A and B are cosmetic when used to improve appearance, or in the absence of physiological functional
impairment that would be improved by their use. Most United Healthcare Certificates of Coverage (COCs) and Summary Plan
Descriptions (SPDs) exclude benefit coverage for cosmetic services. In addition, most Certificates of Coverage and many
Summary Plan Descriptions explicitly exclude benefit coverage for medical and surgical treatment of excessive sweating
(hyperhidrosis). The member specific benefit plan document must be reviewed to determine what benefits, if any, exist for
treatment of hyperhidrosis.
Some Certificates of Coverage allow for coverage of experimental/investigational/unproven treatments for life-threatening
illnesses when certain conditions are met. The member specific benefit plan document must be consulted to make coverage
decisions for this service. Some states mandate benefit coverage for off-label use of medications for some diagnoses or under
some circumstances when certain conditions are met. Where such mandates apply, they supersede language in the benefit
document or in the medical or drug policy. Benefit coverage for an otherwise unproven service for the treatment of serious rare
diseases may occur when certain conditions are met. Refer to the Policy and Procedure addressing the treatment of serious
rare diseases.
Clinical Evidence
Proven
Cervical Dystonia
In a randomized, double-blind, multicenter, non-inferiority, two-period crossover study, Yun et al compared the efficacy and
safety of Dysport and Botox at a 2.5:1 ratio in the treatment of cervical dystonia (CD).
14
The lower ratio than 3:1 was suggested
as a more appropriate conversion ratio, due to the higher efficacy of Botox and more frequent incidence of adverse effects in
CD and other focal movement disorders. Patients who were over 20 years old and have experienced CD for at least 18 months
were eligible, and were allowed to continue on a stable dose of medications for CD for the duration of the trial. Both products
were diluted so that the 2.5:1 ratio resulted in the same volume to be administered. The patients received either Dysport or
Botox, and were followed monthly for the first 16 weeks. After the 4-week washout period, each group was crossed over to
receive the other product, respectively. Patients were also followed up with monthly for 16 weeks in the second period. Results
from both periods were merged and compared according to the two different products. The primary efficacy outcome was the
change in the Tsui scale between the baseline value and that at 1 month after each injection (peak effect). One hundred and
Botulinum Toxins A and B
Page 12 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
two patients enrolled in the study. Patients were allocated 49 and 53 to two different arms of the trial. Arm 1 received Dysport
during the first phase and Botox during the crossover phase. Arm 2 received Botox during the first phase and Dysport during
the second phase. Only 94 of the 102 patients completed the entire study and were included in the final analysis. Mean
changes in the Tsui scale between baseline and 4 weeks after each injection trended to favor Botox, however, this was not
statistically significant (4.0 ±3.9 points Dysport vs. 4.8 ±4.1 points for Botox; 95% CI, -0.1-1.7; p = 0.091). The mean change of
the Toronto western spasmodic torticollis rating scale score, the proportion of improvement in clinical global impression and
patient global impression, and the incidences of adverse events were not significantly different between the two treatments.
The authors concluded that, in terms of efficacy and safety, Dysport at a ratio of 2.5:1 to Botox was not inferior to Botox in
patients with CD.
The efficacy of Daxxify was evaluated in a randomized, double-blind, placebo-controlled, multicenter trial in a total of 301
patients (NCT03608397).
102
At study baseline, 84% of patients had previously received a botulinum toxin as treatment for
cervical dystonia. Patients had a clinical diagnosis of cervical dystonia with baseline Toronto Western Spasmodic Torticollis
Rating Scale (TWSTRS) total score ≥ 20, TWSTRS severity score ≥ 15, TWSTRS disability score ≥ 3, and TWSTRS pain score
≥ 1. For patients who had previously received a botulinum toxin treatment for cervical dystonia, the trial required that ≥ 14
weeks had passed since the most recent botulinum toxin administration. Patients were randomized (3:3:1) to receive a single
administration of 2.5 mL of either Daxxify 125 Units (n = 125), Daxxify 250 Units (n = 130), or placebo (n = 46), divided amongst
the affected muscles as selected by the investigator. The primary efficacy endpoint was the mean change in the TWSTRS total
score from baseline averaged over weeks 4 and 6. TWSTRS evaluates the severity of dystonia, patient-perceived disability from
dystonia, and pain, with a range of possible scores from 0 to 85. The mean change from baseline in the total TWSTRS score
was significantly greater for both dosage groups of Daxxify than for placebo.
Detrusor Overactivity
In a prospective, long-term (3 year), multicenter, open-label extension study following a 52-week, phase III trial of
onabotulinumtoxinA, patients were treated on an “as needed” basis with intradetrusor onabotulinumtoxinA (200U or 300U) for
urinary incontinence (UI) due to neurogenic detrusor overactivity.
94
Patients received treatment ≥ 12 weeks since the previous
treatment and a UI episode threshold. The primary efficacy endpoint was the change from study baseline in UI episodes/day at
week 6 after each treatment. Additional efficacy measurements included: percent change in UI episodes, the proportions of
patients with ≥ 50% and 100% reductions from baseline in UI episodes/day, changes from baseline in volume/void and
Incontinence Quality of Life (I-QOL) total summary scores, IQOL responder rates (proportion of patients achieving a ≥ 11-point
increase from baseline in I-QOL total score, which is defined as the minimally important difference for I-QOL in NDO), and
duration of treatment effect (time to patient request for retreatment). OnabotulinumtoxinA 200U consistently reduced UI
episodes/day; reductions from baseline ranged from –3.2 to –4.1 across six treatments. Volume/void consistently increased,
nearly doubling after treatment. I-QOL improvements were consistently greater than twice the minimally important difference (+
11 points). Overall median duration of effect was 9.0 months (200U). Results were similar for onabotulinumtoxinA 300U. Most
common AEs were urinary tract infections and urinary retention. De novo CIC rates were 29.5, 3.4, and 6.0% (200U), and 43.0,
15.0, and 4.8% (300U) for treatments 1–3, respectively; de novo CIC rates were 0% for treatments 4–6. The authors concluded
that OnabotulinumtoxinA treatments consistently improve UI, volume/void, and QOL in patients with UI due to NDO in this 4-
year study, with no new safety signals.
Migraine Headache
OnabotulinumtoxinA is beneficial for the prophylaxis of chronic migraine headaches based upon FDA approval, published
practice guidelines, professional society evidence reviews, randomized controlled clinical trials, and smaller randomized
exploratory studies.
15,24,25-6
Aurora et al performed a secondary analysis of the data to assess patients who received all five treatment cycles and completed
the PREEMPT-1 and PREEMPT-2 trials. Both studies were 24 week double-blind, placebo controlled, parallel-group phase, with
a 32-week open-label phase, that evaluated the efficacy and safety of onabotulinumtoxinA (BoNT-A). Out of a total of 1,384 total
patients, 1,005 received all five treatment cycles and were included in the analysis. Of these, 513 received all 5 cycles with BTA,
whereas 492 underwent 2 cycles of placebo followed by 3 cycles of BoNT-A treatment. After 56 weeks of treatment, significant
between group differences were found favoring BoNT-A treatment vs. placebo, even after those receiving placebo switching to
BoNT-A. The following headache symptoms were evaluated: mean change in frequency of headache days (-12.0 vs -11.0, p =
0.035); total migraine days (-11.6 vs -10.7, p = 0.038), and moderate/severe headache days (-11.0 vs -10.1 n = 0.042). There
were also large mean improvements from baseline in the following measures: cumulative hours of headache on headache days,
Botulinum Toxins A and B
Page 13 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
frequency of headache episodes, percentage with severe Headache Impact Test (HIT)-6 scores, and total HIT-6 and Migraine-
Specific Quality of Life Questionnaire scores). The percent of patients with a ≥ 50% reduction from baseline in frequency of
headache days was significantly greater for the BoNT-A only group at week 56 (69.6% vs 62.8%, p = 0.023). Treatment-related
adverse event rates were 28.5% for the BoNT-A group vs. 12.4% for the placebo group during the double-blind phase of the
trials. The most frequently reported treatment related adverse events were neck pain (4.3%), muscular weakness (1.6%),
injection site pain (2.1%), and eyelid ptosis (1.9%). This data supports the use of onabotulinumtoxinA for the treatment of
migraine headaches.
In a follow up analysis of the PREEMPT clinical trials, Lipton et al., assessed the effects of treatment with onabotulinumtoxinA
on health-related quality of life (HRQoL) and headache impact in adults with chronic migraine.
28
In the PREEMPT trials,
Headache Impact Test (HIT)-6 scores were obtained at baseline and every 4 weeks. In terms of change in total HIT-6 scores, a
negative value reflects reduced headache impact and an improvement in the patient’s functionality. HRQoL was measured by
the Migraine-Specific Quality of Life Questionnaire (MSQ v2.1). This score was obtained at baseline and every 12 weeks. A
positive change in MSQ v2.1 scores reflects improvement in HRQoL during the PREEMPT study. An analysis of the combined
data looked at 688 subjects who received treatment with Botox vs. 696 who received saline placebo injections. Baseline mean
total HIT-6 and MSQ v2.1 scores were comparable between groups; 93.1% were severely impacted based on HIT-6 scores ≥ 60.
At 24 weeks, in comparison with placebo, Botox treatment significantly reduced HIT-6 scores at all time periods during the
double-blind phase of the trials (p ≤ 0.014). Additionally, HIT-6 measures of headache impact scores showed significant benefit
for the Botox group at 24 weeks of treatment (p < 0.001). Botox treatment significantly improved all domains of the MSQ v2.1 at
24 weeks (p < 0.001). There was also a significant benefit shown for the Botox group compared to placebo with regard to the
proportion of subjects who received clinically meaningful reduction in the number of headache days at all-time points in the
double-blind study periods (p ≤ 0.025). The authors concluded that Botox treatment reduces headache impact and improves
HRQoL.
The pooled results of two phase 3, randomized, double-blind, multicenter, placebo controlled trials addressing the use of
botulinum toxin for the treatment of chronic migraine headaches were reported by Dodick et al., in 2010.
29-31
These studies were
from the Phase III REsearch Evaluating Migraine Prophylaxis Therapy (PREEMPT) clinical program, involving a 24 week
randomized, double-blind phase followed by a 32 week open-label phase. Subjects were randomized (1:1) to receive either 155
units of onabotulinumtoxinA (BoNT-A) or placebo injections every 12 weeks. A total of 1384 adult patients were randomized to
onabotulinumtoxinA (n = 688) or placebo (n = 696), with study visits every 4 weeks. Both studies were identical in design, with
the exception being the designation of the primary (mean change from baseline in frequency of headache days for the 28-day
period ending with week 24) and secondary endpoints (frequency of migraine days, number of cumulative hours of headache
on headache days, proportion of patients with severe HIT-6 score, and others). Injections of BoNT-A or placebo were injected
as 31 fixed-sites, fixed-dose injections across 7 specific head/neck muscle areas. A discretionary 40 units could be
administered using a “follow-the-pain” strategy, resulting in 195 units over 39 sites. Pooled analyses demonstrated a large mean
decrease from baseline in frequency of headache days, with statistically significant between-group differences favoring
onabotulinumtoxinA over placebo at week 24 (-8.4 vs. -6.6; p < 0.001) and at all other time points. Significant differences
favoring onabotulinumtoxinA were also observed for all secondary efficacy variables at all time points, including frequency of
headache days, cumulative headache hours, and the proportion of subjects with severe headaches. No significant difference
was noted in the frequency of acute headache pain medication taken. There was a significantly greater proportion of
experimental group subjects that had a greater that 50% decrease from baseline in headache days. Adverse events occurred in
62.4% of experimental group subjects and 51.7% of placebo subjects, with a greater than 5% incidence of neck pain and
muscular weakness in the experimental group. The authors concluded that the use of onabotulinumtoxinA treatment for
chronic migraine was effective, safe, and well tolerated.
Overactive Bladder
Nitti et al examined the efficacy and safety of onabotulinumtoxinA for the treatment of overactive bladder and urinary
incontinence (UI) in a phase 3, randomized, multicenter, placebo controlled trial.
93
Adult patients (18 years or older) with
idiopathic overactive bladder who experienced 3 or more urgency UI episodes in a 3-day period and an average of 8 or more
micturitions per day were enrolled in the study. Patients were randomized 1:1 to either receive onabotulinumtoxinA 100 U or
placebo over 20 evenly distributed intradetrusor injections. Co-primary end points were the change from baseline in the number
of urinary incontinence episodes per day and the proportion of patients with a positive response on the treatment benefit scale
at posttreatment week 12. Secondary end points included other overactive bladder symptoms and health related quality of life.
OnabotulinumtoxinA significantly decreased the daily frequency of urinary incontinence episodes vs placebo (–2.65 vs –0.87, p
< 0.001) and 22.9% vs 6.5% of patients became completely continent. A larger proportion of onabotulinumtoxinA than placebo
Botulinum Toxins A and B
Page 14 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
treated patients reported a positive response on the treatment benefit scale (60.8% vs 29.2%, p < 0.001). All other overactive
bladder symptoms improved vs placebo (p < 0.05). OnabotulinumtoxinA improved patient health related quality of life across
multiple measures (p < 0.001). Uncomplicated urinary tract infection was the most common adverse event. A 5.4% rate of
urinary retention was observed. The authors concluded that OnabotulinumtoxinA showed significant, clinically relevant
improvement in all overactive bladder symptoms and health related quality of life in patients inadequately treated with
anticholinergics and was well tolerated.
Spasticity (Associated with Cerebral Palsy)
In a global, randomized, placebo-controlled study, the efficacy and safety of abobotulinumtoxinA was evaluated for the
treatment of spasticity in cerebral palsy children with dynamic equinus foot deformity.
95
Two hundred and forty-one patients
were randomized 1:1:1 to receive either abobotulinumtoxinA 10 U/kg/leg, 15 U/kg/leg, or placebo injections into the
gastrocnemius-soleus complex of either one or both legs. The primary endpoint was the demonstration of benefit for each dose
over placebo on the Modified Ashworth Scale from baseline to week 4. Secondary endpoint includes the change of the
Physician’s Global Assessment at week 4 from baseline. Two hundred and twenty-six patients completed the study. At week 4,
Modified Ashworth Scale scores significantly improved with abobotulinumtoxinA; mean (95% confidence interval) treatment
differences versus placebo were –0.49 (–0.75 to –0.23; p = 0.0002) for 15 U/kg/leg and –0.38 (–0.64 to –0.13; p = 0.003) for 10
U/kg/leg. The Physician’s Global Assessment treatment differences versus placebo of 0.77 (0.45 to 1.10) for 15 U/kg/leg and
0.82 (0.50 to 1.14) for 10 U/kg/leg were also significant (both Ps < .0001). The most common treatment-related adverse event
was muscular weakness (10 U/Kg/leg = 2; placebo = 1). The authors concluded that treatment with abobotulinumtoxinA
improves muscle tone in children with dynamic equinus resulting in an improved overall clinical impression and is well
tolerated.
An additional subgroup analysis was conducted on the same two-hundred and forty-one patients examined in the above study.
Delgado et al. found that abobotulinumtoxin A was similarly effective in treating spasticity in cerebral palsy children with
dynamic equinus foot deformity in both children who had not received botulinum toxin before and children who had previously
received botulinum toxin. Of the 241 patients examined, 113 had received botulinum toxin treatment before participating in the
study. Previous botulinum toxin treatment also had no effect on safety outcomes between the two groups.
97
Unproven
Benign Prostatic Hyperplasia
The efficacy and tolerability of botulinum toxin A (BoNT-A) for the treatment of lower urinary tract symptoms in men with benign
prostatic hyperplasia (LUTS/BPH) was evaluated in a randomized placebo controlled trial involving 315 subjects assigned to
either 200 U of BoNT-A (Botox) (n = 157) or placebo (n = 156).
33
Patients with International Prostate Symptom Score (I-PSS) 14
or greater, with peak urinary flow rate 4 to 15 ml per second and total prostate volume 30 to 80 ml were randomized 1:1 to a
single intraprostatic injection of BoNT-A or placebo. A single-blind sham procedure, followed by a 4 week run in was included to
minimize potential placebo effect. The primary endpoint from baseline is total I-PSS at week 12. Additional endpoints assessed
at weeks 6, 12, and 24 were peak urinary flow rate (Qmax), total prostate volume (TPV), and post-void residual urine volume
(PVR). At all-time points there was no difference in I-PSS between the BoNT-A and placebo groups, included at the primary time
point at 12 weeks, however both groups experienced a decrease (-6.3 vs -5.6 points, p < 0.001). There were no differences
between treatment groups for TPV, PSA, or PVR at 12 or 24 weeks. The authors concluded that BoNT-A is unlikely to be a
therapy for male LUTS/BPH.
In an additional phase III clinical trial completed in 2018, BoNT-A was tested against optimized oral medications in treating
lower urinary tract symptoms (LUTS) due to benign prostatic hyperplasia. Four months after BoNT-A injection, most of the
patients who received BoNT-A were able to interrupt LUTS-related medical treatments, but this study’s design did not allow for
a conclusion that this improvement was related to the study drug rather than a sustained placebo effect.
98
Chronic Daily Headache
Four studies were published in the American Academy of Neurology's 2008 assessment of botulinum neurotoxin for pain
disorders.
15
Each of the studies specifically referenced chronic daily headache (CDH) and had a large population of patients
with transformed migraine. The primary outcome measure for all the studies was mean change in headache-free days per
month. The first study, which used a technique of modifying injection site based on location of pain, showed a significant
benefit (11 days vs. 8 days) in the BoNTA treated population. The second study, the largest of patients with CDH, was a
Botulinum Toxins A and B
Page 15 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
randomized, double-blind, placebo-controlled, phase II study, enrolling 702 patients. This trial used a fixed-site strategy. Eligible
patients were injected with BoNTA at 225 U, 150 U, 75 U, or placebo and returned for additional masked treatments at day 90
and day 180. Patients were assessed every 30 days for 9 months. The primary efficacy end point was the mean change from
baseline in the frequency of headache-free days at day 180 for the placebo nonresponder group. The primary efficacy end
point was not met. Mean improvements from baseline at day 180 of 6.0, 7.9, 7.9, and 8.0 headache-free days per month were
observed with BoNTA at 225 U, 150 U, 75 U, or placebo, respectively (p = 0.44). However, a priori-defined analysis of headache
change from baseline in headache frequency revealed that the 225 U and 150 U Botox A groups had statistically significant
greater reductions in headache frequency compared with placebo at day 240 (p = 0.03). In conclusion, BoNTA was safe and
well tolerated. Although the primary efficacy end point was not met, all groups responded to treatment. The 225 U and 150 U
groups experienced a greater decrease in headache frequency than the placebo group at day 240, but the placebo response
was higher than expected. The third study was a subgroup of patients not taking prophylactic medications from a larger overall
study. Only this subgroup showed a significant mean increase in headache-free days although there was a decrease in the
frequency per 30 days. An additional study evaluated 82 patients with chronic daily headache treated with botulinum neurotoxin
A.
36
76.1% of the chronic migraine patients and 36.4% of the chronic tension-type headache patients were considered
responders. Because studies of botulinum A for the prevention of chronic daily headache show mixed results, further studies
are recommended.
Tension Headache
Four studies of patients with tension-type headache were reviewed in the American Academy of Neurology's 2008 assessment
of botulinum neurotoxin for pain disorders.
15
Patients in these studies were randomized to either botulinum neurotoxin (BoNT)
or placebo. After 6 weeks, the first study (n = 112) showed no significant difference compared to a baseline 6 week period in
the primary outcome measure of area under the headache curve in the subjects' headache diary. In another of the studies, both
the BoNT and the placebo group showed improvement in the primary outcome of mean change from baseline in number of
headache-free days from 30 to 60 after injection, but BoNT was not more beneficial and a power analysis was not provided. A
third study showed no significant benefit of BoNT after 12 weeks for decrease of headache, intensity on visual analog scale,
mean number of headache days, headache hours per day, days on which symptomatic treatment was taken, number of
analgesics taken per day, or patient's assessment of improvement.
5
The fourth study, a smaller trial, included 16 patients in a
prospective double-blind, placebo-controlled crossover study and thirty patients in an open-label long-term study. These
patients showed reduction in headache severity and pericranial muscle tenderness, and increased headache-free days with
botulinum treatment.
Additional small randomized controlled trials have found conflicting results similar to those presented above.
27
Until larger
randomized trials are conducting showing a beneficial effect of BTX-A, its use in tension headache is unproven.
Miscellaneous
Botulinum toxin A has been studied in a number of other disorders including: cricopharyngeal dysphagia,
20-23
gustatory
epiphora (crocodile tears), Sphincter of Oddi dysfunction,
12
pancreas divisum, anismus,
16
lower urinary tract dysfunction,
11,18
pelvic floor spasticity,
18
chronic prostatic pain,
18
severe paradoxical vocal cord movement,
40
post-parotidectomy sialoceles,
severe bruxism,
41-42
temporomandibular disorders,
43-44,48
myofascial pain syndrome,
45,72,81
brachial plexus palsy,
46,80,81
thyroid
associated ophthalmopathy,
47
esophageal spasm,
37
post-thoracotomy pseudoangina, epiphora following salivary gland
transplantation, trigeminal neuralgia,
32,73-4
trismus and stridor in amyotrophic lateral sclerosis, proctalgia fugax,
18
nasal
hypersecretion,
50,67
gastroparesis (including diabetic gastroparesis),
58-62, 80,90-91
Lichen simplex, lateral epicondylitis,
51,52
Stiff-
person syndrome, traumatic sixth nerve palsy, Tourette's syndrome,
55
chronic scrotal pain,
99
and pain and/or wound healing
after hemorrhoidectomy. The studies in these disorders have been small and/or uncontrolled open-label trials. Larger, well-
designed studies must occur to demonstrate the effectiveness of botulinum toxin in the treatment of these conditions.
Technology Assessments
Achalasia
A 2014 Cochrane review was published evaluating and comparing endoscopic pneumatic dilation (PD) versus botulinum toxin
injection in the management of primary achalasia.
34
Seven studies involving 178 participants were included. Two studies were
excluded from the meta-analysis of remission rates on the basis of clinical heterogeneity of the initial endoscopic protocols.
There was no significant difference between PD or botulinum treatment in remission within four weeks of the initial intervention;
with a risk ratio of remission of 1.11 (95% CI 0.97 to 1.27). There was also no significant difference in the mean esophageal
Botulinum Toxins A and B
Page 16 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
pressures between the treatment groups; with a weighted mean difference for PD of -0.77 (95% CI -2.44 to 0.91, p = 0.37). Data
on remission rates following the initial endoscopic treatment were available for three studies at six months and four studies at
12 months. At six months 46 of 57 PD participants were in remission compared to 29 of 56 in the botulinum group, giving a risk
ratio of 1.57 (95% CI 1.19 to 2.08, p = 0.0015); whilst at 12 months 55 of 75 PD participants were in remission compared to 27
of 72 botulinum participants, with a risk ratio of 1.88 (95% CI 1.35 to 2.61, p = 0.0002). No serious adverse outcomes occurred
in participants receiving botulinum, while PD was complicated by perforation in three cases. The authors concluded that PD is
the more effective endoscopic treatment in the long term (greater than six months) for patients with achalasia.
Cervical Dystonia
An update of a Cochrane review from 2005 was published in 2017 to compare the efficacy, safety, and tolerability of botulinum
toxin type A (BtA) versus placebo in people with cervical dystonia.
100
The authors included eight randomized controlled trials
(RCTs) of moderate overall risk of bias, including 1010 participants with cervical dystonia. Six studies excluded participants with
poorer responses to BtA treatment, therefore including an enriched population with a higher probability of benefiting from this
therapy. Only one trial was independently funded. All RCTs evaluated the effect of a single BtA treatment session, using doses
from 150 U to 236 U of onabotulinumtoxinA (Botox), 120 U to 240 U of incobotulinumtoxinA (Xeomin), and 250 U to 1000 U of
abobotulinumtoxinA (Dysport).BtA was associated with a moderate-to-large improvement in the participant's baseline clinical
status as assessed by investigators, with reduction of 8.06 points in the Toronto Western Spasmodic Torticollis Rating Scale
(TWSTRS total score) at week 4 after injection (95% CI 6.08 to 10.05; I2 = 0%) compared to placebo, corresponding on average
to a 18.7% improvement from baseline. The mean difference (MD) in TWSTRS pain subscore at week 4 was 2.11 (95% CI 1.38
to 2.83; I2 = 0%). Overall, both participants and clinicians reported an improvement of subjective clinical status. There were no
differences between groups regarding withdrawals due to adverse events. However, BtA treatment was associated with an
increased risk of experiencing an adverse event (risk ratio (RR) 1.19; 95% CI 1.03 to 1.36; I2 = 16%). Dysphagia (9%) and diffuse
weakness/tiredness (10%) were the most common treatment-related adverse events (dysphagia: RR 3.04; 95% CI 1.68 to 5.50;
I2 = 0%; diffuse weakness/tiredness: RR 1.78; 95% CI 1.08 to 2.94; I2 = 0%). Treatment with BtA was associated with a
decreased risk of participants withdrawing from trials. We have moderate certainty in the evidence across all of the
aforementioned outcomes. The authors found no evidence supporting the existence of a clear dose-response relationship with
BtA, nor a difference between BtA formulations, nor a difference with use of EMG-guided injection. Due to clinical
heterogeneity, the authors did not pool data regarding health-related quality of life, duration of clinical effect, or the
development of secondary non-responsiveness. The authors stated that they have moderate certainty in the evidence that a
single BtA treatment session is associated with a significant and clinically relevant reduction of cervical dystonia-specific
impairment, including severity, disability, and pain, and that it is well tolerated, when compared with placebo. There is also
moderate certainty in the evidence that people treated with BtA are at an increased risk of developing adverse events, most
notably dysphagia and diffuse weakness. There are no data from RCTs evaluating the effectiveness and safety of repeated BtA
injection cycles. There is no evidence from RCTs to allow us to draw definitive conclusions on the optimal treatment intervals
and doses, usefulness of guidance techniques for injection, the impact on quality of life, or the duration of treatment effect.
Chronic and Episodic Migraine Headache
A 2018 Cochrane review was published evaluating the effects of botulinum toxins versus placebo or active treatment for the
prevention or reduction in frequency of chronic or episodic migraine in adults.
75
Twenty-eight studies involving 4,190
participants were eligible for inclusion. The longest treatment duration was three rounds of injections with three months
between treatments, so the authors could not analyze long-term effects. For the primary analyses, the authors pooled data from
both chronic and episodic participant populations. Where possible, the authors also separated data into chronic migraine,
episodic migraine and 'mixed group' classification subgroups. Most trials (21 out of 28) were small (fewer than 50 participants
per trial arm). The risk of bias for included trials was low or unclear across most domains, with some trials reporting a high risk
of bias for incomplete outcome data and selective outcome reporting. Twenty-three trials compared botulinum toxin with
placebo. Botulinum toxin may reduce the number of migraine days per month in the chronic migraine population by 3.1 days
(95% confidence interval (CI) -4.7 to -1.4, 4 trials, 1497 participants, low-quality evidence). This was reduced to -2 days (95% CI -
2.8 to -1.1, 2 trials, 1384 participants; moderate-quality evidence) when the authors removed small trials. A single trial of people
with episodic migraine (n = 418) showed no difference between groups for this outcome measure (p = 0.49).In the chronic
migraine population, botulinum toxin reduces the number of headache days per month by 1.9 days (95% CI -2.7 to -1.0, 2 trials,
1384 participants, high-quality evidence). The authors did not find evidence of a difference in the number of migraine attacks
for both chronic and episodic migraine participants (6 trials, n = 2004, p = 0.30, low-quality evidence). For the population of
both chronic and episodic migraine participants a reduction in severity of migraine rated during clinical visits, on a 10 cm visual
analog scale (VAS) of 3.3 cm (95% CI -4.2 to -2.5, very low-quality evidence) in favor of botulinum toxin treatment came from
Botulinum Toxins A and B
Page 17 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
four small trials (n = 209); better reporting of this outcome measure from the additional eight trials that recorded it may have
improved our confidence in the pooled estimate. Global assessment and quality-of-life measures were poorly reported and it
was not possible to carry out statistical analysis of these outcome measures. Analysis of adverse events showed an increase in
the risk ratio with treatment with botulinum toxin over placebo 30% (RR 1.28, 95% CI 1.12 to 1.47, moderate-quality evidence).
For every 100 participants 60 experienced an adverse event in the botulinum toxin group compared with 47 in the placebo
group. Three trials studied comparisons with alternative oral prophylactic medications. Meta-analyses were not possible for
number of migraine days, number of headache days or number of migraine attacks due to insufficient data, but individually
trials reported no differences between groups for a variety of efficacy measures in the population of both chronic and episodic
migraine participants. The global impression of disease measured using Migraine Disability Assessment (MIDAS) scores were
reported from two trials that showed no difference between groups. Compared with oral treatments, botulinum toxin showed no
between-group difference in the risk of adverse events (2 trials, n = 114, very low-quality evidence). The relative risk reduction
(RRR) for withdrawing from botulinum toxin due to adverse events compared with the alternative prophylactic agent was 72% (p
= 0.02, 2 trials, n = 119). There were insufficient data available for the comparison of different doses. The quality of the evidence
assessed using GRADE methods was varied but mostly very low; the quality of the evidence for the placebo and active control
comparisons was low and very low, respectively for the primary outcome measure. Small trial size, high risk of bias and
unexplained heterogeneity were common reasons for downgrading the quality of the evidence. The authors concluded that for
chronic migraine, botulinum toxin type A may reduce the number of migraine days per month by 2 days compared with placebo
treatment. Non-serious adverse events were probably experienced by 60/100 participants in the treated group compared with
47/100 in the placebo group. For people with episodic migraine, the authors remain uncertain whether or not this treatment is
effective because the quality of this limited evidence is very low. Better reporting of outcome measures in published trials would
provide a more complete evidence base on which to draw conclusions.
Chronic Migraine Headache
Hayes compiled a Medical Technology Directory on botulinum toxin treatment for migraine headache dated September 22,
2011.
75
Although a relatively large number of well-designed randomized controlled trials (RCTs) have evaluated
onabotulinumtoxinA (onaBTX-A) and abobotulinumtoxinA (aboBTX-A) [BTX-A] for prevention of migraine, the clinical role of this
treatment remains to be established. Many of the available placebo-controlled RCTs found that BTX-A did not provide
statistically significant benefits or found that the benefits obtained were inconsistent, for instance, occurring at some time
points but not at others. In contrast, the largest available RCT and one of the older RCTs found that patients who underwent
treatment with onaBTX-A experienced statistically significant improvements such as reductions in migraine frequency and
severity. This divergence in study results cannot be resolved based solely on differences in study size and a more likely
explanation was that the benefits obtained with onaBTX-A were relatively small, perhaps too small to be clinically significant.
Moreover, due to lack of long-term follow-up, the available RCTs do not provide any data concerning the durability of potential
benefits from treatment with onaBTX-A. In addition, there was insufficient evidence to support conclusions regarding the
efficacy of onaBTX-A relative to other types of medication for prevention of migraine. Likewise, there was very limited evidence
regarding the effectiveness of aboBTX-A, and no evidence regarding other types of BTX, for the management of chronic or
recurrent headache. Therefore, Hayes has assigned a D rating (no proven benefit and/or not safe) to abobotulinumtoxinA for
prevention of migraine and to rimabotulinumtoxinB as a treatment for migraine headache. Overall, onaBTX-A was safe with few
serious complications reported, earning onabotulinumtoxinA a Hayes rating of C (potential but unproven benefit) for prevention
of migraine headache. Further studies are needed to determine the clinical role of BTX-A relative to current treatments for
prevention of migraine. An annual review of the Hayes Directory on August 21, 2019 resulted in no changes to the original
findings.
Chronic Tension Headache
Hayes compiled a Medical Technology Directory on botulinum toxin treatment for chronic tension-type headache dated
December 30, 2011.
78
A relatively large number of well-designed, randomized, placebo-controlled trials (RCTs) have evaluated
the effects of botulinum toxin A (BTX-A) on patients diagnosed with chronic tension-type headache (CTTH). The majority of
these studies found no benefit of BTX-A relative to placebo. The two studies that did report beneficial effects of BTX on
headache frequency and intensity were very small. Overall, BTX-A was safe. None of the studies compared BTX-A with other
prophylactic treatments for CTTH. An annual review of the Hayes Directory on January 13, 2015 resulted in no changes to the
original findings.
Botulinum Toxins A and B
Page 18 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Detrusor Overactivity
Hayes compiled a Medical Technology Directory on botulinum toxin treatment for detrusor instability, dated December 30,
2011.
86
The results of the available studies provide some evidence that onabotulinumtoxinA (onaBTX-A) improves outcomes for
patients who have idiopathic or neurogenic detrusor overactivity; however, these studies do not provide sufficient evidence to
establish the clinical role of botulinum toxin type A (BTX-A) for these indications. Although randomized clinical trials (RCTs)
consistently found that BTX-A provided statistically significant improvements in urinary incontinence (UI) compared with
placebo treatment, the largest available RCT of BTX-A for idiopathic detrusor overactivity found a placebo effect that was nearly
as large as the treatment effect when expressed in terms of decrease in number of episodes of UI per week. In the largest
available RCT of BTX-A for neurogenic detrusor overactivity, BTX-A treatment was associated with statistically significant
increases in urinary retention and urinary tract infections. None of the studies that met the criteria for review involved long-term
follow-up of patients who underwent treatment with multiple doses of BTX-A, and none of the studies compared BTX-A with
augmentation cystoplasty or neuromodular implantation. At least six of the studies were sponsored by the manufacturer,
creating the potential for bias. Additional controlled studies are needed to determine the long-term efficacy and safety of BTX-A
relative to other current invasive treatments for idiopathic and neurogenic detrusor overactivity. An annual review of the Hayes
Directory on January 9, 2015 resulted in no changes to the original findings.
Strabismus
A 2017 update to a 2012 Cochrane review was published to examine the efficacy of botulinum toxin therapy in the treatment of
strabismus compared with alternative conservative or surgical treatment options.
35
The review also sought to determine the
types of strabismus that particular benefit from the use of botulinum toxin as a treatment option. The secondary objectives were
to investigate the dose effect and complication rates associated with botulinum therapy. Six randomized controlled trials were
eligible for inclusion. The authors concluded that the published literature on the use of botulinum toxin in the treatment of
strabismus consists of retrospective studies, cohort studies or case reviews. These provide useful descriptive information,
clarification is required as to the effective use of botulinum toxin as an independent treatment modality. Six RCTs on the
therapeutic use of botulinum toxin in strabismus, graded as low and very low-certainty evidence, have shown varying
responses. These include a lack of evidence for effect of botulinum toxin on reducing visual symptoms in acute sixth nerve
palsy, poor response in people with horizontal strabismus without binocular vision, similar or slightly reduced achievement of
successful ocular alignment in children with esotropia and potential increased achievement of successful ocular alignment
where surgery and botulinum toxin are combined. Further high quality trials using robust methodologies are required to
compare the clinical and cost effectiveness of various forms of botulinum toxin (e.g. Dysport, Xeomin, etc.), to compare
botulinum toxin with and without adjuvant solutions and to compare botulinum toxin to alternative surgical interventions in
strabismus cases with and without potential for binocular vision.
Motor/Phonic Tics
A 2018 Cochrane review was published evaluating the safety and effectiveness of botulinum toxin in treating motor and phonic
tics in people with Tourette’s syndrome, and to analyze the effect of botulinum toxin on premonitory urge and sensory tics.
95
Only one randomized placebo-controlled, double-blind cross-over study met our selection criteria. In this study, 20 participants
with motor tics were enrolled over a three-year recruitment period; 18 (14 of whom had a diagnosis of Tourette's syndrome)
completed the study; in total, 21 focal motor tics were treated. Although we considered most bias domains to be at low risk of
bias, the study recruited a small number of participants with relatively mild tics and provided limited data for our key outcomes.
The effects of botulinum toxin injections on tic frequency, measured by videotape or rated subjectively, and on premonitory
urge, are uncertain (very low-quality evidence). The quality of evidence for adverse events following botulinum toxin was very
low. Nine people had muscle weakness following the injection, which could have led to unblinding of treatment group
assignment. No data were available to evaluate whether botulinum injections led to immunoresistance to botulinum. The
authors concluded that they are uncertain about botulinum toxin effects in the treatment of focal motor and phonic tics in select
cases, as we assessed the quality of the evidence as very low. Additional randomized controlled studies are needed to
demonstrate the benefits and harms of botulinum toxin therapy for the treatment of motor and phonic tics in patients with
Tourette's syndrome.

Botulinum Toxins A and B
Page 19 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Professional Societies
Spasmodic Dysphonia (Laryngeal Dystonia)
In 2018, the American Academy of Otolaryngology – Head and Neck Surgery published an update of their guideline first
published in 2009.
96
The organization recommended that clinicians should offer, or refer to a clinician who can offer botulinum
toxin injections for the treatment of dysphonia caused by spasmodic dysphonia and other types of laryngeal dystonia.
A recommendation means that the benefits exceed the harms (or that the harms exceed the benefits, in the case of a negative
recommendation) but that the quality of evidence is not as strong (grade B or C). In some clearly identified circumstances,
recommendations may be made on the basis of lesser evidence when high-quality evidence is impossible to obtain and the
anticipated benefits outweigh the harms. Clinicians should also generally follow a recommendation but should remain alert to
new information and sensitive to patient preferences.
Achalasia
In 2020, the American College of Gastroenterology published an evidence-based clinical guideline for the diagnosis and
management of achalasia based on a comprehensive review of the pertinent evidence and examination of relevant published
data.
85
The recommendations for the treatment of achalasia from this guideline are as follows:
In patients with achalasia who are candidates for definite therapy:
o Pneumatic dilation (PD), laparoscopic Heller myotomy (LHM), and peroral endoscopic myotomy (POEM) are
comparable effective therapies for type I or type II achalasia.
o POEM would be a better treatment option in those with type III achalasia.
o Botulinum toxin injection is reserved for those who cannot undergo the above definitive therapies.
Recommend botulinum toxin injection as first-line therapy for patients with achalasia who are unfit for definitive
therapies compared with other less effective pharmacological therapies (Grade quality: Moderate;
Recommendation strength: Strong).
Previous treatment with botulinum toxin injection does not significantly affect performance and outcomes of
myotomy (Grade quality: Low; Recommendation strength: Conditional).
Autonomic & Movement Disorders, Pain, and Spasticity
In a 2013 update to the 2008 Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology
(AAN) published evidence-based (studies classified as Class I to IV and recommendations classified as levels A to U)
69
assessments on the use of botulinum neurotoxin in the treatment of autonomic disorders and pain,
15
movement disorders,
19
and spasticity.
39
In addition, in 2013 authors performed an assessment on the use of botulinum neurotoxin in the treatment of
urologic conditions
87
and secretory disorders
88
based on the AAN methodology. The Quality Standards Subcommittee of the
American Academy of Neurology and the Practice Committee of the Child Neurology Society also published an evidence-based
review of the pharmacologic treatment of spasticity in children and adolescents with cerebral palsy in 2010.
6
Recommendations from these reviews are classified as follows:
Level A - Established as effective, ineffective, or harmful for the given condition in the specified population, requiring at
least two consistent Class I studies.
Level B - Probably effective, ineffective, or harmful for the given condition in the specified population, requiring at least one
Class I study or at least two consistent Class II studies.
Level C - Possibly effective, ineffective, or harmful for the given condition in the specified population, requiring at least one
Class II study or two consistent Class III studies.
Level U - Data inadequate or conflicting; given current knowledge, treatment is unproven.
Recommendations from these reviews are:
BoNT should be offered as a treatment option for axillary hyperhidrosis and detrusor overactivity (detrusor hyperreflexia)
(Level A). BoNT should be considered for palmar hyperhidrosis, sialorrhea, and detrusor sphincter dyssynergia after spinal
cord injury (Level B).
BoNT is probably effective for the treatment of benign prostatic hyperplasia induced lower urinary tract symptoms (Level
B).
BoNT may be considered for low back pain (Level C). BoNT is probably ineffective in episodic migraine and chronic
tension-type headache (Level B).

Botulinum Toxins A and B
Page 20 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Evidence does not permit drawing conclusions on BoNT’s efficacy in chronic daily headache (mainly transformed migraine)
(Level U). Evidence does not support BoNT’s efficacy for the treatment of gustatory sweating (Level U).
BoNT should be offered as an option for the treatment of blepharospasm, cervical dystonia (Level A).
BoNT may be offered for , hemifacial spasm, focal upper extremity dystonia, , and upper extremity essential tremor (Level
B).
BoNT may be considered for, adductor laryngeal dystonia, focal lower limb dystonia, oromandibular dystonia, and motor
tics (Level C).
BoNT should be offered as an option for the treatment of spasticity in adults (Level A). Spasticity in adults results from a
variety of causes such as stroke, trauma, multiple sclerosis, and neoplasm involving the central nervous system.
For localized/segmental spasticity that warrants treatment in children and adolescents with cerebral palsy, botulinum toxin
type A should be offered as an effective and generally safe treatment (Level A) and there is insufficient data to support or
refute the use of botulinum toxin type B (Level U).
Tics in People with Tourette’s Syndrome and Chronic Tic Disorder
In 2019, the American Academy of Neurology (AAN) published evidence-based guideline recommendations regarding the use
of botulinum neurotoxins in treating tics in people with Tourette’s Syndrome, as well as treating chronic tic disorder (studies
classified as Class I to IV and recommendations classified as levels A to C).
101
The recommendations for the treatment of tics in
people with Tourette’s Syndrome and chronic tic disorder from this guideline are as follows:
• Physicians may prescribe botulinum toxin injections for the treatment of older adolescents and adults with localized and
bothersome simple motor tics when the benefits of treatment outweigh the risks (Level C).
• Physicians may prescribe botulinum toxin injections for the treatment of older adolescents and adults with severely
disabling or aggressive vocal tics when the benefits of treatment outweigh the risks (Level C).
• Physicians must counsel individuals with tics that botulinum toxin injections may cause weakness and hypophonia, and
that all effects are temporary (Level A).
Blepharospasm, Cervical Dystonia, Adult Spasticity, and Headache
In a 2016 update to the 2008 guidelines, the American Academy of Neurology (AAN) published evidence-based (studies
classified as Class I to IV and recommendations classified as levels A to U)
286
assessments on the use of botulinum neurotoxins
in the treatment of blepharospasm, cervical dystonia, headache, and adult spasticity.
89
Recommendations from this review are classified as follows:
Level A - Established as effective, ineffective, or harmful for the given condition in the specified population, requiring at
least two consistent Class I studies.
Level B - Probably effective, ineffective, or harmful for the given condition in the specified population, requiring at least one
Class I study or at least two consistent Class II studies.
Level C - Possibly effective, ineffective, or harmful for the given condition in the specified population, requiring at least one
Class II study or two consistent Class III studies.
Level U - Data inadequate or conflicting; given current knowledge, treatment is unproven.
Recommendations from this review for abobotulinumtoxinA (aboBoNT-A, Dysport) are as follows:
AboBoNT-A should be offered as a treatment option for cervical dystonia, focal manifestations of upper limb spasticity, and
focal manifestations of lower limb spasticity that warrant treatment (Level A).
o AboBoNT-A has been established as safe and effective for the reduction of adult upper limb spasticity and
improvement of passive function (multiple Class I studies). AboBoNT-A has also been established as safe and effective
for the reduction of adult lower limb spasticity (multiple Class I studies).
o Data is inadequate to determine the efficacy of aboBoNT-A for improvement of active function associated with adult
upper limb spasticity (Class I studies, inconsistent results dependent on active functional outcomes). Data is also
inadequate to determine the efficacy of aboBoNT-A for improvement of active function associated with adult lower limb
spasticity (no studies available or inconsistent results dependent on specific outcome from multiple Class I studies).
AboBoNT-A may be considered as a treatment option for blepharospasm (Level C).
Recommendations from this review for incobotulinumtoxinA (incoBoNT-A, Xeomin) are as follows:
IncoBoNT-A should be offered as a treatment option for focal manifestations of upper limb spasticity (Level A).
o IncoBoNT-A has been established as safe and effective for the reduction of adult upper limb spasticity and
improvement of passive function (multiple Class I studies).

Botulinum Toxins A and B
Page 21 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
o Data is inadequate to determine the efficacy of incoBoNT-A for improvement of active function associated with adult
upper limb spasticity (Class I studies, inconsistent results dependent on active functional outcomes).
IncoBoNT-A should be considered as a treatment option for blepharospasm and cervical dystonia (Level B).
There is insufficient evidence to support or refute the use of incoBoNT-A for the treatment of lower limb spasticity (Level U).
Recommendations from this review for onabotulinumtoxinA (onaBoNT-A, Botox) are as follows:
OnaBoNT-A should be offered as a treatment option for focal manifestations of upper limb spasticity, focal manifestations
of lower limb spasticity that warrant treatment, and chronic migraine (Level A).
o OnaBoNT-A has been established as safe and effective for the reduction of adult upper limb spasticity and
improvement of passive function (multiple Class I studies). OnaBoNT-A has also been established as safe and effective
for the reduction of adult lower limb spasticity (multiple Class I studies).
o Data is inadequate to determine the efficacy of onaBoNT-A for improvement of active function associated with adult
upper limb spasticity (Class I studies, inconsistent results dependent on active functional outcomes). Data is also
inadequate to determine the efficacy of onaBoNT-A for improvement of active function associated with adult lower limb
spasticity (no studies available or inconsistent results dependent on specific outcome from multiple Class I studies).
OnaBoNT-A should be considered as a treatment option for blepharospasm and cervical dystonia (Level B).
OnaBoNT-A should not be offered as a treatment option for episodic migraine (Level A).
OnaBoNT-A should not be considered as a treatment option for tension-type headache (Level B).
Recommendations from this review for rimabotulinumtoxinB (rimaBoNT-B, Myobloc) are as follows:
RimaBoNT-B should be offered as a treatment option for cervical dystonia (Level A).
RimaBoNT-B should be considered as a treatment option for focal manifestations of upper limb spasticity (Level B).
o RimaBoNT-B is probably safe and effective for the reduction of adult upper limb spasticity (1 Class I study).
o Data is inadequate to determine the efficacy of rimaBoNT-B for improvement of active function associated with adult
upper limb spasticity (Class I studies, inconsistent results dependent on active functional outcomes).
There is insufficient evidence to support or refute the use of rimaBoNT-B for the treatment of blepharospasm and lower
limb spasticity (Level U).
U.S. Food and Drug Administration (FDA)
This section is to be used for informational purposes only. FDA approval alone is not a basis for coverage.
For non-cosmetic use, abobotulinumtoxinA (Dysport) is FDA approved for the treatment of adults with cervical dystonia. Dysport
is also indicated for the treatment of spasticity in pediatric patients 2 years of age and older.
10
IncobotulinumtoxinA (Xeomin) is FDA approved for the treatment of adults with cervical dystonia.. Xeomin is also indicated for
the treatment of adults with blepharospasm, upper limb spasticity in adult patients, and chronic sialorrhea in patients 2 years of
age and older. Xeomin is also indicated for the treatment of upper limb spasticity in pediatric patients 2 to 17 years of age,
excluding spasticity caused by cerebral palsy.
70
For non-cosmetic use, daxibotulinumtoxinA-lanm (Daxxify) is FDA approved for the treatment of cervical dystonia in adult
patients.
102
For non-cosmetic use, onabotulinumtoxinA (Botox) is FDA approved for the prophylaxis of headaches in adult patients with
chronic migraine (≥ 15 days per month with headache lasting 4 hours a day or longer). Safety and effectiveness of Botox have
not been established for the prophylaxis of episodic migraine (14 headache days or fewer per month).
1
Botox is also approved for treatment of spasticity in patients 2 years of age and older.
Botox is also indicated for reducing the severity of abnormal head position and neck pain associated with cervical dystonia in
adults; for the treatment of strabismus and blepharospasm associated with dystonia; for the treatment of overactive bladder
with symptoms of urge urinary incontinence, urgency, and frequency in adults who have an inadequate response or are
intolerant to an anticholinergic medication; for the treatment of urinary incontinence due to detrusor overactivity associated with
a neurologic condition [e.g., spinal cord injury (SCI), multiple sclerosis (MS)] in adults who have an inadequate response to or

Botulinum Toxins A and B
Page 22 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
are intolerant of an anticholinergic medication; and for the treatment of severe primary axillary hyperhidrosis that is
inadequately managed with topical agents.
1
Safety and efficacy of Botox for hyperhidrosis in other body areas have not been
established. Weakness of hand muscles and blepharoptosis may occur in patients who receive Botox for palmar hyperhidrosis
and facial hyperhidrosis, respectively. Patients should be evaluated for potential causes of secondary hyperhidrosis (e.g.,
hyperthyroidism) to avoid symptomatic treatment of hyperhidrosis without the diagnosis and/or treatment of the underlying
disease. Safety and effectiveness of Botox have not been established for the treatment of axillary hyperhidrosis in pediatric
patients under age 18.
RimabotulinumtoxinB (Myobloc) is FDA approved for the treatment of adults with cervical dystonia to reduce the severity of
abnormal head position and neck pain associated with cervical dystonia. It is also FDA approved for the treatment of chronic
sialorrhea in adults.
2
All botulinum toxin products approved by the FDA carry a black box warning regarding the possibility of the distant spread of
toxin effect.
1,2,10,70
The warning states that post marketing reports indicate that the effects of all botulinum toxin products may
spread from the area of injection to produce symptoms consistent with botulinum toxin effects. These may include asthenia,
generalized muscle weakness, diplopia, ptosis, dysphagia, dysphonia, dysarthria, urinary incontinence and breathing
difficulties. These symptoms have been reported hours to weeks after injection. Swallowing and breathing difficulties can be life
threatening and there have been reports of death. The risk of symptoms is probably greatest in children treated for spasticity
but symptoms can also occur in adults treated for spasticity and other conditions, particularly in those patients who have an
underlying condition that would predispose them to these symptoms. In unapproved uses, including spasticity in children, and
in approved indications, cases of spread of effect have been reported at doses comparable to those used to treat cervical
dystonia and upper limb spasticity and at lower doses.
References
1. Botox [prescribing information]. Irvine, CA: Allergan Pharmaceuticals, Inc., November 2023.
2. Myobloc [prescribing information]. Rockville, MD: Solstice Neurosciences, Inc., March 2021.
3. Elmiyeh B, Prasad VM, Upile T, et al. A single-centre retrospective review of unilateral and bilateral Dysport injections in
adductor spasmodic dysphonia. Logoped Phoniatr Vocol. 2010;35(1):39-44.
4. Truong DD, Bhidayasiri R. Botulinum toxin therapy of laryngeal muscle hyperactivity syndromes: comparing different
botulinum toxin preparations. Eur J Neurol. 2006;13(Suppl 1):36-41.
5. Upile T, Elmiyeh, Jerjes W, et al. Unilateral versus bilateral thyroartytenoid botulinum toxin injections in adductor spasmodic
dysphonia: a prospective study. Head Face Med. 2009;5:20.
6. Delgado MR, Hirtz D, Aisen M, et al. Practice Parameter: Pharmacologic treatment of spasticity in children and adolescents
with cerebral palsy (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy
of Neurology and the Practice Committee of the Child Neurology Society. Neurology. 2010;74(4):336-43.
7. Brisinda G, Cadeddu F, Brandara F, et al. Randomized clinical trial comparing botulinum toxin injections with 0.2 per cent
nitroglycerin ointment for chronic anal fissure. Br J Surg. 2007;94(2):162-7.
8. Brisinda G, Cadeddu F, Brandara F, et al. Botulinum toxin for recurrent anal fissure following lateral internal
sphincterotomy. Br J Surg. 2008;95(6):774-8.
9. Hartl DM, Julieron M, LeRidant AM, et al. Botulinum toxin A for quality of life improvement in post-parotidectomy gustatory
sweating (Frey’s syndrome). J Laryngol Otol. 2008;122(10):1100-4.
10. Dysport [prescribing information]. Wrexham, UK: Ipsen Biopharm Ltd., January 2023.
11. Chen JL, Chen CY, Kuo HC. Botulinum toxin A injection to the bladder neck and urethra for medically refractory lower
urinary tract symptoms in men without prostatic obstruction. J Formos Med Assoc. 2009;108(12):950-6.
12. Murray W, Kong S. Botulinum toxin may predict the outcome of endoscopic sphincterotomy in episodic functional post-
cholecystectomy biliary pain. Scand J Gastroenterol. 2010;Feb 15.
13. Silva J, Pinto R, Carvalho T, et al. Intraprostatic Botulinum Toxin Type A injection in patients with benign prostatic
enlargement: duration of the effect of a single treatment. BMC Urol. 2009;9:9.
Botulinum Toxins A and B
Page 23 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
14. Yun JY, Kim JW, Kim HT, et al. Dysport and Botox at a ratio of 2.5:1 units in cervical dystonia: a double-blind, randomized
study. Mov Disord. 2015 Feb;30(2):206-13.
15. Naumann M, So Y, Argoff CE, et al. Assessment: Botulinum neurotoxin in the treatment of autonomic disorders and pain
(an evidence-based review): Report of the Therapeutics and Technology Assessment Subcommittee of the American
Academy of Neurology. Neurology. 2008;70(19):1707-14.
16. Farid M, El Monem HA, Omar W, et al. Comparative study between biofeedback retraining and botulinum neurotoxin in the
treatment of anismus patients. Int J Colorectal Dis. 2009;24(1):115-20.
17. Cruz F, Herschorn S, Aliotta P, et al. Efficacy and Safety of OnabotulinumtoxinA in Patients with Urinary Incontinence Due
to Neurogenic Detrusor Overactivity: A Randomised, Double-Blind, Placebo-Controlled Trial. Eur Urol (2011), doi:10.1016/
j.eururo.2011.07.002.
18. Apostolidis A, Dasgupta P, Denys P, et al. Recommendations on the Use of Botulinum Toxin in the Treatment of Lower
Urinary Tract Disorders and Pelvic Floor Dysfunctions: A European Consensus Report. Eur Urol. 2009;55(1):100-20.
19. Hallett M, Albanese A, Dressler D, Segal KR, Simpson DM, Truong D, Jankovic J. Evidence-based review, and assessment
of botulinum neurotoxin for the treatment of movement disorders. Toxicon. 2013 Jun 1;67:94-114.
20. Oh TH, Brumfield KA, Hoskin TL, et al. Dysphagia in inclusion body myositis: clinical features, management, and clinical
outcomes. Am J Phys Med Rehabil. 2008;87(11):883-9.
21. Krause E, Schirra J, Gurkov R. Botulinum toxin a treatment of cricopharyngeal dysphagia after subarachnoid hemorrhage.
Dysphagia. 2008;23(4):406-10.
22. Suzukia Y, Sanio N, Shinonaga C, et al. Successful botulinum toxin treatment of dysphagia in a spinal muscular atrophy
type 2 patient. Brain Dev. 2007;29(10):662-5.
23. Alfonsi E, Merlo IM, Ponzio M, et al. An electrophysiological approach to the diagnosis of neurogenic dysphagia:
implications for botulinum toxin treatment. J Neurol Neurosurg Psychiatry. 2010;81(1):54-60.
24. Saper JR, Mathew NT, Loder EW, et al. A double-blind, randomized, placebo-controlled comparison of botulinum toxin type
A injection sites and doses in the prevention of episodic migraine. Pain Med. 2007;8(6):478-85.
25. Relja M, Poole AC, Schoenen J, et al. A multicentre, double-blind, randomized, placebo-controlled, parallel group study of
multiple treatments of botulinum toxin type A (BoNTA) for the prophylaxis of episodic migraine headaches. Cephalgia.
2007;27(6):492-503.
26. Aurora SK, Gawel M, Brandes JL, et al. Botulinum toxin type a prophylactic treatment of episodic migraine: a randomized,
double-blind, placebo-controlled exploratory study. Headache. 2007;47(4):486-99.
27. Kemal Erdemoglu A, Barlibas A. The long-term efficacy and safety of botulinum toxin in refractory chronic tension-type
headache. J Headache Pain. 2007;8(5):294-300.
28. Lipton RB, Varon SF, Grosberg B, et al. OnabotulinumtoxinA improves quality of life and reduces impact of chronic
migraine. Neurology. 2011; 77(15):1465-1472.
29. Aurora SK, Dodick DW, Turkel CC, et al.; PREEMPT 1 Chronic Migraine Study Group. Onabotulinumtoxin A for treatment of
chronic migraine: Results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 1 trial. Cephalgia
2010; 30(7):793-803.
30. Diener HC, Dodick DW, Aurora SK, et al. OnabotulinumtoxinA for treatment of chronic migraine: results from the double-
blind, randomized, placebo-controlled phase of the PREEMPT 2 trial. Cephalgia. 2010; 30(7):804-814.
31. Dodick DW, Turkel CC, Degryse RE, et al. OnabotulinumtoxinA for treatment of chronic migraine: pooled results from the
double-blind, randomized, placebo-controlled phases of the PREEMPT clinical program. Headache. 2010; 50(6):921-936.
32. Zhang H, Lian Y1, Ma Y, Chen Y, He C, Xie N, Wu C. Two doses of botulinum toxin type A for the treatment of trigeminal
neuralgia: observation of therapeutic effect from a randomized, double-blind, placebo-controlled trial. J Headache Pain.
2014 Sep 27;15:65.
33. McVary KT, Roehrborn CG, Chartier-Kastler E, et al. A multicenter, randomized, double-blind, placebo controlled study of
onabotulinumtoxinA 200 U to treat lower urinary tract symptoms in men with benign prostatic hyperplasia. J Urol. 2014;
192(1):150-156.
Botulinum Toxins A and B
Page 24 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
34. Leyden JE, Moss AC, MacMathuna P. Endoscopic pneumatic dilation versus botulinum toxin injection in the management
of primary achalasia. Cochrane Database Syst Rev. 2014;12:CD005046.
35. Rowe FJ, Noonan CP. Botulinum toxin for the treatment of strabismus. Cochrane Database Syst Rev. 2017 Mar
2;3:CD006499.
36. Mathew NT, Kailasam J, Meadors L. Predictors of Response to Botulinum Toxin Type A (BoNTA) in Chronic Daily
Headache. Headache. 2008;48(2);194-200.
37. Krause E, Hempel JM, Gürkov R. Botulinum toxin A prolongs functional durability of voice prostheses in laryngectomees
with pharyngoesophageal spasm. Am J Otolaryngol. 2009 Nov-Dec;30(6):371-5.
38. de Bree R, Duyndam JE, Kuik DJ, Leemans CR. Repeated botulinum toxin type A injections to treat patients with Frey
syndrome. Arch Otolaryngol Head Neck Surg. 2009;135(3):287-90.
39. Esquenazi A, Albanese A, Chancellor MB, Elovic E, Segal KR, Simpson DM, Smith CP, Ward AB. Evidence-based review,
and assessment of botulinum neurotoxin for the treatment of adult spasticity in the upper motor neuron syndrome.
Toxicon. 2013 Jun 1;67:115-28.
40. Baldwin MK, Benumof JL. Paradoxical vocal cord movement: a unique case of occurrence and treatment. Anesthesiology.
2007;107(2):359.
41. Guarda-Nardini L, Manfredini D, Salamone M, et al. Efficacy of botulinum toxin in treating myofascial pain in bruxers: a
controlled placebo pilot study. Cranio. 2008;26(2):126-35.
42. Santos MT, Manzano FS, Genovese WJ. Different approaches to dental management of self-inflicted oral trauma: oral
shield, botulinum toxin type A neuromuscular block, and oral surgery. Quintessence Int. 2008;39(2):e63-9.
43. Kurtoglu C, Gur OH, Kurkcu M, et al. Effect of botulinum toxin-A in myofascial pain patients with or without functional disc
displacement. J Oral Maxillofac Surg. 2008;66(8):1644-51.
44. Vázquez Bouso O, Forteza González G, Mommsen J, et al. Neurogenic temporomandibular joint dislocation treated with
botulinum toxin: report of 4 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(3):e33-7.
45. Lew HL, Lee EH, Castaneda A, et al. Therapeutic use of botulinum toxin type A in treating neck and upper-back pain of
myofascial origin: a pilot study. Arch Phys Med Rehabil. 2008;89(1):75-80.
46. Price AE, Ditaranto P, Yaylali I, et al. Botulinum toxin type A as an adjunct to the surgical treatment of the medial rotation
deformity of the shoulder in birth injuries of the brachial plexus. J Bone Joint Surg Br. 2007;89(3):327-9.
47. Wutthiphan S. Role of botulinum toxin A in diplopia following orbital decompression. Strabismus. 2008;16(3): 112-5.
48. Fu KY, Chen HM, Sun ZP, et al. Long-term efficacy of botulinum toxin type A for the treatment of habitual dislocation of the
temporomandibular joint. Br J Oral Maxillofac Surg. 2009 Aug 6. [Epub ahead of print].
49. Yoon SJ, Ho J, Kang HY, et al. Low-dose botulinum toxin type A for the treatment of refractory piriformis syndrome.
Pharmacotherapy. 2007;27(5):657-65.
50. Sapci T, Yazici S, Evcimik MF, et al. Investigation of the effects of intranasal botulinum toxin type A and ipratropium
bromide nasal spray on nasal hypersecretion in idiopathic rhinitis without eosinophilia. Rhinology. 2008;46(1);45-51.
51. Oskarsson E, Piehl AK, Gustafsson BE, Pettersson K. Improved intramuscular blood flow and normalized metabolism in
lateral epicondylitis after botulinum toxin treatment. Scan J Med Sci Sports. Scand J Med Sci Sports. 2009;19(3):323-8.
52. Placzek R, Drescher W, Deuretzbacher G, et al. Treatment of chronic radial epicondylitis with botulinum toxin A. A double-
blind, placebo-controlled, randomized multicenter study. J Bone Joint Surg Am. 2007;89(2):255-60.
53. Akbar M, Abel, R, Seyler-Thorsten M, et al. Repeated botulinum-A toxin injections in the treatment of myelodysplastic
children and patients with spinal cord injuries with neurogenic bladder dysfunction. BJU Int. 2007;100(3):639-45.
54. Del Popolo G, Filocamo MT, Li Marzi V, et al. Neurogenic Detrusor Overactivity Treated with English Botulinum Toxin A: 8-
Year Experience of One Single Centre. Eur Urol. 2008;53(5):1013-20.
55. Aguirregomozcorta M, Pagonabarraga J, Diza-Manera J, et al. Efficacy of botulinum toxin in severe Tourette syndrome with
dystonic tics involving the neck. 2008;14(5):443-5.
56. Lagalla G, Millevolte M, Capecci M, et al. Long-lasting benefits of botulinum toxin type B in Parkinson's disease-related
drooling. J Neurol. 2009;256(4):563-7.
Botulinum Toxins A and B
Page 25 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
57. Wilken B, Aslami B, Backes H. Successful treatment of drooling in children with neurological disorders with botulinum toxin
A or B. Neuropediatrics. 2008;39(4):200-4.
58. Coleski R, Anderson MA, Hasler WL. Factors Associated with Symptom Response to Pyloric Injection of Botulinum Toxin in
a Large Series of Gastroparesis Patients. Dig Dis Sci. 2009 Jan 30. [Epub ahead of print].
59. Reddymasu SC, Singh S, Sankula R, et al. Endoscopic pyloric injection of botulinum toxin-A for the treatment of
postvagotomy gastroparesis. Am J Med Sci. 2009;337(3):161-4.
60. Mirbaheri SA, Sadeghi A, Amouie M, et al. Pyloric injection of botulinum toxin for the treatment of refractory GERD
accompanied with gastroparesis: a preliminary report. Dig Dis Sci. 2008;53(10):2621-6.
61. Friedenberg FK, Palit A, Parkman HP, et al. Botulinum toxin A for the treatment of delayed gastric emptying. Am J
Gastroenterol. 2008;103(2):416-23.
62. Arts J, Holvoet L, Caenepeel P, et al. Clinical trial: a randomized-controlled crossover study of intrapyloric injection of
botulinum toxin in gastroparesis. Aliment Pharmacol Ther. 2007;26(9):1251-8.
63. Ehren I, Volz D, Farrelly E, et al. Efficacy and impact of botulinum toxin A on quality of life in patients with neurogenic
detrusor overactivity: A randomized, placebo-controlled, double-blind study. Scand J Urol Nephrol. 2007;41(4):335-40.
64. Shuhendler AJ, Lee S, Se B, et al. Efficacy of Botulinum Toxin Type A for the Prophylaxis of Episodic Migraine Headaches:
A Meta-analysis of Randomized, Double-Blind, Placebo-Controlled Trials. Pharmacotherapy. 2009;29(7):784-91.
65. Kanovsky P, Slawek J, Denes Z, et al. Efficacy and Safety of Botulinum Neurotoxin NT 201 in Poststroke Upper Limb
Spasticity. Clin Neuropharm 2009;32:259-265.
66. Barnes M, Schnitzler A, Medeiros L, et al. Efficacy and safety of NT 201 for upper limb spasticity of various etiologies – a
randomized parallel-group study. Acta Neurol Scand 2010;122:295–302.
67. Rohrbach S, Junghans K, Köhler S, Laskawi R. Minimally invasive application of botulinum toxin A in patients with
idiopathic rhinitis. Head Face Med. 2009;16;5:18.
68. Kuo HC, Liu HT. Therapeutic effects of add-on botulinum toxin A on patients with large benign prostatic hyperplasia and
unsatisfactory response to combined medical therapy. Scand J Urol Nephrol. 2009;43(3):206-11.
69. Editor’s Note to Authors and Readers: Levels of Evidence coming to
Neurology
®
. Accessed June 21, 2010.
70. Xeomin [prescribing information]. Raleigh, NC: Merz Pharmaceuticals, LLC, September 2023.
71. Silberstein SD, Holland S, Freitag F, et al. Evidence-based guideline update: Pharmacologic treatment for episodic migraine
prevention in adults. Report of the Quality Standards Subcommittee of the American Academy of Neurology and the
American Headache Society. Neurology 2012; 78:1337-1345.
72. Soares A, Andriolo RB, Atallah AN, da Silva EM. Botulinum toxin for myofascial pain syndromes in adults. Cochrane
Database Syst Rev. 2014 Jul 25;7:CD007533.
73. Bohluli B, Motamedi MH, Bagheri SC, et al. Use of botulinum toxin A for drug-refractory trigeminal neuralgia: preliminary
report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011 Jan;111(1):47-50. Epub 2010 Jul 31.
74. Zuniga C, Diaz S, Piedimonte F, et al. Beneficial effects of botulinum type A in trigeminal neuralgia. Arq Neuropsiquiatr.
2008 Sep;66(3A):500-3.
75. Herd CP, Tomlinson CL, Rick C, et al. Botulinum toxins for the prevention of migraine in adults. Cochrane Database Syst
Rev. 2018 Jun 25;6:CD011616.
76. Dressler D. Routine use of Xeomin in patients previously treated with Botox: long term results. European Journal of
Neurology. 2009;16(Suppl 2):2-5.
77. Waseem Z, Boulias C, Gordon A, Ismail F, Sheean G, Furlan AD. Botulinum toxin injections for low-back pain and sciatica.
Cochrane Database of Systematic Reviews
2011, Issue 1. Art. No.: CD008257.
78. Hayes Medical Technology Directory. Botulinum Toxin Treatment for Chronic Tension-Type Headache. December 30,
2011. Accessed on September 6, 2016.
79. Bjornson K, Hays R, Graubert C, et al. Botulinum toxin for spasticity in children with cerebral palsy: a comprehensive
evaluation. Pediatrics. 2007 Jul;120(1):49-58.
80. MCG
™
Care Guidelines. Ambulatory Care 22
nd
Edition. OnabotulinumtoxinA. Accessed on January 13, 2021.

Botulinum Toxins A and B
Page 26 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
81. MCG
™
Care Guidelines. Ambulatory Care 22
nd
Edition. AbobotulinumtoxinA. Accessed on January 13, 2021.
82. MCG
™
Care Guidelines. Ambulatory Care 22
nd
Edition. RimabotulinumtoxinB. Accessed on January 13, 2021.
83. Albanese A, Asmus F, Bhatia KP, et al. EFNS guidelines on diagnosis and treatment of primary dystonias. Eur J Neurol.
2011 Jan;18(1):5-18.
84. Novak I, Campbell L, Boyce M, et al. Botulinum toxin assessment, intervention and aftercare for cervical dystonia and other
causes of hypertonia of the neck: international consensus statement. Eur J Neurol. 2010 Aug;17 Suppl 2: 94-108.
85. Vaezi MF, Pandolfino JE, Vela MF. ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol.
2020 Aug; 115:1393–1411.
86. Hayes Medical Technology Directory. Botulinum Toxin Treatment for Detrusor Instability. December 30, 2011. Accessed on
September 6, 2016.
87. Chancellor MB, Elovic E, Esquenazi A, Naumann M, Segal KR, Schiavo G, Smith CP, Ward AB. Evidence-based review, and
assessment of botulinum neurotoxin for the treatment of urologic conditions. Toxicon. 2013 Jun 1;67:129-40.
88. Naumann M, Dressler D, Hallett M, Jankovic J, Schiavo G, Segal KR, Truong D. Evidence-based review, and assessment of
botulinum neurotoxin for the treatment of secretory disorders. Toxicon. 2013 Jun 1;67:141-52.
89. Simpson DM, Hallett M, Ashman EJ, et al. Practice guideline update summary: Botulinum neurotoxin for the treatment of
blepharospasm, cervical dystonia, adult spasticity, and headache: Report of the Guideline Development Subcommittee of
the American Academy of Neurology. Neurology 2016;86:1-9.
90. Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L, American College of Gastroenterology. Clinical guideline:
management of gastroparesis. Am J Gastroenterol 2013;108:18-37.
91. Camilleri M. Treatment of gastroparesis. UptoDate. Accessed on August 18, 2017.
92. Nitti VW, Dmochowski R, Herschorn S, et al. OnabotulinumtoxinA for the Treatment of Patients with Overactive Bladder and
Urinary Incontinence: Results of a Phase 3, Randomized, Placebo Controlled Trial. J Urol 2017; 197: S216-S223.
93. Kennelly M, Dmochowski, Schulte-Baukloh H, et al. Efficacy and Safety of OnabotulinumtoxinA Therapy are Sustained Over
4 Years of Treatment in Patients With Neurogenic Detrusor Overactivity: Final Results of a Long-Term Extension Study.
Neurourol Urodyn 36:368–375 (2017).
94. Delgado MR, Tilton A, Russman B, et al. AbobotulinumtoxinA for Equinus Foot Deformity in Cerebral Palsy: A Randomized
Controlled Trial. Pediatrics. 2016;137(2):e20152830.
95. Pandey S, Srivanitchapoom P, Kirubakaran R, Berman BD. Botulinum toxin for motor and phonic tics in Tourette's
syndrome. Cochrane Database Syst Rev. 2018 Jan 5;1:CD012285.
96. Stachler RJ, Francis DO, Schwartz SR, et al. Clinical Practice Guideline: Hoarseness (Dysphonia) (Update). Otolaryngol
Head Neck Surg. 2018 Mar;158(1_suppl):S1-S42.
97. Dabrowski, E., Bonikowski, M., Gormley, M., Volteau, M., Picaut, P., & Delgado, M. R. (2018). AbobotulinumtoxinA Efficacy
and Safety in Children with Equinus Foot Previously Treated with Botulinum Toxin. Pediatric neurology, 82, 44-49.
98. Robert, G., Descazeaud, A., Karsenty, G., Saussine, C., Azzouzi, A. R., de la Taille, A., & Benard, A. (2018). Prostatic
injection of botulinum toxin is not inferior to optimized medical therapy in the management of lower urinary tract symptoms
due to benign prostatic hyperplasia: results of a randomized clinical trial. World journal of urology, 36(6), 921-929.
99. Khambati, A., Lau, S., Gordon, A., & Jarvi, K. A. (2014). OnabotulinumtoxinA (Botox) Nerve Blocks Provide Durable Pain
Relief for Men with Chronic Scrotal Pain: A Pilot Open‐Label Trial. The journal of sexual medicine, 11(12), 3072-3077.
100. Castelão, M., Marques, R. E., Duarte, G. S., Rodrigues, F. B., Ferreira, J., Sampaio, C., . & Costa, J. (2017). Botulinum toxin
type A therapy for cervical dystonia. Cochrane Database of Systematic Reviews, (12).
101. Pringsheim, T., Okun, M. S., Müller-Vahl, K., Martino, D., Jankovic, J., Cavanna, A. E., . & Oskoui, M. (2019). Practice
guideline recommendations summary: Treatment of tics in people with Tourette syndrome and chronic tic disorders.
Neurology, 92(19), 896-906.
102. Daxxify [prescribing information]. Newark, CA: Revance Therapeutics, Inc., August 2023.

Botulinum Toxins A and B
Page 27 of 27
UnitedHealthcare Commercial Medical Benefit Drug Policy
Effective 04/01/2024
Proprietary Information of UnitedHealthcare. Copyright 2024 United HealthCare Services, Inc.
Policy History/Revision Information
Date
Summary of Changes
04/01/2024
Applicable Codes
Updated list of applicable HCPCS codes to reflect quarterly edits:
o Removed C9160
o Replaced J3490 and J3590 with J0589
Supporting Information
Archived previous policy version 2024D0017AJ
Instructions for Use
This Medical Benefit Drug Policy provides assistance in interpreting UnitedHealthcare standard benefit plans. When deciding
coverage, the member specific benefit plan document must be referenced as the terms of the member specific benefit plan
may differ from the standard plan. In the event of a conflict, the member specific benefit plan document governs. Before using
this policy, please check the member specific benefit plan document and any applicable federal or state mandates.
UnitedHealthcare reserves the right to modify its Policies and Guidelines as necessary. This Medical Benefit Drug Policy is
provided for informational purposes. It does not constitute medical advice.
This Medical Benefit Drug Policy may also be applied to Medicare Advantage plans in certain instances. In the absence of a
Medicare National Coverage Determination (NCD), Local Coverage Determination (LCD), or other Medicare coverage guidance,
CMS allows a Medicare Advantage Organization (MAO) to create its own coverage determinations, using objective evidence-
based rationale relying on authoritative evidence (Medicare IOM Pub. No. 100-16, Ch. 4, §90.5
).
UnitedHealthcare may also use tools developed by third parties, such as the InterQual
®
criteria, to assist us in administering
health benefits. UnitedHealthcare Medical Benefit Drug Policies are intended to be used in connection with the independent
professional medical judgment of a qualified health care provider and do not constitute the practice of medicine or medical
advice.
