
Employees’ Manual
Title 8, Chapter I Revised April 14, 2023
Medical Institutions

Title 8: Medicaid Table of Contents
Chapter I: Medical Institutions
Revised April 14, 2023 Page 1
Page
Iowa Department of Health and Human Services Employees’ Manual
Overview .................................................................................................................................................. 1
Medicare Coverage for Institutional Care ................................................................................................................. 1
Eligibility ................................................................................................................................................... 2
Who Is Not Eligible ......................................................................................................................................................... 4
Eligibility for the 300% Group ....................................................................................................................................... 5
Eligibility of Blind or Disabled Children in Medical Institutions ................................................................ 6
Preadmission and Resident Review (PASRR) ............................................................................................................ 7
Medical Necessity ............................................................................................................................................................ 7
Continued Stay Reviews ..................................................................................................................................... 8
If Level of Care Is Denied .................................................................................................................................. 8
Approval at a Lower Level of Care ................................................................................................................. 9
Effect of Institutionalization on SSI and FIP Eligibility ............................................................................................ 10
How SSI Eligibility Is Affected .......................................................................................................................... 10
How FIP Eligibility Is Affected ......................................................................................................................... 11
Income and Resources of Married Persons ........................................................................................ 12
Determining if a Common-Law Marriage Exists .................................................................................................... 14
When Both Spouses Are in an Institution ............................................................................................................... 15
Living in the Same Room .................................................................................................................................. 15
Living in Different Rooms................................................................................................................................. 17
When Applying for or Receiving Waiver or PACE Services .............................................................................. 18
Client Participation ............................................................................................................................... 18
Income Available for Client Participation ................................................................................................................ 19
Income Exempt From Client Participation .............................................................................................................. 22
Non-MAGI-Related Members ......................................................................................................................... 22
Deductions From Client Participation ...................................................................................................................... 25
Ongoing Personal Needs Allowance ............................................................................................................. 26
Earned Income .................................................................................................................................................... 27
Personal Needs Expenses in the Month of Entry ....................................................................................... 28
Personal Needs in the Month of Discharge ................................................................................................. 29
Deduction for the Maintenance Needs of Spouse and Dependents ..................................................... 30
Deduction for Unmet Medical Needs ........................................................................................................... 37
If Client Participation Exceeds the Facility’s Medicaid Rate ................................................................................ 38
Client Participation for Skilled Care ......................................................................................................................... 39
Members With a Medical Assistance Income Trust (MAIT) ............................................................................... 40
125 Percent of the Statewide Average Charge for Care ......................................................................... 41
Trust Payments ................................................................................................................................................... 42
Determination of Client Participation ........................................................................................................... 44
Other Third-Party Payments ....................................................................................................................................... 51
Changes in Client Participation .................................................................................................................................. 52
If Lower Level of Care Is Needed .................................................................................................................. 53
Effect of Buy-In .................................................................................................................................................... 54
If the Member Receives a Lump Sum ............................................................................................................ 56
If the Member Leaves or Transfers Facilities .............................................................................................. 57

Title 8: Medicaid Table of Contents
Chapter I: Medical Institutions
Revised April 14, 2023 Page 2
Page
Iowa Department of Health and Human Services Employees’ Manual
Qualified Medicare Beneficiaries in Skilled Care .............................................................................. 60
Client Participation for QMBs Entering Skilled Care ............................................................................................ 61
Billing and Payment .............................................................................................................................. 64
Provider Rates ................................................................................................................................................................ 65
Billing Process ................................................................................................................................................................. 65
Payment for Reserve Bed Days .................................................................................................................................. 66
Nursing Facilities ................................................................................................................................................ 66
ICFs/ID .................................................................................................................................................................. 67
When Reserve Bed Days Are Paid Privately ............................................................................................... 67
No Supplementation of Payment Allowed .............................................................................................................. 67
Payment for Inpatient Hospitals Who Require a Lower Level of Care ........................................................... 68
Payment for Transferring a Resident by Ambulance ............................................................................................. 68
Billing and Payment for Hospice Members .............................................................................................................. 69
Use of IoWANS ..................................................................................................................................... 69
Important Facts About IoWANS for Facility Programs ....................................................................................... 70
Facility Administrative Information ................................................................................................... 71
Reporting Changes in a Resident’s Status ................................................................................................................ 71
Transfers and Discharges ............................................................................................................................................. 71
Resident Trust Account ............................................................................................................................................... 72
If a Facility Closes ........................................................................................................................................................... 72
If Facility Ownership Changes .................................................................................................................................... 73

Title 8: Medicaid Page 1
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Overview
Revised April 14, 2023 Verification of Income
Overview
This chapter explains the eligibility, income, and resource policies that are unique for people in medical
institutions. Following an explanation of how Medicare pays for people in medical institutions, there is a
section on who is and is not eligible for Medicaid payment of medical institution care. Also included in this
section is information about how institutionalization may affect a person’s eligibility for other benefits.
Because income and resource policies are different for married people, these policies are outlined in the next
section. Once the member is determined eligible, client participation is then calculated using the policies and
procedures listed in the section that follows.
The balance of the chapter is devoted to administrative issues, such as billing, that are used when handling
cases involving Medicaid members in medical institutions.
The section on billing and payment includes information about using the Institutional and Waiver
Authorization and Narrative System (IoWANS) for authorization of facility payments.
Medicare Coverage for Institutional Care
To receive Medicare reimbursement for institutional care, a facility must be certified to provide:
▪ Care in an acute hospital setting,
▪ Care in a psychiatric hospital for patients age 65 and older, or
▪ Skilled nursing care.
Nursing facilities that provide the skilled level of care must also be certified to participate in the
Medicare program. Because of this requirement, many Medicaid members’ skilled nursing care is first
paid by Medicare. (Other resources, including Medicare, must be used before any Medicaid payment is
made.)
Medicare coverage limits are based on a “benefit period.” Medicare defines a benefit period as
beginning the day the person enters the hospital as an inpatient and ending after the person has not
been in a hospital or skilled nursing facility for 60 days. If the person returns to the hospital or skilled
care in less than 60 days, this is not a new benefit period. Any remaining days in the current benefit
period are used.
Medicare coverage of hospital care is as follows:
▪ For the first 60 days of each benefit period, full payment is made after the beneficiary pays a
deductible.
▪ For days 61 through 90, beneficiaries pay a daily coinsurance.
▪ After 90 days in the hospital for a single benefit period, beneficiaries may draw on their “lifetime
reserve.” The lifetime reserve is 60 days and is nonrenewable. Beneficiaries must pay a
coinsurance.
▪ After 150 days (or 90 days if the lifetime reserve has been exhausted), Medicare makes no further
payment.

Title 8: Medicaid Page 2
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Overview
Revised April 14, 2023 Medicare Coverage for Institutional Care
At the skilled level of care, Medicare covers 100 days per benefit period if the person has been
hospitalized for at least three days within 30 days of entering skilled care. Medicare pays the full cost
for days 1 through 20. For days 21 through 100, Medicare pays the full cost except for a daily
coinsurance, which is paid by the beneficiary. After 100 days, Medicare skilled care payment stops until
the next benefit period begins.
Mr. B enters the hospital on January 5. After being hospitalized for four days, he returns home. He
enters skilled care on February 1 and stays there until May 15. He is eligible for 100 days of Medicare
skilled nursing coverage (20 days of full coverage and 80 days of coinsurance). Medicare coverage
ends May 11.
On July 1, Mr. B returns to the hospital. After three days in the hospital, he reenters skilled care. Mr.
B is not eligible for any more Medicare skilled nursing coverage, because he has not been outside of a
hospital or skilled care long enough to begin a new benefit period.
Medicare coverage of care in a psychiatric hospital is as follows:
▪ There is a lifetime payment limit of 150 days for people who entered a mental health institute
(MHI) before January 1, 1989, and did not have a break in their benefit period. (A patient breaks
the benefit period by returning home or being placed in a hospital.)
▪ For a person who entered an MHI after January 1, 1989, the lifetime limit is 190 days.
Medicare does not cover the cost of care in a nursing facility for people with mental illness, an
intermediate care facility for people with an intellectual disability (ICF/ID), or a psychiatric medical
institution for children (PMIC).
Eligibility
Legal reference: 42 CFR 435.911, 441 IAC 76 (Rules in Process)
Unless otherwise specified in this chapter, application policies and general eligibility requirements are the
same for people living in a medical institution as for any other applicant. Follow processing procedures
described in 8-B, Application Processing and eligibility requirements in 8-C, Nonfinancial Eligibility, 8-D, Resources,
8-E, Income, and 8-F, Coverage Groups.
A person who is not currently a Medicaid member must file an application as defined in 8-B, Which Application
Form to Use.
Residents of medical institutions must also:
▪ Meet specific income and resource guidelines for single and married couples.
▪ Need the level of care provided by the medical institution. See Medical Necessity.
▪ Have lived in an institution for 30 consecutive days if in the 300% eligibility group.
Title 8: Medicaid Page 3
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Eligibility
Revised April 14, 2023
Reassess eligibility for a Medicaid member who enters a medical institution to determine if the member
meets these additional eligibility requirements. (You do not need to reassess eligibility when a member enters
an acute-care hospital unless the member expects to stay or stays more than 30 days.) A new application is
not required, unless the person is at the end of a Medically Needy certification period, or the certification
period will end within the 30-day stay requirement.
Mr. W is eligible for Medically Needy with a certification period of May and June. He enters the nursing
home on June 5. He is not eligible for nursing facility payment until he meets the requirements of the 300%
group because he is over income. Mr. W must file an application.
Even if an application is not needed, evaluate income and resources of the client as well as the other
requirements for facility payment. Entering a facility can change the household unit, deeming policies, and
countable resources and income. See Effect of Institutionalization on SSI and FIP Eligibility.
A Non-MAGI member who is eligible for full Medicaid before entering the facility does not need to meet the
30-day-stay requirement for nursing facility approval in the month of entry. However, a redetermination is
required before facility eligibility can be approved for ongoing months. A member, who is redetermined to
the 300% group, must meet the 30-day-stay requirement before ongoing eligibility is approved.
MAGI-related members are not eligible for payment of long term care services. Exception: Children under
the age of 21 who meet eligibility under the 300% group. In the month of entry, the income of the parents is
counted. If the child continues to be institutionalized in the month after the month of admission, the child is
considered as an individual. The income of the parents is not counted or deemed to the child.
Newborns who do not leave the hospital or who are transferred to another medical institution are
considered as individuals. When a newborn is not discharged home but goes directly to another medical
facility, the income of the parents is not counted or deemed to the child.
Newborns who are discharged home but return to the hospital or some other medical institution are
considered part of the household in the month of admission. The income of the parents is counted or
deemed in the month of entry. If the child continues to be institutionalized in the month after the month of
admission, the child is considered as an individual. The income of the parents is not counted or deemed to
the child.
Count resources according to 8-D, Resource Eligibility of Children.
The 30-day stay requirement applies to people in the 300% group only. Medicaid members who are
automatically redetermined to another coverage group to cover the cost of facility care do not need to meet
the 30-day-stay requirement unless they are redetermined to the 300% group.

Title 8: Medicaid Page 4
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Eligibility
Revised April 14, 2023 Who Is Not Eligible
A MEPD member enters a nursing facility on April 15. The member is eligible for nursing facility assistance in
the month of entry. The IM worker redetermines eligibility for ongoing months and finds that the member
meets level of care requirements, is over the 300% limit, but continues to be eligible for MEPD. The
member is eligible for nursing facility assistance for ongoing months because the member meets level-of-care
requirements and remains eligible for Medicaid in a full coverage group.
Assess client participation as specified in Client Participation for all members.
For ICF/ID, see 6-Appendix for instructions on completing the required form, ICF/ID Residential Care
Agreement, form 470-0374.
Medicaid eligibility may be established for a person who lives in a medical institution that does not participate
in the Medicaid program, even though no Medicaid payment will be made to the facility. Determine income,
resources, and level of care as though the institution were participating in Medicaid.
The Iowa Medicaid Enterprise Medical (IME) Medical Services Unit will do a level of care determination for a
person in a facility that is not Medicaid-certified. If the person does not meet the facility’s level of care,
determine eligibility as if the person lived at home.
The following sections give more information on:
▪ Who is not eligible for Medicaid payment of institutional care
▪ Eligibility under the 300% coverage group
▪ Determination of medical necessity for institutional care
▪ The effect of institutionalization on SSI and FIP eligibility
Who Is Not Eligible
Legal reference: 441 IAC 75 (Rules in Process)
Eligibility under most coverage groups includes eligibility for Medicaid medical institution payment if the
medical necessity requirements are met. Exceptions are as follows:
▪ The Medically Needy coverage group does not provide for payment for nursing care, skilled care,
ICF/ID or NF/MI care, or care in psychiatric institutions.
▪ The qualified Medicare beneficiary (QMB) coverage group provides limited coverage for hospital
and skilled nursing care and no coverage for nursing care or ICF/ID care. Only Medicare
premiums, coinsurance, and deductible are covered.
▪ The qualified disabled and working persons (QDWP) coverage group provides Medicaid payment
only for Medicare Part A premiums.
▪ The specified low-income Medicare beneficiary (SLMB) and the expanded specified low-income
Medicare beneficiary (E-SLMB) coverage groups provide Medicaid payment only for Medicare Part
B premiums.

Title 8: Medicaid Page 5
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Eligibility
Revised April 14, 2023 Who Is Not Eligible
Examine such cases to determine if the members would be eligible for institutional care payment if in
another coverage group. Obtain a new application only if a Medically Needy certification is about to
end.
Eligibility for the 300% Group
Legal reference: 441 IAC 75 (Rules in Process)
The 300% group is an eligibility group used for a person in a medical institution who meets all the
following requirements:
▪ Has countable income less than or equal to 300% of the SSI benefit amount.
▪ Meets level of care requirements as determined by the Iowa Medical Enterprise (IME). See Medical
Necessity.
▪ Receives care in a hospital, nursing facility, psychiatric medical institution, or ICF/ID for 30
consecutive days.
▪ The person is age 65 or older, blind, disabled, or is under the age of 21.
▪ Meets all SSI eligibility requirements except income. EXCEPTION: Do not consider resources for
children under 21.
For more information about the 300% group, see 8-F, People in Medical Institutions: 300% Income Level.
Do not approve eligibility until after the applicant has lived in an institution for at least 30 consecutive
days. Eligibility begins no earlier than the first day of the month in which the 30-day period began. The
period begins at 12 a.m. on the day of admission and ends no earlier than 12 midnight of the thirtieth
day following the beginning of the period.
Only one 30-day period is required to establish eligibility. Discharge during a subsequent month,
creating a partial month of care, does not affect eligibility for that partial month, regardless of whether
the eligibility determination was completed before discharge.
If the person dies before completing the 30-day period, consider the person to have met the 30-day
requirement.
The 30-day stay requirement applies to the 300% group only. Medicaid members who are automatically
redetermined to another coverage group to cover the cost of facility care do not need to meet the 30-
day-stay requirement unless they are redetermined to the 300% group.
A temporary absence of not more than 14 full consecutive days does not interrupt the 30-day period if
the person remains under the jurisdiction of the institution. The person must first have been physically
admitted to the institution.
Do not wait until after the 30-day period is over to verify other eligibility factors such as income and
resources.

Title 8: Medicaid Page 6
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Eligibility
Revised April 14, 2023 Eligibility for the 300% Group
1. The client enters a nursing facility at 4:00 p.m. on September 5 and remains there. An application
for Medicaid is received on September 12. The 30-day period of residency is met on October 4.
Eligibility can be established on October 4, effective September 1, assuming all other eligibility
factors are met. There is no eligibility for a prior period under the 300% coverage group.
2. The client enters a hospital at noon on August 1, transfers to a nursing facility August 15, and
remains there until October 15. An application is received September 15. Eligibility can be
established effective August 1 for the 300% group, assuming all other eligibility factors are met.
3. The client enters the hospital on August 15 and leaves September 15. The client is eligible for
Medicaid under the 300% group effective August 1. Eligibility for the 300% group ends September
30, providing timely notice is given.
4. The client has been a private-pay patient at a nursing facility for several years. An application for
Medicaid is received August 10. Eligibility can be established retroactive to May 1, assuming all
other eligibility factors are met.
5. The client enters a nursing facility on July 31 and is discharged September 10. Eligibility can be
established for July, August, and September, assuming all other eligibility factors are met.
6. The client enters the hospital March 31, leaves the hospital on April 14, and returns to the
hospital April 16. The client is not eligible, since the client was not in the hospital for 30
consecutive days. The client must establish the 30-day period in the medical institution starting
April 16 up to and including May 15 to be eligible for the 300% group.
People with income in excess of 300% of the SSI benefit for one person may qualify for Medicaid
payment for institutional care using a medical assistance income trust. See Members With a Medical
Assistance Income Trust (MAIT).
Eligibility of Blind or Disabled Children in Medical Institutions
Legal reference: 42 CFR 435.725, 441 IAC 75 (Rules in Process)
A blind or disabled child under age 18 (or under age 22 if a student) may be eligible for
institutional care. The child is eligible for the month of birth if all other eligibility factors are met.
Count the income of the parents for the month the child entered the institution if the child lived
with the parents for part of that month. See 8-E, Deeming SSI-Related Income for a description of
the deeming process between parents and children.
Effective with the first full calendar month of institutionalization, consider only the income and
resources of the child when determining Medicaid eligibility. A child who is born in a medical
institution and does not leave the institution during the month of birth is considered a resident
of the institution for a full calendar month. Count only the child’s income when determining
eligibility.
For treatment of resources, see 8-D, Resource Eligibility of Children.
The income and resources of the parents are not deemed to the child until the month following
the month of discharge.

Title 8: Medicaid Page 7
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Eligibility
Revised April 14, 2023 Eligibility for the 300% Group
3-20-03
4-10-03
Child is born in hospital
Child leaves hospital for parent’s home
The parents’ income is not considered in determining eligibility for March and April.
Preadmission and Resident Review (PASRR)
All individuals entering a Medicaid-certified nursing facility must have a Preadmission Screening and
Resident Review (PASRR) completed. PASRR is a federally required process to ensure that individuals
with intellectual disabilities or mental illness are appropriately screened, evaluated, placed in nursing
facilities when appropriate; and if placed in a nursing facility, are receiving all services necessary to meet
the resident’s needs. A PASSR must be completed prior to an individual being admitted into a nursing
facility.
All nursing facilities in Iowa are required to use the PathTracker system to enter resident admissions,
transfers, and discharges. PathTracker data is used to generate form 470-5386, PASRR Case Activity
Report.
Medical Necessity
Legal reference: 441 IAC 78.3(249A), 441 IAC 81.3(249A), 441 IAC 81.7(249A), 441
IAC 82.7(249A), 441 IAC 82.8(249A), 441 IAC 85.7(2)
A person is eligible for Medicaid payment for care in a long term care facility or psychiatric institution
only if the level of care provided is determined to be reasonable, medically necessary, and appropriate.
A level of care determination is required when a person enters a facility or moves to a different level
of care. Use the Case Activity Report to determine who will be making the level of care determination.
Review the form to verify the date of the member’s admission to the facility and Medicare coverage.
The Iowa Medicaid Enterprise (IME) Medical Services Unit or the MCO determine whether the person
needs the level of care provided by a medical institution. However, when a person is eligible for
Medicare and admits into a facility using their Medicare skilled nursing benefit, the Medicare
intermediary makes the determination. Accept a level of care determination completed for Medicare
purposes for determining Medicaid eligibility. A person who has been approved for Medicare at a
particular level of care is eligible for the same level of care under Medicaid. The facility should submit a
new Case Activity Report when Medicare benefits are exhausted. To begin the process, make entries
to pend the facility program in the Automatic Benefit Calculation (ABC) system. This initiates the level
of care determination.
The IME Medical Services Unit nurse reviewer or the MCO makes a level of care determination based
on the information provided and enters the decision in IoWANS. IoWANS documents the level of
care approval and effective date.

Title 8: Medicaid Page 8
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Eligibility
Revised April 14, 2023 Medical Necessity
If a member has requested retroactive eligibility to cover cost of medical institution care, check to see
if the IME Medical Services Unit has made a retroactive determination. A person may have needed
institutional care in the retroactive period even if such care is not medically necessary now.
If the member meets all other eligibility requirements and the level of care is medically necessary,
complete ABC entries for an eligibility determination. See 14-B(9). For more information, see 14-M,
IoWANS User Guide for specific enrollment processes.
See If Level of Care Is Denied for procedures when the IME Medical Services Unit finds that the person
does not need the level of care requested.
NOTE: When a person requests Medicaid payment for skilled nursing care in an out-of-state facility,
refer the facility to the Bureau of Medical and Long Term Services and Supports for approval of
payment. Also discuss the waivers and programs for all-inclusive care for the elderly (PACE) with these
applicants and request waiver slots if appropriate. (A person receiving Iowa Medicaid payment in an
out-of-state facility is still considered an Iowa resident and can be put on waiver waiting lists.)
Continued Stay Reviews
Legal reference: 441 IAC 78.3(249A), 441 IAC 81.3(1), 441 IAC 81.7(249A), 441 IAC
82.8(249A), 441 IAC 85.7(2)
An initial medical necessity determination does not ensure continued eligibility. The IME Medical
Services Unit or the MCO will review the member’s level of care within 90 days after admission.
A member must continue to need the level of institutionalized care provided in order to ensure
continued eligibility.
Assume that the level of care continues to be approved as long as the member stays at the same
level of care. The IME Medical Services Unit will notify you of any change in the level of care.
See If Level of Care Is Denied for procedures when the IME Medical Services Unit finds that the
member does not need the level of care received. If a continued-stay review denies the current
level of care, but the member continues to need care in a medical institution, eligibility can
continue with payment at the lower level of care. See Approval at a Lower Level of Care.
If Level of Care Is Denied
Legal reference: 441 IAC 81.3(1)
If the applicant does not need a level of medical institution care or needs a lower level than
requested, the IME Medical Services Unit or the MCO issues a denial letter to the applicant, the
physician, the facility, and the Bureau of Medical and Long Term Services and Supports. IoWANS
will notify you if level of care is denied.

Title 8: Medicaid Page 9
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Eligibility
Revised April 14, 2023 Medical Necessity
The client may file an appeal if the client disagrees with the IME decision. Appeal requests should
be sent to the Department’s Appeals Section following the normal appeal procedure in 1-E,
Appeals and Hearings. IME staff will review the previous denial and complete an internal
reconsideration in preparation for the appeal.
When level of care is denied, the application for payment of nursing facility care should be
denied. People in the 300% group must need institutional care as a condition of eligibility. People
who qualify under other coverage groups may be eligible for general Medicaid services even if
they are not eligible for Medicaid payment for their institutional care.
1. Mr. P has lived in a nursing facility for four years and has gross income of $700 monthly.
He applies for Medicaid March 1. IME determines that Mr. P does not need care in a
medical institution. He is not eligible for Medicaid payment for nursing care. Medicaid
eligibility under other coverage groups is examined.
2. Mrs. W has been receiving skilled care for three months when she applies for Medicaid
November 5. IME determines that Mrs. W does not need skilled care, but does need
nursing care. Ms. W meets all other eligibility factors. The application is approved for
medical institution care at the nursing care level.
If a person files a timely appeal of a level of care denial in a continued stay review, continue
assistance pending the decision.
If the appeal decision upholds the IME denial, examine the case to determine if the client is
eligible for another Medicaid coverage group that does not depend on institutional residence
(e.g. Medically Needy or qualified Medicare beneficiary). If so, payment will be made for other
services. No payment will be made for facility care. Enter the aid type the person would have if
living at home.
Ms. A is a Medicaid member in a nursing facility. She is in the 300% group and has income of
$900 per month. She is denied nursing level of care and receives the final decision June 3 that
she no longer needs care in a medical institution. Her case is canceled effective July 1 for the
300% group. She is automatically determined eligible for the Medically Needy coverage group.
Approval at a Lower Level of Care
Legal reference: 441 IAC 81.10(4)“g,” 441 IAC 78.3(6), 441 IAC 78.3(14)
If the IME Medical Services Unit or the MCO determines that a person needs a lower level of
care, the client must seek placement in the correct level of care. The social worker at the facility
is responsible for finding another placement if the current facility does not offer the lower level
of care.
If an alternative placement is not available, payment may be made at the lower level if the facility
agrees to accept it. When the facility agrees to accept payment at the rate for the certified lower
level of care, continue to use the same aid type entered for the original level of care.

Title 8: Medicaid Page 10
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Eligibility
January 2, 2015 Medical Necessity
Mr. N is initially approved for nursing level of care. At the continued stay review, he is
determined to need residential level of care. Payment can continue at the residential care
facility rate. The case continues under the nursing facility aid type and vendor number used
before the denial of level of care.
If the facility will not accept the lower payment rate, approve Medicaid in the aid type the person
would be in if living at home.
NOTE: ICFs/ID and PMICs offer care that is not primarily nursing care. IME does not usually
certify a lower level of care for people in these facilities.
Effect of Institutionalization on SSI and FIP Eligibility
How SSI Eligibility Is Affected
Legal reference: 20 CFR 416.211, 20 CFR 416.414
Entry into a medical institution may affect SSI eligibility including the benefit amount and deeming
policies. When an SSI recipient enters a medical institution, notify the Social Security
Administration district office using form 470-0641, Report of Change in Circumstances - SSI-Related
Programs. This allows Social Security to review the payment.
When an SSI recipient enters a public or private medical institution in which Medicaid pays more
than 50% of the cost of care, different SSI benefits rates apply. The person is entitled to the full
SSI benefit rate for any month in which the person is out of the institution for part of the month.
The SSI benefit rate drops to $30 effective with the first full calendar month that the person is in
the institution. For many people in institutions, this policy results in loss of SSI benefits. If SSI
benefits continue, then Medicaid eligibility can continue without completing a review.
Recipients who lose SSI eligibility because they enter the institution must complete an
application. This form is for purposes of review and is not an application. Complete an automatic
redetermination to see if the person meets the requirements of another Medicaid coverage
group.
When Medicaid is not paying at least 50% of the cost of private institutional care for an SSI
recipient, the person continues to receive full SSI benefits as though the person were in an
independent living arrangement. The Social Security Administration determines who is paying
50% of the cost of care. When SSI continues, the person retains Medicaid eligibility by virtue of
the receipt of SSI benefits.

Title 8: Medicaid Page 11
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Eligibility
Revised April 14, 2023 Effect of Institutionalization on SSI and FIP Eligibility
When an SSI recipient enters a public medical institution, such as a state mental health institute,
SSI benefits end effective with the first full calendar month the person lives in the institution,
unless Medicaid is paying at least 50% of the cost. EXCEPTIONS:
▪ Full SSI benefits continue for up to three months, even if Medicaid pays 50% of the cost of
care, when a doctor verifies that the stay will be less than three months.
▪ People who perform substantial gainful activity receive the full SSI benefit for two full
months after entry to a medical institution.
When SSI recipients aged 22 through 64 enter a mental health institution, they lose SSI eligibility
after being in the institution for a full calendar month.
The Social Security Administration stops deeming income and resources from ineligible parents
to an eligible child effective the month after the month the child enters a medical institution.
When both members of a married couple receive SSI and one enters a medical institution, the
Social Security Administration considers them a couple for the month of entry. They are
considered separately the next month for SSI. Medicaid policy considers each member of the
couple for attribution even though one or both members may be on SSI.
1. Mr. W, age 65, enters a mental health institute and applies for Medicaid. His income is
$100 per month. He would be eligible for SSI outside the institution, but the SSI benefit
level changes to $30 since Medicaid is expected to pay more than 50% of the care, and his
income is in excess of that amount. He is eligible under the coverage group “eligible for SSI
but for living in a medical institution.”
2. Mr. J, an SSI recipient, age 32, enters a county hospital in its swing-bed unit. There is an
initial level-of-care denial. Mr. J has insurance that pays the swing-bed. Since Medicaid does
not pay 50% of the cost of care, Mr. J is canceled from SSI. However, Medicaid continues
under the coverage group for persons ineligible for SSI because of requirements that do
not apply to Medicaid, because Mr. J meets all other SSI requirements.
How FIP Eligibility Is Affected
Legal reference: 441 IAC 41.23(3)“b”
Entry into a medical institution may affect Family Investment Program (FIP) eligibility. Examine
eligibility to determine if the person who enters the medical institution continues to meet the
FIP definition of “living with.” See 4-C, Temporary Absence in a Medical Institution.
The person is not a part of the FIP eligible group at home if the person is not expected to return
within one year from either:
▪ The date of application, if the person is not a current member, or
▪ The date of entry to a medical institution, if the person is a current member.
If the person is not “living with” the family at home, determine eligibility of the person in a
medical facility separately.

Title 8: Medicaid Page 12
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Eligibility
Revised April 14, 2023 Effect of Institutionalization on SSI and FIP Eligibility
If a MAGI-related person loses eligibility under the previous coverage group, examine eligibility
under a Non-MAGI-related coverage group. Examine eligibility under the 300% group for a child
under 21.
If a parent is 21 or older, determine if the family would be eligible for FIP if the person were to
live at home.
Income and Resources of Married Persons
Legal reference: 441 IAC 75 (Rules in Process)
If a spouse in an institution is expected to stay at least 30 consecutive days, some eligibility factors are
considered differently. These include:
▪ Determining income from property.
▪ Division of income for Non-MAGI-related groups.
▪ Attribution of resources to an institutionalized spouse and a community spouse. (There is no attribution
for single persons.)
▪ Different income and resource policies for spouses who entered an institution before September 30,
1989, and those who entered on or after that date.
Determine the anticipated length of institutionalization for new applicants. Verify with a physician that the
stay is expected to last at least 30 consecutive days if the client is unsure or the information is questionable.
Eligibility factors are also different depending upon whether one or both spouses are in an institution and
whether they share a room. This section deals with the different requirements based on length of stay and
living arrangements.
When one spouse is in an institution, treatment of income and resources depends upon the spouse’s
situation, as explained in the following chart:
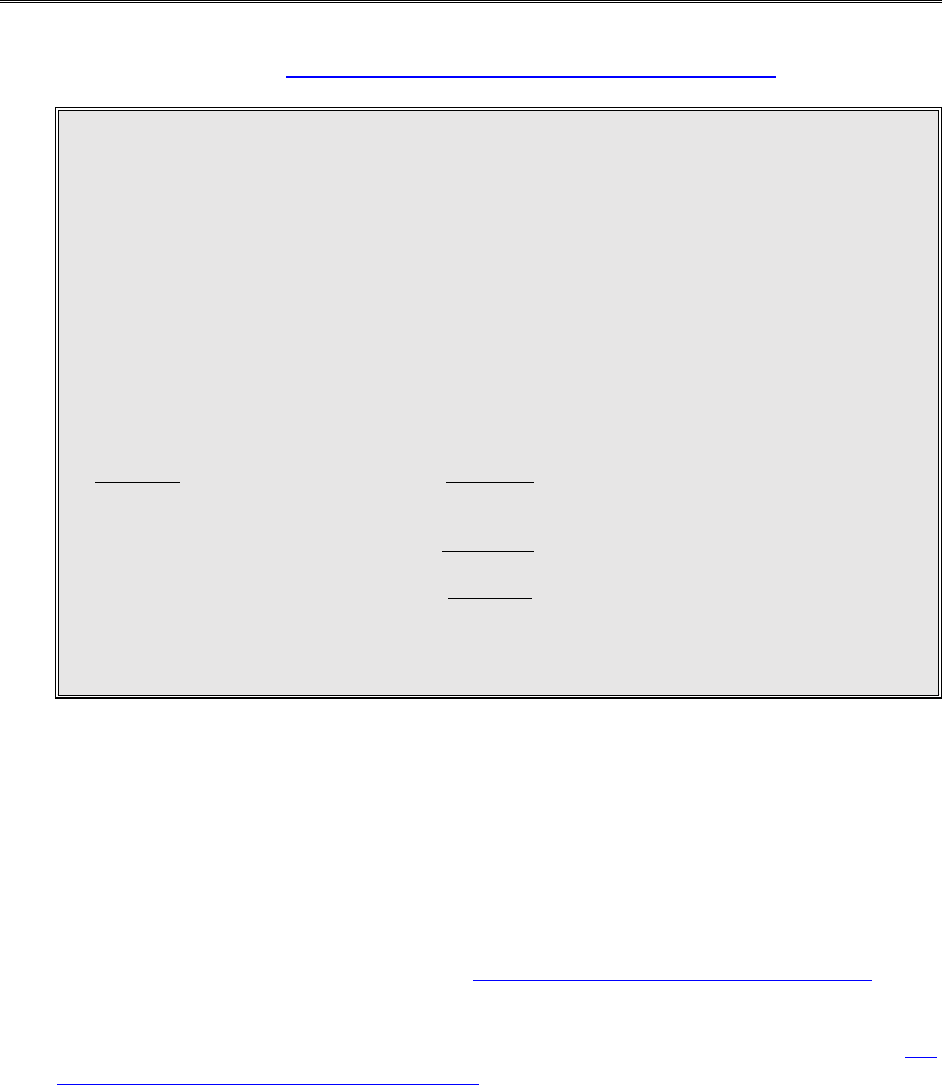
WHEN ONE SPOUSE IS IN AN INSTITUTION
Expected stay of less than 30 days:
Income: Compare household income to SSI
limit for couple when determining eligibility.
Resources: Compare household resources to SSI
limit for a couple when determining eligibility.
Mrs. M enters skilled care after a hip injury, expecting to stay about 20 days. Mr. M, her spouse, is at
home. Mr. and Mrs. M have gross income of $600 monthly and countable resources of $6,000. Mrs.
M’s eligibility is determined with Mr. M, since she is not expected to remain in a medical institution
30 consecutive days. They may be eligible under the Qualified Medicare Beneficiary group or
Medically Needy (for services other than skilled care).

Title 8: Medicaid Page 13
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Income and Resources of Married Persons
Revised April 14, 2023
Expected stay of less than 30 days, but stay exceeds 30 days:
Income: Count only the institutionalized
spouse’s income to determine eligibility and
client participation. May divert income to the
community spouse to raise income to minimum
monthly maintenance needs allowance
(MMMNA).
Resources: Complete an attribution.
In an institution on or after September 30, 1989, for 30 days or more:
Income: Count only the institutionalized
spouse’s income to determine eligibility and
client participation. May divert income to the
community spouse to raise income to
MMMNA.
Resources: Complete an attribution.
Institutionalized spouse returns home, but community spouse enters facility and expects to
stay 30 days or more:
Income: Count only the newly institutionalized
spouse’s income to determine eligibility and
client participation. May divert income to the
community spouse to raise income to
MMMNA.
Resources: Complete an attribution for new
institutionalized spouse and new community spouse.
Marries a community spouse before eligibility is established:
Income: Count only the institutionalized
spouse’s income to determine eligibility and
client participation. May divert income to the
community spouse to raise income to
MMMNA.
Resources: Complete an attribution for new
institutionalized spouse and new community spouse
as of the date of entry into the medical institution.
Marries a community spouse after eligibility is established:
Income: Count only the institutionalized
spouse’s income to determine eligibility and
client participation. May divert income to the
community spouse to raise income to
MMMNA.
Resources: Compare the institutionalized spouse’s
resources to the single-person limit. Do not count
community spouse’s resources to institutionalized
spouse. Complete an attribution for the new
institutionalized spouse and new community spouse
only if the institutionalized spouse’s assistance is
canceled and reapplication is made.

Title 8: Medicaid Page 14
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Income and Resources of Married Persons
Revised April 14, 2023 Determining if a Common-Law Marriage Exists
Institutionalized person marries another institutionalized person:
Income: Treat as individuals or a couple per
client request and client advantage. If treated as
a couple, compare total gross income to 2 x
300%. If treated as individuals, income limit of
300% for each person.
Resources: Treat as individuals or a couple per
client request and client advantage. If treated as a
couple, add resources, compare to $3,000 limit. If
treated as individuals, resource limit is $2,000 for
each person.
Determining if a Common-Law Marriage Exists
Legal reference: Legislative Guide to Marriage Law/Iowa Legislative Services Agency at
https://www.legis.iowa.gov/docs/central/guides/marriage.pdf;
IowaLegalAid.org at http://www.iowalegalaid.org/resource/common-law-marriage-in-
iowa
When determining if someone has a spouse, there may be situations where a common-law marriage
exists or the applicant or member claims a common-law marriage exists. Accept a couple’s claim that a
common-law marriage exists unless you have reason to question the claim. If you question the claim, a
common-law marriage exists if both people:
▪ Mutually agree they are married (they are not free to marry someone else).
▪ Live together continuously or lived together continuously before one member entered a medical
institution.
▪ Publicly declare and present themselves to be married.
The following items can further indicate that a common-law marriage exists:
▪ Joint income tax forms
▪ Joint purchase of property (house, car, etc.)
▪ Mortgages or loans
▪ Insurance policies
▪ School records
▪ Employment records
▪ Birth records
▪ Joint bank accounts
▪ Statements to friends or relatives
▪ Hotel or motel registrations
▪ Wear wedding bands
Evidence must represent the couple as married. One item is generally not enough evidence, but several
items might indicate a common-law marriage.
A common-law marriage is a legal and valid marriage. When a common-law marriage exists, treat the
adults the same as any other married couple.

Title 8: Medicaid Page 15
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Income and Resources of Married Persons
Revised April 14, 2023 Determining if a Common-Law Marriage Exists
1. Mr. Brown applies for nursing facility care. Mr. Brown and Ms. Smith have lived together for 25
years. They have purchased several properties together, including the home they live in. They
have a joint bank account.
Mr. Brown requests that an attribution be completed because he states they are common law.
There is no evidence that they have publicly declared or presented themselves as married. They
have always filed individual income tax returns.
Since they have never publicly declared or presented themselves as married and never filed a
joint return, evidence shows they are not common law. Do not complete an attribution.
2. Sally and John complete an application for facility care. John is listed as the spouse. Sally enters a
medical institution on April 14.
In a phone conversation with John, he states they have a common-law marriage. Sally and John
have publically declared they are husband and wife. John has Sally listed on his employment
application as his wife. This creates a presumption that a common-law marriage exists.
The worker completes an attribution of resources. When Sally is resource-eligible, John will be
allowed a spousal diversion, if applicable.
When Both Spouses Are in an Institution
When both spouses are institutionalized and living in different facilities, treat each as a single individual.
Do not count the income and resources of one spouse to determine the eligibility of the other spouse.
When both spouses are in the same institution, treatment of income and resources depends upon
whether the spouses are living in the same room or in different rooms, as explained below.
Living in the Same Room
Legal reference: 441 IAC 75 (Rules in Process)
If spouses live in the same room in a medical institution, treat their income as a couple from the
month the first spouse entered the medical institution until the last day of the sixth calendar
month in which the first spouse continuously lived in the facility. The six-month period that the
couple must be treated together begins with the month following the month of entry into the
institution when both spouses enter in the same month. When spouses enter the same room at
different times, see When a Spouse Moves Into the Same Room.
To be eligible for Medicaid, the couple’s combined income cannot be more than two times the
300% limit of the SSI benefit for a single person. Use the SSI resource limit for a married couple.
After Six Months
Effective the first day of the seventh calendar month, spouses can choose to be treated
individually. If they chose to be separate, the income of each spouse cannot exceed 300%
of the SSI benefit for one, and the resource limit is $2,000 for each person.

Title 8: Medicaid Page 16
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Income and Resources of Married Persons
Revised April 14, 2023 When Both Spouses Are in an Institution
The couple can continue to be treated as a couple after six months if:
▪ They choose to be considered together, or
▪ One spouse would be ineligible for Medicaid or would receive reduced benefits by
considering them separately.
People treated together as a couple for income and client participation must be treated as
a couple for resources. People treated individually for income and client participation must
be treated individually for resources.
1. Mr. and Mrs. J, a married couple, enter the same room in a nursing facility on June
13. Mr. J has gross income of $950, and Mrs. J has gross income of $675. Their
combined income of $1,625 is compared to twice the 300% income limit for June
through December. In January, they choose to be separate and their respective
incomes are compared to the single-person gross income limit.
They have countable resources of $3,000 in a joint checking account. For June
through December, their resources are combined and compared to the couple
limit. For January, half of their combined resources is compared to the single-person
resource limit. (The jointly owned checking account is divided in half, since each
spouse is a Medicaid member.)
2. Mr. and Mrs. Z enter the same room of a nursing facility in January. Mr. Z’s income
is $2,700 per month and Mrs. Z’s income is $300 per month. Their combined
income is $3,000; their combined resources are $2,900.
As of July 1, eligibility for Mr. and Mrs. Z can be determined as separate individuals.
Because this would make Mr. Z ineligible beginning July 1, the worker continues to
determine the Zs’ NF eligibility as a couple.
When a Spouse Moves Into the Same Room
Legal reference: 441 IAC 75 (Rules in Process)
If one spouse is in an institution and the second spouse later moves into the same room
within six months of the first spouse’s entry, the policies under Living in the Same Room
apply to the eligibility of the second spouse. The eligibility and client participation of the
spouse who has been in the institution does not change for the month of entry of the
second spouse.
The initial eligibility of the second spouse to enter the institution is considered with the
spouse already in the institution when they both live in the same room during the six-
month period. In the next month after the second spouse’s entry, combine the income
of both spouses when determining each person’s eligibility, until the six-month period has
expired. The six-month period begins the month of entry of the first spouse.

Title 8: Medicaid Page 17
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Income and Resources of Married Persons
Revised April 14, 2023 When Both Spouses Are in an Institution
Once the six months has elapsed, there is no second six-month period if the couple
enters different rooms and then later reenters the same room. There is not a new six
months’ treatment for a couple’s income and resources if the couple changes nursing
homes. However, if both spouses return home and then reenter a medical facility, a new
six months of treatment as a couple applies.
Mr. Y entered a nursing facility in May and became eligible for Medicaid. Mrs. Y enters
the same room in June. Their eligibility must be considered together from June through
October 31. Her eligibility is determined by adding her income of $450 to Mr. Y’s
income of $575 and comparing the result of $1,025 to twice the 300% income limit. Her
countable resources of $1,180 are added to his countable resources of $1,817. She is
eligible.
Living in Different Rooms
Legal reference: 441 IAC 75 (Rules in Process)
If both spouses are institutionalized in the same facility but in different rooms:
▪ Treat their income and resources as a couple for the month of entry to the institution.
Combined income may not exceed two times the 300% limit for an individual.
▪ Treat their income separately for eligibility purposes effective the month after the month of
entry.
The spouses can be treated as a couple effective the first day of the seventh calendar month of
continuous residency in the same facility if:
▪ One spouse would be ineligible or would receive reduced benefits if considered separately,
or
▪ The spouses choose to be considered together.
If the spouses enter separate rooms at different times, treat income and resources as for an
individual. After the spouse who entered the facility first has been in the facility for six months,
the spouses may choose to be considered together for eligibility.

Title 8: Medicaid Page 18
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Income and Resources of Married Persons
Revised April 14, 2023 When Both Spouses Are in an Institution
Mr. W enters skilled nursing facility care and Mrs. W enters an NF care on November 7 (not
in the same room). Their joint income is $897. They must remain in a medical facility 30
consecutive days for eligibility. They meet this requirement December 6.
Mr. W’s income is $497 monthly and Mrs. W’s income is $400 monthly. Mr. W has $1,800 in a
savings account and Mrs. W has $1,400 in checking.
For November, the combined income of Mr. and Mrs. W is counted towards two times the
300% income limit for an individual. Their income ($897) is below this limit. The couple’s joint
resources ($1,800 + $1,400 = $3,200) are compared to the resource limit for a couple.
Mr. and Mrs. W are both ineligible for the 300% group for November because their combined
resources exceed the couple limit for the 300% group. They are conditionally eligible for
Medically Needy.
For December, each person’s resources are compared to the resource limit for an individual.
Mr. and Mrs. W each have resources below the 300% group limit, so they become eligible
effective December 1.
When Applying for or Receiving Waiver or PACE Services
Legal reference: 441 IAC 83.2(1)“f,” 441 IAC 83.3(5), 441 IAC 83.22(1)“c,” 441 IAC 83.23(5), 441
IAC 83.42(1)“c,” 441 IAC 83.43(5), 441 IAC 83.61(1)“b,” 441 IAC 83.62(5), 441
IAC 83.82(1)“b,” 441 IAC 83.83(4), 441 IAC 83.102(1)“e,” 441 IAC 83.103(4)
hen one spouse is applying for or receiving home- and community-based service (HCBS) waiver or
programs for all-inclusive care for the elderly (PACE) services and the other spouse lives in the home,
treat income and resources according to policies under Income and Resources of Married Persons in
the category “In an institution on or after September 30, 1989, for 30 days or more.”
When both spouses are applying for or receiving HCBS waiver or PACE services, treat income and
resources according to policies under When Both Spouses Are in an Institution: Living in the Same
Room.
When one spouse is in a medical facility and the other spouse is applying for or receiving HCBS waiver
or PACE services, treat each as an individual. Do not count the income and resources of one spouse
to determine the eligibility of the other spouse.
Client Participation
Legal reference: 42 CFR 435.725, 441 IAC 75 (Rules in Process), 441 IAC 81.4(2), 441 IAC 82.9(2)
Medicaid members (except for members in acute hospital care or QMB recipients) are required to
participate in the cost of medical institution care. The amount that a resident contributes is called “client
participation.” Both client participation and third party payments, such as Medicare, must be paid before any
Medicaid payment.
The facility is notified of the member’s client participation amount through the Iowa Medicaid Provider
Access (IMPA) portal.

Title 8: Medicaid Page 19
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Income Available for Client Participation
The facility makes arrangements directly with the resident to collect client participation. Generally, the facility
will ask the member to pay client participation at the beginning of the month from income received during
the month. If income is received periodically during the month, the member may be asked to pay the facility
as income is received.
This section describes:
▪ Countable and exempt income in determining the client participation.
▪ Deductions.
▪ How client participation is calculated.
Enter gross income into the system to determine first-month and ongoing client participation.
Review the client participation determination at the time of the eligibility review. Verify:
▪ The member’s income and deductions.
▪ The income of the community spouse and dependents.
▪ The cost of unmet medical needs.
Income Available for Client Participation
Legal reference: 42 CFR 435.725, 441 IAC 75 (Rules in Process)
Use the member’s total monthly income, including:
▪ The $30 benefit that SSI pays to people who remain eligible in a medical institution.
▪ Infrequent and irregular income disregarded during eligibility computation.
▪ All earned income and child support. (NOTE: The $25 annual fee paid to the Child Support
Recovery Unit is not considered income.)
▪ The gross income before tax or social security withholding. (Members can write the income
source to ask that federal tax not be withheld. Members should describe their living and financial
circumstances in the request.)
▪ Veterans aid and attendance if included in the monthly VA check. Do not allow a deduction for
amounts being recouped. Enter the aid and attendance amount as “income” for benefits if the
system is determining client participation.
▪ Veterans payments for unusual medical expenses (UME) included in the monthly VA check, if the
veteran or the surviving spouse of a veteran is residing in the Iowa Veterans Home (IVH) in
Marshalltown and does not have a spouse or dependents. In these circumstances, the first $90 of
the monthly VA check is not considered to be UME.
Payments for UME are not considered as income in determining eligibility or client participation for
veterans residing in other medical facilities or those residing at the IVH who have a spouse or
other dependents.
▪ Deemed income from the parent for any month when a child spends part of the month in the
parents’ household (i.e., the child enters the facility on a day other than the first of the month).

Title 8: Medicaid Page 20
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Income Available for Client Participation
▪ Benefits from insurance policies for institutional care that are paid to the policyholder but
excluded as income for eligibility purposes. (See 8-E, What Is Not Considered Income and Types of
SSI Related Income: Insurance and Third-Party Payments for a description of this type of income.)
▪ Interest and dividends that are excluded during the eligibility computation.
See 8-E, Projecting Income for instructions on calculating client participation correctly.
Do not allow the earned income deduction of $65 and 1/2 or the $20 disregard in computing gross
income. See Ongoing Personal Needs Allowance regarding earned income.
Ms. J. has a gross monthly pension of $50.00. $5.80 is deducted from the pension for federal income
tax. Also, she has infrequent interest income that prorates to $6.00 monthly. The $50.00 gross
pension and $6.00 interest are counted as income in computing client participation.
If a client enters skilled care, check with the facility to determine if Medicare will share in the cost of
care. Calculate client participation as if Medicare were not paying. The facility will refund any excess
client participation to the client.
EXCEPTION: Client participation is not accessed when the combination of Medicare payments and
Medicaid benefits available to qualified Medicare beneficiaries covers the cost of skilled care. For more
information on client participation in skilled care, see Client Participation for QMBs Entering Skilled
Care.
If there is a community spouse, consider only the institutionalized spouse’s income when determining
client participation.
If both spouses are in the same room and they chose to be considered as a couple, use the couple’s
combined income to determine eligibility. Determine client participation for each spouse based on half
of the combined income.
If spouses are living in different rooms of the same medical institution or in different medical
institutions, they are considered separately for eligibility. Consider each person’s income separately for
client participation.
Benefits insurance policies that are paid to the policyholder are considered available to pay for facility
care. Add them to the client participation for the benefit calculation. These payments are not
considered income for eligibility as long as they are applied to the member’s cost of care. Any
insurance payment retained by the member is considered income in the month of receipt and must be
included in the eligibility determination.
When an insurance payment is based on a flat rate per day, convert the daily amount to a monthly
amount by multiplying by 30.4. Add the monthly amount to the client participation after giving all
allowable deductions. Do not complete form 470-2826, Insurance Questionnaire, when the insurance
payments are added to the client participation. (See 8-E, Third-Party Payments.)
Title 8: Medicaid Page 21
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Income Available for Client Participation
If the client participation plus the additional insurance benefits exceeds the maximum monthly Medicaid
rate, follow policies under If Client Participation Exceeds the Facility’s Medicaid Rate.
Mr. M enters a nursing facility. His income consists of $870 in social security and $200 private
pension. He also has an insurance policy that he purchased to pay for nursing facility care. The policy
pays $70 per day when Mr. M receives nursing facility care. He also has a Medicare supplement
insurance policy with an $86 premium.
The premium on his nursing facility policy is waived while he is receiving care in a nursing facility. He
is applying the benefits paid by this policy to his monthly nursing facility care charges.
Mr. M applies for Medicaid payment for nursing facility care. The worker calculates the average
monthly insurance benefits by taking the $70.00 per day times 30.4, for a monthly average of
$2,128.00 and adds this monthly nursing facility insurance benefit to the client participation after all
deductions are allowed.
Eligibility Calculation
Client Participation Calculation
$ 870.00
+ 200.00
$ 1,070.00
Social security
Private pension
Total income
$ 870.00
+ 200.00
$ 1,070.00
- 50.00
- 86.00
$ 934.00
+ 2,128.00
$ 3,062.00
Social security
Private pension
Total income
Personal needs
Health insurance
Client participation
Insurance benefit
Mr. M’s payment to the facility
Since Mr. M’s payment to the facility is greater than the maximum Medicaid rate for nursing facility
care, no Medicaid payment is made.
Veterans Affairs (VA) lump-sum payments are income in the month of receipt and a resource the
month following the month of receipt, except that portion due to aid and attendance and unusual
medical expenses.
A VA aid and attendance payment is a third-party liability. Count the aid and attendance for the month
it was intended to cover. Recalculate client participation for those months and complete a vendor
adjustment or overpayment, as appropriate.
The portion of a VA payment attributable to unusual medical expenses is not considered as income in
determining eligibility or client participation. See 8-E, Non-MAGI-Related Veterans Affairs Payments for
more information about aid and attendance and unusual medical expenses.
Deem parental income to a child in the month of entry to the facility using SSI income policies. See 8-E,
Deeming from an Ineligible Parent to an Eligible Child.

Title 8: Medicaid Page 22
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Income Exempt From Client Participation
Income Exempt From Client Participation
Legal reference: P.L. 99-643, 441 IAC 75 (Rules in Process)
For FIP recipients, do not calculate client participation using the income of the member or the family if
the member has a parent, stepparent, or child at home who receives FIP and the family’s income is
considered together in determining FIP eligibility.
Sam, age 17, enters a facility and is expected to stay less than 12 months. His Medicaid eligibility is
determined under the 300% group. The family’s income is below the FIP guidelines for their household
size.
Sam will need to meet the 30-day stay requirement for the 300% group. The family at home is
approved for FIP and neither the family’s income nor Sam’s income is used to calculate client
participation.
For State Supplementary Assistance recipients, exempt the State Supplementary Assistance payment
and exempt any client participation that the member paid while in a State Supplementary Assistance
living arrangement for the month of entry to the medical institution.
If the member enters a medical institution from foster care, do not count the amount of income paid
for foster care when calculating client participation for that month. Check with the service worker for
the amount of the member’s income that was spent on the foster care maintenance payment, and use
the remaining balance as income.
Non-MAGI-Related Members
Legal reference: 441 IAC 75 (Rules in Process)
For Non-MAGI-related members who are substantially gainfully employed, as determined by the
Social Security Administration, exempt any SSI and mandatory State Supplementary Assistance
payments for the first two full months after the resident enters the institution.
For Non-MAGI-related members expecting to return home within three months, exempt SSI or
federally administered State Supplementary Assistance payments for the three months after
entry to the institution if the Social Security Administration continues these payments.
To determine whether to exempt the income of an SSI or federally administered SSA recipient,
ask how long the person expects to remain in the facility. Record the answer under
“Comments” on form 470-0641, Report of Change of Circumstances, SSI-Related Programs, and send
the form to the Social Security Administration district office.
If the expected stay is more than three months, assume that SSI and State Supplementary
Assistance will end.
If the expected stay is less than three months, phone the Social Security Administration to
report this. Ask staff to let you know if payments will continue. If payment continues, do not
count it in determining client participation.

Title 8: Medicaid Page 23
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Income Exempt From Client Participation
If the SSI worker does not call you within five days of your telephone call, call the SSI worker
again. Act on the best information available from Social Security.
If you assume that SSI or State Supplementary Assistance payments will continue but later
determine that the member was not eligible for payments, redetermine client participation based
on the actual income for each month.
Ms. H, an SSI recipient, enters a nursing facility on June 10, expecting to stay two months. She
informs her worker June 13. The IM worker sends form 470-0641 to the SS office informing
them of the move and asking the SSI worker to notify the IM worker of the possibility of
continued SSI.
On July 1, the SSI worker notifies the IM worker that the case is being developed. On July 27,
the SSI worker says that the SSI will continue. The IM worker notifies Ms. H that the SSI does
not count for client participation for July, August, or September. Her social security income
and other income are counted.
Veterans or Surviving Spouses of Veterans
Legal reference: 441 IAC 75 (Rules in Process); 38 USC sec. 5503
Veterans Affairs (VA) “reduced/improved” pension payments are limited to $90 per
month after a veteran or surviving spouse enters a medical institution unless the person
has a spouse or dependent. Federal law requires that this $90 be excluded from client
participation (in addition to the $50 personal needs allowance).
The VA considers a report of the changed living arrangement timely if made within 30
days of entry and gives a 60-day notice of benefit reduction. Pension recipients are not
required to repay any excess assistance received between the time they report entry to a
Medicaid institution and the time VA makes the change.
To determine whether to exempt the income of a veteran or surviving spouse of a
veteran, you must:
▪ Determine the type of VA payment being received. Other types of VA benefits, such
as compensation payments, aid and attendance, and unmet medical expenses are not
subject to the reduction and do not qualify for the $90 income exclusion.
▪ Determine whether the person has a spouse or dependents. If the person has a
spouse or dependent, the pension will not be reduced, and the person does not
qualify for the $90 income exclusion.
Based on the person’s situation:
▪ Use the entire VA pension amount to determine eligibility and client participation for
the month of entry if the veteran or surviving spouse is entitled to full benefits for
that month.

Title 8: Medicaid Page 24
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Income Exempt From Client Participation
▪ If the VA pension has already been reduced because the person came from another
institutional placement, exclude $90 pension as income when determining eligibility
and client participation.
▪ If the client does not have a spouse or dependent, assume that the VA pension will
be reduced to $90. Exclude $90 pension income when determining income and client
participation beginning with the month after the month of entry to the institution.
▪ If the VA continues to pay full benefits to a member whose pension will be changed to
$90:
• Consider any pension or aid and attendance amount over $90 for eligibility and
client participation,
• Tell the member to report when the pension is reduced, and
• Use the reduced amount to calculate client participation for the month of the
reduction, even if the change is reported later.
NOTE: VA pension payments of certain residents of the Iowa Veterans Home are not
subject to the $90 limitation but still qualify for the $90 income exclusion. See Residents
of the Iowa Veterans Home.
When an application for a VA pension is approved, a lump sum is sent to the member.
Exclude the portion of this lump sum that represents the $90 reduced/improved pension,
based on federal requirements for eligibility and benefits. Consider any remaining amount
of the lump sum as income in the month of receipt. Any amount of the lump sum retained
in the following month is a countable resource.
Mr. V has a monthly pension of $600 and gross Social Security benefit of $800. He has
no wife or dependent children. He enters a nursing facility from home in January. His full
pension continues until April, when it is reduced to $90. Mr. V informs the worker in
April of the reduction.
Mr. V’s entire VA pension and gross Social Security benefit is used to determine
eligibility and client participation for January, and he is allowed expenses of his home in
the month of entry (up to the current SSI benefit amount) plus the $50 personal needs
allowance.
$90 of Mr. V’s VA pension is excluded for eligibility and client participation effective
February 1, and ongoing. The remaining $510 VA pension plus the $800 Social Security
benefit is countable income until April.
For April, the IM worker removes the $510 from countable income. If the worker is
unable to change April client participation by timely notice, the worker must prepare a
vendor adjustment to correct the payment.

Title 8: Medicaid Page 25
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Income Exempt From Client Participation
Residents of the Iowa Veterans Home
Legal reference P.L. 105-33
A person whose Veteran Affairs (VA) pension would normally be limited to $90 after
entry to a medical institution will continue to receive the full pension amount upon entry
to the Iowa Veterans Home (IVH). However, the person is still entitled to exclude $90 of
the pension in the determination of income and client participation.
To determine whether to exempt the income of a veteran or surviving spouse of a
veteran who resides in the Iowa Veterans Home (IVH), you must determine:
▪ The type of VA payment received and
▪ If the client has a spouse or dependent.
If the client is entitled to a full VA pension for the month of entry to the IVH; then use the
entire VA pension to determine eligibility and client participation in the month of entry.
If the client has a spouse or dependent, continue to count the full VA pension as
income when determining eligibility and client participation. This will result in the client
retaining only the $50 personal needs allowance.
If the client does not have a spouse or dependent, exclude $90 of the VA pension
income beginning the month after the month of entry to the IVH, even though the pension
will not be reduced. This will result in the client retaining $90 of the VA pension in
addition to the $50 personal needs allowance. Because of living at the IVH, the member is
not subject to the normal $90 VA pension limitation.
NOTE: Persons receiving VA compensation payments are not entitled to the $90 veteran’s
income exclusion.
VA payments for unusual medical expenses are countable income when determining client
participation for residents of the IVH who do not have a spouse or dependents.
Deductions From Client Participation
Members are allowed the following deductions from their income when client participation is
calculated:
▪ Personal needs allowances, which are:
• An ongoing personal needs allowance
• Personal needs in the month of entry to the institution
• Personal needs in the month of discharge from the institution
▪ Deduction for the maintenance needs of a spouse and dependents.
▪ Deduction for unmet medical needs.
Each of these deductions is explained in more detail in the next sections.

Title 8: Medicaid Page 26
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Deductions From Client Participation
Ongoing Personal Needs Allowance
Legal reference: 441 IAC 75 (Rules in Process)
All members who have at least $50 in countable monthly income retain $50 for a personal needs
allowance. Members who have less than $50 in countable monthly income retain all of their
income for a personal needs allowance.
The personal needs allowance is for the member’s use for items not provided by the facility,
such as magazines, cigarettes, personal care items, etc. If not used, the personal needs allowance
represents a countable resource in the month following the month the income was received and
is subject to resource limits.
Veteran and surviving spouses of veterans who receive the $90 reduced/improved pension
receive a $50 personal needs allowance in addition to the $90 income exclusion. See Veterans
or Surviving Spouses of Veterans.
State-Funded Payment
When a member who resides in a nursing facility, ICF/ID, or NF/MI has countable income
of less than $50 per month, a state-funded payment for the difference between that
countable income and $50 is issued so that the member will have $50 for personal needs.
(This state-funded payment is not available to residents of PMICs.)
When a facility application is approved with an effective date in the previous month, issue
the appropriate state-funded payment for each month in a lump-sum payment.
Do not consider the lump sum as income in the month of receipt for purposes of
determining eligibility or client participation. The state-funded payment is excluded as
assistance based on need.
Direct Deposit for State-Funded Payment
Medicaid facility residents or their payees who receive a state-funded payment have the
option to request that their payments be deposited directly to an active account at a
financial institution.
The date the money is deposited into the account depends on when the payment is
authorized, as follows:
▪ Ongoing monthly payments are deposited into the member’s account on the first
working day of the month.
▪ Reinstatements that occur too late in the month to be included with the monthly
issuances are generally deposited into the member’s account three to five days after
the first working day of the month.

Title 8: Medicaid Page 27
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Deductions From Client Participation
Members who choose direct deposit will receive a notification similar to a check stub.
This notification is mailed so that the member should receive it close to the date the
benefits are available in the account.
Remind members that there is a risk that creditors holding past-due bills could attempt to
garnish the account.
When a member requests direct deposit, have the member complete form 470-0261,
Agreement for Automatic Deposit. See 6-Appendix for the form and instructions for its use.
Use the Automated Direct Deposit (DIRD) system to enroll members in direct deposit.
See 14-B(4), DIRD-Automated Direct Deposit for instructions in using the DIRD system. The
beginning date for direct deposit is ten working days past the date you enter the direct
deposit request in the DIRD, unless another, later beginning date is requested.
Benefits will continue to be credited to the account until the member requests a change
and you make direct deposit stop entries in the DIRD system. Act promptly to terminate
or change direct deposit when requested to do so by the member.
Remind members to report promptly if the account is closed or changed. Failure to report
a closed or changed account can cause delays in getting the payment if the direct deposit is
rejected.
If facility assistance is canceled and reinstated before system month end of the month of
cancellation, direct deposit will continue. If the facility program is still canceled after
system month end, DIRD system entries are required to start direct deposit again.
Earned Income
If the member has earned income, allow an additional $65 deduction from earned income only.
The $65 deduction is intended for expenses in producing the income, like transportation, extra
clothing, FICA, etc. This deduction is in addition to the $50 deduction for personal needs and
the $90 VA pension income exemption for certain veterans and surviving spouses.
If the member has less than $65 of earned income, deduct only the earned amount. If the
member has self-employment income, deduct the expenses of self-employment from gross self-
employment income. The $65 personal needs allowance is automatically subtracted from the
amount of earned income entered in the ABC system’s BCW2 field.
See 8-E, Projecting Income more information.
1. Mr. B, a Medicaid member residing in an ICF/ID, has income of $596. His client
participation is $546 monthly ($596 - $50 personal needs).
2. Mrs. D, a Medicaid member residing in a nursing facility, has income of $596. Her client
participation is $546 monthly ($596 - $50 personal needs).

Title 8: Medicaid Page 28
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Deductions From Client Participation
3. Mrs. G, a Medicaid member residing in a nursing facility, has income of $30 SSI. Her client
participation is $0 and a state-funded payment of $20 is issued to bring her total personal
needs allowance up to $50.
4. Ms. M lives in a nursing facility and occasionally works for her former employer when
needed. She has $450 a month unearned income and her earned income averages $50 a
month. She is allowed a total personal needs deduction of up to $65 from earned income
and $50 from unearned income.
5. Mr. H, an SSI recipient living in an ICF/ID, has net self-employment earnings of $18 a
month from his hobby, carving wood. He is allowed a total of $48 personal needs
allowance, $18 from his earned income and $30 from the SSI income. His client
participation is $0. A state-funded payment of $20 is issued to bring his total personal
needs allowance to $68.
Personal Needs Expenses in the Month of Entry
Legal reference: 42 CFR 435.725, 42 CFR 435.726, 441 IAC 75 (Rules in Process)
A person entering a medical institution can be given an allowance for stated living expenses
during the month of entry unless the person has a community spouse. Allow this deduction in
addition to the $50 personal needs allowance.
For a single person, the limit on the deduction for living expenses or the month of entry is the
amount of the SSI benefit for one person. Use the following deduction guidelines for married
couples:
▪ If both spouses enter a medical institution in the same month and live in the same room,
combine their income in determining client participation for the month of entry. Deduct any
claimed expenses from this amount up to the amount of the SSI benefit for a couple.
▪ If both spouses enter a medical institution in the same month but live in different rooms,
deduct any claimed expenses up to one-half of the amount of the SSI benefit for a married
couple. However, if the income of one spouse is less than the deduction, give the remainder
of the allowance to the other spouse.
▪ If the community spouse enters a medical institution in a later month, deduct claimed
expenses for the month of entry when calculating client participation, up to the amount of
the SSI benefit for one person.
Determine the prior living arrangement of the member. People living in a private living
arrangement do not have to verify their living expenses unless questionable. Living alone or with
friends or relatives is a “private living arrangement,” regardless of who owns the dwelling.
If the person was not in a private living arrangement, allow these deductions for personal needs
expenses in the month of entry as follows:
▪ If the member enters a hospital and then enters a nursing facility in the next month, do not
allow a personal needs expense deduction for the month of entry into the nursing facility.
The month of entry to a medical institution was the month that the person entered the
hospital, and client participation is not assessed for people in hospitals.

Title 8: Medicaid Page 29
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Deductions From Client Participation
▪ If a waiver member or programs for all-inclusive care for the elderly (PACE) enrollee moves
to a nursing facility, do not recalculate client participation. Apply any client participation that
was not used for waiver services or PACE to the first partial month of facility care.
▪ If the member was in a residential care facility (RCF) and received State Supplementary
Assistance, deduct the amount paid in client participation to the RCF. Follow these same
guidelines for members of in-home health-related care.
▪ If the member was in a RCF but did not receive State Supplementary Assistance, allow a
deduction for home-maintenance living expense up to the amount of the SSI benefit for a
single person.
▪ If the member was in a family-life home, deduct the amount paid to the home for client
participation.
▪ If the member was in foster care, deduct the amount of the income retained by the
Department to recover foster care expenses.
In April, Mr. L enters skilled care and Mrs. L enters nursing care. Their gross monthly
income is $272 for Mrs. L and $430 for Mr. L. They state that they have home
maintenance expenses of $1,500 and are allowed a deduction equal to a couple’s SSI
benefit of $1,415 for the month of entry.
The Ls’ combined gross income is $702. Each spouse is allowed a $50 personal needs
allowance. The personal allowances and the deduction for living expenses for the month of
entry are subtracted from that gross income. ($702 – 50 – 50 – 1,415 = 0)
Personal Needs in the Month of Discharge
Legal reference: 441 IAC 75 (Rules in Process)
The member is allowed an additional personal needs deduction in the month of discharge from a
medical institution to a private living arrangement, unless the member has a community spouse.
A member does not need to make any declaration of expenses to get this deduction. Deduct the
SSI benefit for a single person (or the SSI benefit amount for a couple if both spouses are
discharged in the same month).
If member moves from a nursing facility to a HCBS waiver program or programs for all-inclusive
care for the elderly (PACE), recalculate the nursing facility client participation. Allow a home
maintenance deduction for the month of discharge, even if the member is going to receive
waiver or PACE services during the month.
If the member is discharged and returns home and the spouse at home is an HCBS waiver
member or PACE enrollee, allow a diversion to the waiver or PACE spouse at home. (See
Allowance for the Community Spouse.)
Allow the deduction even if you are informed about the discharge after the member left the
facility or after client participation has been paid. Complete a vendor adjustment for the month
of discharge if necessary.

Title 8: Medicaid Page 30
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Deductions From Client Participation
1. Ms. M enters skilled care in February and returns home in October. She is allowed a
deduction for expenses in October equal to the SSI benefit for one person.
2. Mr. and Mrs. P enter a nursing facility together and return home in the same month. They
are given the SSI benefit for two as a deduction in the month of discharge.
Deduction for the Maintenance Needs of Spouse and Dependents
Legal reference: 42 CFR 435.725, 441 IAC 75 (Rules in Process)
Allow a deduction for the maintenance needs for:
▪ A community spouse and dependents living with the community spouse, including:
• Children, regardless of age,
• Parents and in-laws, and
• Siblings of either spouse.
NOTE: Consider children under age 22 who are away attending school but are under the
control of the parents as living with the community spouse.
▪ Children under the age of 21 living at home when there is no community spouse.
If the institutionalized spouse has a community spouse with income less than the minimum
monthly maintenance needs allowance (MMMNA), allow a deduction to provide an ongoing
allowance for the maintenance needs of the community spouse. Also allow a deduction for
minor or dependent children, stepchildren, dependent parents, or the dependent siblings of
either spouse who live with the community spouse.
The community spouse and dependents must apply for every income benefit for which they are
eligible, except they are not required to accept Supplemental Security Income (SSI), Family
Investment Program (FIP), or State Supplementary Assistance (SSA) in place of the maintenance
needs allowance.
Issue form 470-0383, Notice Regarding Acceptance of Other Benefits, to the community spouse and
dependents. The community spouse and dependents must indicate whether the member or
spouse intends to apply for the identified benefits.
If the community spouse or dependents refuse to apply for benefits, contact the benefit agency
to determine benefit amounts for a person in the same financial circumstances as the spouse or
dependent. Count the anticipated amount as income as if the spouse or dependents received the
benefits. Reduce the maintenance needs allowance by the amount of the anticipated income
from each income source.
Consider income prospectively. See 8-E, Projecting Future Income. If there is a change in income,
consider the change when determining prospective income.

Title 8: Medicaid Page 31
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Deductions From Client Participation
Use the verified gross income of the spouse and dependents when determining maintenance
needs. Include all monthly earned and unearned income and assistance from the FIP, SSI, and
SSA. Gross income also includes the proceeds of any annuity or contract for sale of real
property. See 8-D, Specific Non-MAGI-Related Resources: Annuities on how to count annuities.
Consider income the same way the SSI program considers income. Do not allow the community
spouse or dependents the earned income disregard or the general income disregard. Do not
count any other income disregarded by policy.
If the community spouse is receiving FIP, the community spouse’s share of the grant is based on
whether the children for whom the FIP benefit is received are the children or the stepchildren of
the institutionalized spouse.
▪ If the children receiving FIP are all stepchildren of the institutionalized spouse, use the
standard of need for one as the portion of the FIP benefit to count as income for the
community spouse.
▪ If the children receiving FIP are all children of the institutionalized spouse, consider the FIP
grant as income to the community spouse. Divide the grant by the number of people in the
household and count the result as income to each person when calculating deficits.
▪ If the institutionalized spouse has both stepchildren and legal children at home receiving FIP,
use the procedure in 4-E, Excluded Parent to determine the FIP income of the community
spouse.
If the community spouse or dependents receive SSI or federally administered SSA, use the State
Data Exchange (SDX) amount labeled “SSI gross” or “SSA gross.”
If the community spouse or dependents receive SSA benefits for in-home health-related care,
count all the SSA benefit for the spouse or dependent receiving this care. If both spouses receive
in-home health-related care in the month of entry, ask the service worker the amount of the
community spouse’s SSA benefit.
Allowance for the Community Spouse
Legal reference: 441 IAC 75 (Rules in Process)
To determine the maintenance needs of the community spouse, subtract the spouse’s
gross income from the minimum monthly maintenance needs (MMMNA) allowance shown
below. The allowance is indexed annually for inflation.

Title 8: Medicaid Page 32
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Deductions From Client Participation
Minimum Monthly Maintenance Needs Allowance (MMMNA)
Calendar Year
Amount
Calendar Year
Amount
2024
$3,853.50
2012
$2,841.00
2023
$3,715.50
2011
$2,739.00
2022
$3,435.00
2010
$2,739.00
2021
$3,259.50
2009
$2,739.00
2020
$3,216.00
2008
$2,610.00
2019
$3,160.50
2007
$2,541.00
2018
$3,090.00
2006
$2,488.50
2017
$3,022.50
2005
$2,377.50
2016
$2,980.50
2004
$2,319.00
2015
$2,980.50
2003
$2,266.50
2014
$2,931.00
2002
$2,232.00
2013
$2,898.00
2001
$2,175.00
Mr. B enters a nursing facility for long-term care, leaving Mrs. B at home. Mr. B has
$800 per month gross income and also receives $100 in aid and attendance
payments. The income available from Mr. B to meet Mrs. B’s needs is determined as
follows:
$ 800.00
- 50.00
$ 750.00
Gross income
Personal needs allowance
Available to meet Mrs. B’s needs
If the shortfall between Mrs. B’s income and the MMMNA is $750 or more, Mr. B’s
client participation will be $100, the amount of his aid and attendance payments.
When one spouse lives in a facility and the other lives in the community and receives
HCBS waiver or programs for all-inclusive care for the elderly (PACE) services, the
spouses are treated as a married couple living in separate facilities for eligibility.
However, when determining client participation of the institutionalized spouse, a diversion
to the community spouse can continue even when the community spouse is receiving
waiver or PACE services.
If you divert income from the institutionalized spouse to the community spouse, inform
the community spouse’s income maintenance and SSI workers when the community
spouse or dependents receive FIP, SSI, or SSA.
Either spouse may request an appeal if the spouse believes the community spouse needs
income above this level because of significant financial duress. (If the income of the
institutionalized spouse does not support a greater allowance for the community spouse,
explain this to the client.)

Title 8: Medicaid Page 33
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Deductions From Client Participation
The administrative law judge may substitute a higher allowance. If the appeal decision
establishes a higher allowance, substitute this amount as the maintenance need. See 8-D, If
the Applicant Appeals the Attribution Amount.
If any court orders a greater monthly income allowance against the institutionalized
spouse to support the community spouse, use that amount as the minimum monthly
maintenance needs allowance. Obtain from the applicant a copy of the court order to
verify the amount of the court-ordered support.
If the community spouse indicates in writing that some or all of the diversion is not
wanted, make the diversions in the lesser amount requested by the community spouse.
Assume that the community spouse is receiving the benefit of the income diverted from
the institutionalized spouse. No further investigation is required unless there is evidence
to the contrary. When the income is not made available, make a referral to the adult
protective service worker at the request of the community spouse.
1. Mr. B is eligible for Medicaid payment in a nursing facility. His gross income is
$650 a month, and Mrs. B’s income is $350 a month. The only income that can
be provided for a maintenance need for Mrs. B is $650 minus $50 personal
needs, or $600 a month.
This diversion allows a total income of only $950 a month for Mrs. B ($350 +
$600). No more income can be diverted to Mrs. B, even if an appeal decision
sets her maintenance needs at a higher amount.
2. Mrs. G is receiving skilled care and is eligible for Medicaid in the 300% group.
Mr. G is at home. He has earned income of $4,750 per month. No diversion of
Mrs. G’s income can be made for Mr. G in determining her client participation,
because his income exceeds the maintenance need of $3,853.50, and no greater
amount has been ordered.
3. Mr. D receives skilled care and is eligible for Medicaid under the 300% group.
Mrs. D is living in an RCF and receives SSI and SSA. Mrs. D’s income consists of
$533 social security, $430 SSI, and $276.30 SSA, for a total of $1,239.30 per
month. Mr. D has gross income of $752. He is allowed a $50 personal needs
allowance. The diversion is determined as follows:
Mr. D:
$ 752.00
- 50.00
$ 702.00
Gross income
Personal needs
To divert
Mrs. D:
$ 3,853.50
- 1,239.30
$ 2,614.20
Maintenance
Income
Deficit
Only $702 can be diverted to Mrs. D, because Mr. D must be allowed an
ongoing personal needs allowance before a diversion is made to Mrs. D. Mrs.
D’s income with the diversion is $1,239.30 + $702.00 = $1,941.30. Mrs. D loses
eligibility for State Supplementary Assistance.

Title 8: Medicaid Page 34
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Deductions From Client Participation
4. Mr. O is in a nursing facility and eligible for Medicaid. Mrs. O and their three
children are at home and receiving FIP. Mr. O has begun receiving veterans’
income of $500 per month. Mrs. O’s only income is the FIP grant.
The amount of FIP to count for Mrs. O in the first month of diversion is the
difference between the grant for four people and the grant for three people
($495 - $426 = $69). The diversion to Mrs. O is determined as follows:
Mr. O:
$ 500.00
- 50.00
$ 450.00
Income
Personal needs
To divert
Mrs. O:
$ 3,853.50
- 69.00
$ 3,784.50
Maintenance
FIP income
Deficit
Mr. O can divert a maximum of $450 of his income to Mrs. O. With this
diversion, Mrs. O and the children remain eligible for FIP.
Even though Mrs. O’s income may decrease after the initial month, there will be
no change in the diversion from Mr. O. He does not have enough income to
meet the needs of his spouse.
5. Mrs. E is a community spouse with $500 gross monthly income. She is
estranged from Mr. E and has obtained a court order for $3,900 per month in
support. The court-ordered amount is substituted for the $3,853.50
maintenance needs. The diversion of income is determined as follows:
Mr. E:
$ 1,100.00
- 50.00
$ 1,050.00
Gross income
Personal needs
To divert
Mrs. E:
$ 3,900.00
- 500.00
$ 3,400.00
Maintenance
Income
Deficit
Mr. E can divert only $1,050 because his income supports only this amount.
Allowance for Other Dependents
Legal reference: 441 IAC 75 (Rules in Process)
Determine the maintenance needs of the other dependents by subtracting each person’s
gross income from 150% of the monthly federal poverty level for a family of two
(currently $2,178 per month), and dividing the result by three. Include SSI and FIP benefits
as income.
The dependent’s diversion does not need to be for the benefit of the dependent. That is a
requirement for the community spouse diversion only.

Title 8: Medicaid Page 35
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Deductions From Client Participation
1. Mr. T receives Medicaid payment for nursing care. His wife and mother live at
home. Diversion for Mr. T’s dependents is determined as follows:
Mr. T:
$2,150.00
- 50.00
$ 2,100.00
Gross income
Personal needs
Available to divert
Mrs. T:
$ 3,853.50
- 970.00
$ 2,883.50
Maintenance needs
Income
Deficit
Mr. T’s mother:
$2,178.00
- 398.00
$1,780.00
150% FPL for 2
Income
Divided by 3 = $593.34 maintenance for dependent
The total need of the spouse and dependent is $2,883.50 + $593.34 or
$3,476.84. Mr. T does not have enough income to meet all of his mother’s
needs. Mr. T’s client participation is determined as follows:
$ 2,150.00
- 50.00
- 2,883.50
- 0.00
$ 0.00
Gross income
Personal needs allowance
Diversion for spousal deficit
Diversion for mother’s needs ($2,100.00 - $2,883.50)
2. Mrs. W lives in a nursing facility and is Medicaid-eligible. Mr. W lives at home
with two children who do not receive FIP. Mr. W has earned income. Mrs. W
has workers’ compensation. The children have no income.
Mrs. W:
$ 700.00
- 50.00
$ 650.00
Gross income
Personal needs allowance
Income available to divert to spouse and dependents
The spousal and dependent allowances are determined as follows:
Mr. W:
$ 3,853.50
- 4,000.00
$ 0.00
Maintenance
Gross income
Unmet needs
Children:
$2,178.00
- 0.00
$2,178.00
Poverty level
Income
Divided by 3 = $726.00 per
child
$726.00 x 2 children = $1,452.00
All of Mrs. W’s income after deduction of her personal needs is diverted for the
children. Mrs. W’s client participation is determined as follows:
$ 700.00
- 50.00
- 650.00
$ .00
Gross income
Personal needs
Diversion for dependents’ needs ($700 – 50 = $650)
Amount of client participation

Title 8: Medicaid Page 36
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Deductions From Client Participation
3. Mr. P is in a nursing facility and is eligible for Medicaid. Mrs. P lives at home with
her three children (Mr. P’s stepchildren) who are eligible for FIP.
The FIP grant for the children and Mrs. P is $495. The amount for the children
is $426. The amount for Mrs. P is $69 ($495 - $426 = $69). Each child is
credited with $142 as income ($426 divided by 3). The maintenance allowances
are determined as follows:
Mr. P:
$ 821.00
- 50.00
$ 771.00
Gross income
Personal needs
Available to divert
Mrs. P:
$ 3,853.50
- 69.00
3,784.50
Maintenance
FIP income
Deficit
All of Mr. P’s income is diverted to Mrs. P. There is no more income remaining
for a diversion to the dependents.
If the institutionalized person does not have a spouse but does have children under age 21
at home, allow a deduction from the institutionalized person’s income to meet the
children’s maintenance needs. Do not allow a deduction if the children receive FIP.
Count the children’s income and a parent’s income if living in the home in determining
maintenance needs. Use gross income less disregards allowed in the FIP program. Child
support is considered income of the child.
Calculate the children’s maintenance needs by subtracting the children’s income from the
FIP standard for that number of children.
1. Mr. G is eligible for Medicaid while living in a nursing facility. He has $700 per
month gross income. He has a child aged 20 at home who has no income. The
FIP payment standard for one is considered as the need. The determination of
the dependent’s allowance is as follows:
Mr. G:
$ 700.00
- 50.00
$ 650.00
Gross income
Personal needs
Available to divert
Child G:
$ 183.00
- 0.00
183.00
Need for one
Income
Deficit
2. Mrs. F is Medicaid-eligible in a nursing facility. She has $350 gross monthly
income. She has two children at home who are under 21. One child has
unearned income of $105 per month. The determination of the dependents’
allowance is as follows:
Mrs. F:
Both children:
$ 350.00
- 50.00
$ 300.00
Gross income
Personal needs
Available to divert
$ 361.00
- 105.00
$ 256.00
Payment standard
Unearned income
Deficit
$256 can be diverted to meet the needs of the children.

Title 8: Medicaid Page 37
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Deductions From Client Participation
Deduction for Unmet Medical Needs
Legal reference: 42 CFR 435.725, 441 IAC 75 (Rules in Process)
Allow a deduction for expenses a person incurs for medical or remedial care that is not payable
by a third party, including the following:
▪ The member’s Medicare premiums, other health insurance premiums (including dental and
vision), deductibles, and coinsurance.
• There should be no Medicare Part A or Part B deductibles or coinsurance once
Medicaid eligibility is established. The portion of the premium that remains the
member’s responsibility is an allowable unmet medical deduction.
• Members who are enrolled in Part D plans or who qualify for Part D but were not
enrolled may continue to be responsible for premiums, deductibles, drug costs, or
coinsurance. The length of time the member remains responsible and the amount of
expense varies greatly between plans.
Allow verified expenses as an unmet medical deduction. If a deduction is allowed and
expenses are later reimbursed, consider the reimbursement as income in the month of
receipt and adjust the client participation accordingly.
▪ Health insurance premiums for coverage of other persons of the family when the insurance
is a family policy that covers the member.
▪ Expenses for necessary medical or remedial care recognized under state law that are not
covered by Medicaid and were not incurred during a transfer of assets penalty period.
▪ Medical bills for the month of eligibility that the member paid before being determined
eligible, unless Medicaid will later pay the bill. For example, a member may have paid a
medical bill incurred before eligibility was determined.
If those bills were incurred during the period that retroactive eligibility is granted or during
the month of application, allow the bills to be deducted as long as Medicaid does not later
pay the bill.
▪ Client participation paid in another medical facility and “private pay” payments made by
residents of medical institutions.
▪ Client participation paid for in-home health-related care, home- and community-based
waiver services, or programs for all-inclusive care for the elderly (PACE).
1. Mr. S was approved for Medicaid and nursing facility payments effective May 1. He was
ineligible for Medicaid before the month of May. Mr. S did not have enough resources to
pay all the private-pay charges for the month of April. He still owes the facility $900 for
April charges.
Mr. S arranges with the facility to pay off the $900 by paying $300 in June, $300 in July, and
$300 in August. He provides the IM worker with verification of this agreement. An unmet
medical deduction of $300 can be allowed for the months of June, July, and August when
calculating the client participation for those months.

Title 8: Medicaid Page 38
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Deductions From Client Participation
2. Mrs. A is approved for Medicaid and nursing facility payments effective May 1. She has
client participation of $200 but she fails to pay the May client participation during the
month of May. In June, Mrs. A pays both the May and the June client participation.
The IM worker cannot allow an unmet medical deduction in the month of June for the
$200 May client participation that was paid late, as it is not a private-pay expense.
Do not allow a deduction for payment of:
▪ A bank service charge made for handling medical insurance payments.
▪ Insurance premiums if the benefit paid is counted as income for eligibility.
▪ Adult day care services from a source not certified as a Medicaid provider. This is not
medical care.
If the agent is unable to tell you if the insurance is indemnity or health, ask if an established
amount is paid if the member is ill or injured, regardless of the amount of the medical bill. If yes,
treat it as an indemnity policy. If benefits are paid only to cover incurred expenses of illness or
injury, treat it as a health insurance policy.
If Client Participation Exceeds the Facility’s Medicaid Rate
Legal reference: 441 IAC 81.22(1)
The member is required to pay only the amount charged to the Medicaid program. (When the
Department retroactively increases the maximum daily rate, the facility can charge the client the
increased amount retroactively.)
After computing client participation, if client participation exceeds the facility’s Medicaid rate on
IoWANS, the ABC system will generate a notice telling the member that the facility can’t charge client
participation in excess of the approved Medicaid daily rate for the number of days the member
received services in the facility. If eligibility and client participation were calculated manually, add the
following words to the notice:
“This is the most you will have to pay for your care, based on your income. The facility can
charge you this amount or their daily rate whichever is less, for the days you are in the facility. If
the facility rate changes for the past months, you may have to pay more based on the new rate.”
When the client participation equals or exceeds the maximum Medicaid monthly reimbursement rate,
no Medicaid payment is made. The member retains any difference between the Medicaid rate charged
by the facility and the client participation.
This situation occurs most often when the member has veterans’ aid and attendance payments but can
also occur when the member has nursing facility insurance.

Title 8: Medicaid Page 39
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 If Client Participation Exceeds the Facility’s Medicaid Rate
Mr. C is in a nursing facility. He does not have a wife or dependents. He receives:
$ 900.00
$ 400.00
$ 500.00
$ 1,000.00
Social security
Private pension
VA pension
VA aid and attendance allowance (disregarded for eligibility)
His income exclusive of the A & A allowance is $1,800, and he is eligible for Medicaid. The total
amount available to him is $2,800. Mr. C has no unmet medical expenses or private health insurance,
so his potential client participation is $2,660 ($2,800 - $50 personal needs allowance - $90 VA
pension exemption).
Mr. C’s client participation exceeds the maximum Medicaid reimbursement rate for the facility where
he lives. Since his client participation exceeds the Department’s maximum payment for nursing care,
Medicaid makes no payment for Mr. C’s care, although he is eligible for all other Medicaid services.
Client Participation for Skilled Care
Legal reference: 441 IAC 81.6(20)“b”
Do not split or zero out client participation just because Medicare covered some of the skilled stay at
the facility. The facility provider will report Medicare-covered days on the Case Activity Report. In most
cases, the Medicare payment amount will exceed or equal the Medicaid-allowed payment amount.
If this is the case for the skilled days, Medicare will pay the cost of care. Medicaid will not participate,
and the facility will not require the member to pay client participation. Payment of any skilled care days
will be handled by the facility in the way it submits the claim. Facility providers have received an
informational letter explaining the procedure for these claims.
Providers are to submit a Medicare claim for the Medicare-covered days. The provider should also
submit one Medicaid care claim for the full month, even when the resident’s status changes to a
Medicare-payable level of care during the month. The Medicare days are to be shown on the Medicaid
claim as noncovered days to avoid duplicate payment by Medicare and Medicaid.
A Medicaid member was in a nursing facility from May 1 to May 7. She was in the hospital on May 7
through May 12 and then returned to the nursing facility with Medicare coverage from May 13
through May 16. Medicare coverage ended May 17. The member’s care was covered only by Medicaid
from May 17 to May 31.
The worker determines one client participation amount for the entire month. The facility bills
Medicare for the four Medicare-covered days of May 13 to May 16. The facility submits a Medicaid
claim for May 1 through May 31 (the entire month) showing four noncovered days (the four days that
Medicare covered).
The claim for May 1 through May 31 is processed and the facility receives Medicaid payment for 27 of
the 31 days. The Medicaid payment is reduced by the amount of the full monthly client participation.
The four Medicare-covered days are not paid on this claim. If Medicare does not pay at 100%, a
crossover claim is received and processed. Medicaid payment is made only when the rate for
Medicare didn’t equal or exceed the Medicaid rate.

Title 8: Medicaid Page 40
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Client Participation for Skilled Care
When the Medicare rate equals or exceeds the Medicaid rate, no Medicaid payment is made to the
facility for the Medicare-covered days. Most of these situations, there is no Medicaid payment on the
Medicare crossover claim. In a rare case where the Medicaid rate is higher, you will need to adjust the
client participation.
If a facility reports that the client participation has been used twice, once on the crossover claim and
once on the long-term care claim, then the stay will need to be split in IoWANS to correct the
doubled client participation.
If the facility reports that the client participation has been used twice and the client is a qualified
Medicare beneficiary (QMB), then the stay will need to be split in IoWANS to show that client
participation was zero for the Medicare-covered days. Change the client participation to zero during
Medicare-covered days when:
▪ A QMB-eligible facility client is receiving skilled care, and
▪ The Medicaid rate is higher than the Medicare rate for this stay.
For more information on QMB eligibles, see Client Participation for QMBs Entering Skilled Care.
Members With a Medical Assistance Income Trust (MAIT)
Legal reference: 441 IAC 75.24(249A)
People with income in excess of 300 percent of the SSI benefit for one person may qualify for Medicaid
payment for institutional care using a medical assistance income trust. A person with such a trust
qualifies for facility payment only if the person’s total gross monthly income does not exceed 125
percent of the statewide average charge for the type of facility or level of care the person meets.
If the person’s total income is less than 125 percent of the statewide average charge for care, the trust
makes payments to raise the person’s countable income up to but not above the 300% limit. This
allows the person to be income-eligible for Medicaid payment for facility care. See 125 Percent of the
Statewide Average Charge for Care.
Unless the trust document provides otherwise, the trust is effective as of the date the trust document
is executed (signed) and the trust is funded. If the trust document is signed but not funded, the trust
becomes effective the first month that income is assigned to the trust.
For example, if the trust document is signed after the first of the month, and the income for the month
is assigned to that trust, then only income that the trustee makes available to the member is counted
for eligibility during that month.
See 8-D, Trusts for more information about requirements for medical assistance income trusts. Iowa
law requires certain deductions be allowed from the trust beneficiary’s gross income when determining
client participation.

Title 8: Medicaid Page 41
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Members With a Medical Assistance Income Trust (MAIT)
The following sections explain:
▪ 125 Percent of the statewide average charges for care
▪ Trust payments
▪ Determination of client participation
125 Percent of the Statewide Average Charge for Care
Legal reference: 441 IAC 75.24(3)“b”
Charge for care figures are:
Type of Care
Charge for Care
July 1, 2022
June 30, 2023
July 1, 2023 –
June 30, 2024
Nursing facility
9507.50
$10,467.50
PMIC
21,701.25
$21,477.50
Mental health institute
$30,857.50
$35,152.50
ICF/ID
$46,272.50
$54,781.25
Substitute a higher amount for 125 percent of the average statewide charge for nursing facility
care in the following situations:
If the trust beneficiary meets the level of
care requirements for…
Then use this amount in the income
comparison:
Nursing facility care and receives some type of
specialized care (e.g., care in a Medicare-certified
hospital-based nursing facility or a nursing facility
providing care to special populations such as an
Alzheimer’s unit, pediatric skilled care, or skilled
care for brain injury)
The cost of the type of specialized care
being received. In general, use the rate
charged by the facility.
Skilled nursing care and is eligible for HCBS
waiver or programs for all-inclusive care for the
elderly (PACE) services except for income
The costs in a facility providing the type of
care being received
Services in a PMIC and resides in a PMIC
The 125 percent of the statewide average
charge to private-pay patients for PMIC
care
Services in an MHI and resides in a state MHI
The 125 percent of the statewide average
charge for state MHI care
Services in an MHI and is eligible for HCBS
waiver or PACE services except for income
The 125 percent of the statewide average
charge for state MHI care
Services in an ICF/ID and resides in an ICF/ID
The 125 percent of the maximum monthly
Medicaid payment rate for services in an
ICF/ID

Title 8: Medicaid Page 42
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Members With a Medical Assistance Income Trust (MAIT)
Trust Payments
Legal reference: Iowa Code Section 633C.3
If the total income received by the beneficiary of a medical assistance income trust, including
income received or generated by the trust, is less than 125 percent of the applicable statewide
average charge for care, Iowa law allows the following deductions (trust payments) from gross
income to determine client participation:
1. A reasonable amount may be paid or set aside for trust administration fee not to exceed
$10 per month without court approval. This payment is not considered income to the client.
2. An amount for the needs of the beneficiary:
▪ A personal needs allowance of $50 for a medical facility resident plus additional amounts
for personal needs in the month of entry or discharge, as appropriate. NOTE: Exclude
$90 of VA pension income per Income Exempt From Client Participation.
▪ A maintenance allowance of 300% of the current SSI income limit for a waiver member
or a PACE enrollee.
3. An amount for the needs of dependents:
▪ An amount diverted to the community spouse to raise the spouse’s income to the
minimum monthly maintenance needs allowance.
▪ A deduction for minor or dependent children, dependent parents, or the dependent
siblings of either spouse living at home.
Determine the deduction according to Deduction for the Maintenance Needs of Spouse and
Dependents.
4. An amount for unmet medical needs, determined according to Deduction for Unmet
Medical Needs.
5. Any amount of income remaining, up to the Medicaid rate, is paid directly to the medical
facility, a waiver service provider, or the PACE provider. This payment is not considered
income to the client.
6. At the trustee’s option, payment may be paid directly to other medical providers that would
otherwise be covered by Medicaid or may be paid to reimburse Medicaid. This payment is
not considered income to the client.
Title 8: Medicaid Page 43
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Members With a Medical Assistance Income Trust (MAIT)
7. Any remaining income must be retained in the trust until the beneficiary’s death, or, if the
trust is abolished, must be paid to the state of Iowa.
1. Mrs. S is in a nursing facility at nursing facility level of care. She has social security benefits
of $974 and a pension of $780, for total gross monthly income of $1,754. Mrs. S did not
really need a medical assistance income trust but is paying all of her income to the trust.
Mrs. S’s total income is less than 125 percent of the average charge for nursing facility
level of care. The trust will pay her all of the available income. Count the payment from
the trust to Mrs. S as income. She is income-eligible for Medicaid payment of nursing
facility care using the medical assistance income trust.
2. Mr. T is in a nursing facility at the nursing facility level of care. He has social security
benefits of $1,500 and a monthly pension of $1,138 per month. Only his social security
check is deposited into his medical assistance income trust.
Mr. T’s total income is less than 125 percent of the average charge for nursing facility
care. The trust may set aside $10 per month for administration. The trust will pay Mr. T
the $50 personal needs allowance each month Mr. T is income-eligible for Medicaid
payment of nursing facility care using the medical assistance income trust.
3. Mr. W is in the Alzheimer’s unit of a nursing facility. He meets the nursing facility level of
care. He has social security benefits of $2,825, an annuity payment of $3,450, and a
monthly private pension of $3,400.
Mr. W’s total income is $9,675. His total income is higher than $9,507.50, 125 percent of
the average charge for nursing facility care. However, since Mr. W is receiving specialized
care, the cost of his Alzheimer’s care can be substituted for the average nursing facility
charge.
Mr. W provides a statement from the nursing facility that he pays $360 per day for his
care. The average monthly cost would be $10,944 ($360 X 30.4 = $10,944). The cost of
$10,944 can be substituted in place of 125 percent of the statewide average charge for
nursing facility care. Mr. W is income-eligible for Medicaid payment of nursing care using
the medical assistance income trust.
If the total income received by the beneficiary (including income received by or generated by the
trust) equals or is greater than 125 percent of the applicable statewide average charge for
care, Iowa law directs the trust to make the following payments, in the following order:
1. A reasonable amount may be paid or set aside for trust administration fee, not to exceed
$10 per month without court approval. This payment is not considered income to the client.
2. All remaining amounts paid into the trust or retained from prior months must then be paid
out to the beneficiary. This payment is considered as income to the beneficiary for Medicaid
eligibility purposes. (Use this income to calculate eligibility.)

Title 8: Medicaid Page 44
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Members With a Medical Assistance Income Trust (MAIT)
Mr. Y is a resident of a nursing facility at nursing facility level of care. His gross monthly
income consists of social security benefits of $2,277, a civil service pension of $4,500, and
income from his farm (homestead) of $2,980. His total gross monthly income of $9,757 is
deposited into a medical assistance income trust.
Mr. Y’s total income is greater than 125 percent of the average charge for nursing facility care.
The trust will take $10 in administration fees and pay the remaining as income to Mr. Y. Mr. Y
is not income-eligible for Medicaid payment of nursing facility care because his income still
exceeds program limits.
NOTE: Use form 470-4678, MAIT Facility Worksheet, to calculate client participation for members
who reside in a medical institution and have a MAIT. Use form 470-4679, MAIT Waiver
Worksheet, to calculate client participation for members who are eligible for a home- and
community-based services (HCBS) waiver and also have a MAIT.
Determination of Client Participation
When determining client participation for a person with a medical assistance income trust, count
only the income to be paid from the trust or otherwise made available to the member as income
to the member. Do not count as income to the member:
▪ The gross monthly income paid into the trust.
▪ Direct client participation payments the trust makes to the facility or waiver service
provider or programs for all-inclusive care for the elderly (PACE) provider.
When the member’s gross monthly income is less than 125 percent of the statewide charge for
the care the member receives (see 125 Percent of the Statewide Average Charge for Care):
▪ Enter 300% of the SSI limit on the ABC system’s BCW2 screen with an income indicator of
“S” for eligibility.
▪ Enter social security on the ABC system’s BCW2 screen with an income indicator of “B”
and the total of all other income with an income indicator of “X” for benefits.
▪ Enter the following deductions for benefits:
• Trust administration fee
• Spouse and dependent needs
• Unmet medical expenses

Title 8: Medicaid Page 45
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Members With a Medical Assistance Income Trust (MAIT)
Mr. R is a single person in a nursing facility. His income consists of $1,377.70 gross social
security benefits and $2,200.00 in pension, for a total of $3,577.70 per month. He has
Medicare and a supplemental health insurance. The Medicare premium of $174.70 is
withheld from his social security check. The supplemental policy premium of $200 per
month is withheld from his pension check.
Mr. R’s nursing facility costs are $3,500 per month. He contacts an attorney and
establishes a medical assistance income trust. His $1,203 net social security check
($1,377.70 - $174.70 = $1,203) and $2,000.00 net pension check ($2,200.00 less $200.00
private insurance premium) are deposited to the trust.
The total income that is deposited into the trust account is $3,203. The additional
$374.70 withheld from his checks is countable income that is not deposited to the trust.
Calculate the amount of income left in trust after trust administration fees by subtracting
the fee from the total deposited into the trust.
$ 3,203.00
- 10.00
$3,193.00
Total net amount deposited into trust
Trustee retains $10 trust administrative fee
Income remaining in trust
Of the remaining $3,193, the trustee makes $50 available to Mr. R for his personal needs.
The trustee pays the remaining $3,143 in the trust directly to the nursing facility up to
the Medicaid rate.
ABC system entries:
▪ $2,829.00 (300% of the SSI benefit level) is entered on the BCW2 screen with an
income indicator of “S” for eligibility.
▪ $1,377.70 is entered on the BCW2 screen with an income indicator of “B,” and
$2,200.00 is entered with an income indicator of “X” for benefits only. $200 is
entered in DEDUCT2 field as an unmet medical expense for benefits only. $10 is
entered in the DEDUCT PAY field as the trust administration fee.
▪ When the member’s gross monthly income is equal to or greater than 125 percent of
the statewide charge for the care the member receives (see 125 Percent of the Statewide
Average Charge for Care):
• Enter gross income with an income indicator of “S” for eligibility and benefits on the
BCW2 screen. The income exceeds the 300% amount, so the case will be denied or
canceled from facility care and Medicaid.
• Enter any income retained by the member or withheld but continues to be counted as
income on the BCW2 screen with the applicable income indicator for both eligibility and
benefit.
• Process the case for other coverage groups, including Medically Needy, to pay for other
medical costs, unless the household has requested otherwise.

Title 8: Medicaid Page 46
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Members With a Medical Assistance Income Trust (MAIT)
1. Mr. Z is a resident of a nursing facility. He has social security benefits of $2,488, a
civil service pension of $4,209, and $3,000 from a private person, for a total gross
monthly income of $9,697.
Mr. Z establishes a medical assistance income trust. His income is greater than 125
percent of the statewide average charge for care. The trust pays the $10
administration fee and pays the remaining $9,687 to Mr. Z. This payment is
counted as income to Mr. Z when determining Medicaid eligibility and benefits.
2. Mr. G enters a nursing facility on July 1, 2017, leaving Mrs. G at home. His income
consists of $1,900 in social security and $933 in civil service pension. Mrs. G’s
income consists of $210 social security. Mr. G applies for Medicaid payment for
nursing facility care. The worker explains the income limit and Mr. G sets up a
medical assistance income trust to receive all of his income.
Spousal diversion calculation:
$ 3,853.50
- 210.00
$ 3,643.50
Minimum monthly maintenance needs allowance
Mrs. G’s income
Deficit to be met by diversion from Mr. G’s income to Mrs. G
Client participation calculation:
$ 2,833.00
- 10.00
- 50.00
$ 2,773.00
- 3,643.50
$ .00
Total income deposited to the trust
Trust administrative fee
Personal needs allowance
Total income available for diversion
Diversion to Mrs. G
Client participation
3. Mrs. C applies for waiver assistance. She lives with her husband and their child, age
10. Mrs. C’s income consists of $2,600 in social security and $950 in pension. Mr. C
has $2,000 in gross monthly earnings. A $250 monthly health insurance premium is
deducted from his earnings. This policy covers the whole family. Mrs. C meets level
of care for waiver assistance and establishes a MAIT that receives all of her income.
Spousal diversion calculation:
$ 3,853.50
- 2,000.00
$ 1,853.50
Minimum Monthly Maintenance Needs Allowance
Mr. C’s countable income
Amount of Mr. C’s deficit from MMMNA
Dependent diversion calculation:
$ 2,178.00
- 0.00
$ 2,178.00
150% FPL for 2
Child’s income
Divided by 3 = $726.00 maintenance for dependent
Client participation calculation:
$ 3,550.00
- 10.00
- 50.00
- 2,579.50
- 250.00
$ 660.50
Mrs. C’s gross income
Trust administration fee
Mrs. C’s personal needs allowance
Spouse and Dependent diversion ($1,853.50 + $726.00)
Unmet medical-health insurance premium
Waiver client participation

Title 8: Medicaid Page 47
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Members With a Medical Assistance Income Trust (MAIT)
If the institutionalized spouse’s income is above 125 percent of the statewide average charge, a
medical assistance income trust alone may not be sufficient to gain eligibility.
Mr. E enters a nursing facility at the NF level of care, leaving Mrs. E at home. He does not
receive specialized care. He has monthly income of $2,500 in social security, $4,500 in
IPERS benefits, and $3,000 from an annuity. Mrs. E’s income consists of $220 social
security. After Mr. E pays for nursing facility care and other medical bills, he has only $200
a month he can give to Mrs. E to live on.
Mr. E applies for Medicaid payment for nursing facility care. The worker explains the
income limit and that a medical assistance income trust will not help Mr. E qualify for
Medicaid. Since his income exceeds 125 percent of the statewide average charge, state law
requires that all income after the $10 trust administration fee is income to Mr. E, leaving
him over income for Medicaid.
The worker refers the couple to their attorney to determine if a qualified domestic
relations order will offer relief. Once the qualified domestic relations order is complete,
the ownership of some or all of the income will be changed to Mrs. E. Mr. E should file
another application at this time.
The worker obtains a copy of the order to determine which income sources changed to
Mrs. E’s ownership. Only the income owned by Mr. E is countable to him when
determining Medicaid eligibility and client participation.
Beneficiaries who have a Medicare premium deducted from their social security check are
considered to have received the premium amount. This is also true for people who have other
withholdings, such as union dues, taxes, and private health insurance.
When buy-in occurs, recalculate the client participation without the deduction for the Medicare
premium, effective with the month of buy-in. (See Effect of Buy-In, later in this chapter.)
Eliminate the Medicare premium deduction when calculating client participation for future
months.

Title 8: Medicaid Page 48
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Members With a Medical Assistance Income Trust (MAIT)
1. Mr. J is a single person in a nursing facility. His income consists of $1,522.70 gross
social security benefits and $2,500 in pension, for a total of $4,022.70 per month. He
has Medicare and a supplemental health insurance with a premium of $123.40 per
month. Mr. J’s nursing facility costs are $5,500 per month. He contacts an attorney and
establishes a medical assistance income trust.
Income to the trust:
$ 1,348.00
+ 2,500.00
$ 3,848.00
Net social security (gross of $1,522.70 less $174.70 Medicare equals
net amount of $1,358.00 rounded down)
Gross pension check
Total amount that is deposited into the trust
Client participation calculation:
$ 4,022.70
- 10.00
- 50.00
- 174.70
- 123.40
$ 3,664.60
Gross income
Trust administration fees
Personal needs allowance
Medicare premium
Health insurance premium
Client participation
Amount paid from the trust:
$ 3,848.00
- 10.00
- 50.00
- 123.40
$ 3,664.60
Total amount deposited into trust
Trust administrative fees
Personal needs allowance
Health insurance premium
Client participation
When buy-in occurs for Mr. J’s Medicare premium, the worker recalculates client
participation.
Income to the trust:
$ 1,522.00
+ 524.10
+ 2,500.00
$4,546.10
Gross monthly social security
Gross social security Medicare reimbursement check
Gross pension check
Total amount that is deposited into the trust account
Client participation and amount paid from the trust:
$ 4,546.10
- 10.00
- 50.00
- 123.40
$ 4,362.70
Total amount deposited into trust
Trust administrative fees
Personal needs allowance
Health insurance premium
Client participation in the month buy-in reimbursement is received
Ongoing client participation calculation:
$ 1,522.00
+2,500.00
$ 4,022.00
- 10.00
- 50.00
- 123.40
$ 3,838.60
Gross social security
Gross pension
Gross income
Trust administration fee
Personal needs allowance
Health insurance premium
Client participation

Title 8: Medicaid Page 49
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Members With a Medical Assistance Income Trust (MAIT)
2. Mr. K is a single person in a nursing facility. His income consists of $1,543.70 gross
social security benefits and $1,000.00 in pension, for a total of $2,543.70 per month.
He has Medicare and a supplemental health insurance. The health insurance premium
of $100 per month is withheld from his pension check. Mr. K’s nursing facility costs are
$5,500 per month.
Mr. K contacts an attorney and establishes a medical assistance income trust. Income
to the trust:
$ 1,369.00
+ 900.00
$ 2,269.00
Net social security (gross of $1,543.70 less $174.70 Medicare
rounded down)
Net pension check (gross $1,000.00 less $100 insurance premium)
Total amount that is deposited into the trust account
Client participation calculation:
$ 2,543.70
- 10.00
- 50.00
- 174.70
- 100.00
$2,209.00
Gross income
Trust administration fee
Personal needs allowance
Medicare premium
Health insurance premium
Client participation
Amount paid from the trust:
$ 2,269.00
- 10.00
- 50.00
$ 2,209.00
Total amount deposited into the trust
Trust administration fee
Personal needs allowance
Client participation
3. Mrs. D enters a nursing facility, leaving Mr. D at home. Mrs. D’s income consists of
$1,234.70 in social security and $1,940 in IPERS benefits. She has Medicare and a
supplemental insurance policy. The monthly premium for the supplemental policy is
$64. Mr. D’s income consists of $1,300 social security.
Mrs. D applies for Medicaid payment for nursing facility care. The worker explains the
income limit. The couple contacts an attorney and sets up a medical assistance income
trust to receive Mrs. D’s income.
Spousal diversion calculation:
$ 3,853.50
- 1,300.00
$ 2,553.50
Minimum monthly maintenance needs allowance
Mr. D’s income
Deficit to be diverted from Mrs. D’s income to Mr. D
Income to the trust:
$ 1,060.00
+ 1,940.00
$ 3,000.00
Net social security (Gross is $1,234.70 less $174.70 Medicare equals
net amount of $1,060.00 rounded down)
Gross IPERS
Total income that is deposited into the trust

Title 8: Medicaid Page 50
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Members With a Medical Assistance Income Trust (MAIT)
Client participation calculation:
$ 3,174.70
- 10.00
- 50.00
$ 3,114.70
- 2,553.50
561.20
- 238.70
$ 322.50
Mrs. D’s gross income
Trust administration fee
Personal needs allowance
Diversion to Mr. D
Unmet medical expense ($174.70 Medicare premium and $64 health
insurance)
Client participation
Amount paid from the trust:
$ 3,000.00
- 10.00
- 50.00
- 2,553.50
- 64.00
$ 322.50
Total amount deposited into trust
Trust administration fee
Personal needs allowance
Diversion to Mr. D
Health insurance premium
Client participation
When buy-in occurs for Mrs. D, the worker recalculates her client participation,
effective for the month of buy-in.
Income to the trust:
$ 1,234.00
524.10
+ 1,940.00
$ 3,698.10
Gross social security
Gross social security Medicare reimbursement check
IPERS
Total amount that is deposited into the trust account
Client participation and amount paid from the trust:
$ 3,698.10
- 10.00
- 50.00
- 2,553.50
- 64.00
$ 1,020.60
Total amount deposited into trust
Trust administrative fees
Personal needs allowance
Diversion to Mr. D
Health insurance premium
Client participation in the month buy-in reimbursement is received
Ongoing client participation and amount paid from the trust:
$ 1,234.00
+ 1,940.00
3,174.00
- 10.00
- 50.00
- 2,553.50
- 64.00
$ 496.50
Gross social security
IPERS
Income going into the trust
Trust administration fee
Personal needs allowance
Diversion to Mr. D
Unmet medical needs
Client participation
No recalculation is needed for members whose spousal deduction equals the income after the
personal needs allowance deduction, since no Medicare deduction was given.

Title 8: Medicaid Page 51
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Other Third-Party Payments
Other Third-Party Payments
Veterans Affairs (VA) aid and attendance payments are a third-party liability. They do not count as
income when determining eligibility, but do count in the client participation calculation. Enter any third-
party liability that is not considered income to the member as another income source in the benefit
calculation (separately from the income) on the ABC system’s BCW2 screen.
Third-party liability or other non-income sources may be included in benefit payments. For example,
veterans’ payments for aid and attendance, housebound allowance, or unusual medical expenses are
included with veterans’ pensions. These amounts should not be deposited into the trust. If the check
containing both payments is deposited into the trust account, the trustee should remove the non-
income portion of the payment and pay it to the beneficiary.
Mrs. V is a single person in a nursing facility. Her income consists of $2,980 in social security
benefits and $1,402 VA benefits. The payment from VA consists of $782 in VA pension and $620
in aid and attendance. Mrs. V has a Medicare premium.
Mrs. V contacts an attorney and establishes a medical assistance income trust. The income
deposited into the trust is the $2,980 social security benefit and $782 VA pension, for a total of
$3,762. The trustee removes the $620 aid and attendance and gives it to Mrs. V to pay the third-
party liability portion of the client participation.
Income to the trust:
$ 2,980.00
+ 782.00
$ 3,762.00
Gross Social Security
VA pension
Total income that is deposited into the trust
Client participation calculation:
$ 3,762.00
- 10.00
- 50.00
$ 3,702.00
+ 620.00
$ 4,322.00
Mrs. V’s gross income
Trust administration fee
Personal needs allowance
VA aid and attendance
Client participation
When there are income disregards for a community spouse as well as third-party liability, follow the
same order as for a case that does not have a trust.
Mr. C enters a nursing facility. He has monthly income of $2,400 social security, $442 IPERS
benefits, $731 VA pension, and $489 VA aid and attendance, none of which is attributable to
unusual medical expenses. Mrs. C, at home, gets $500 in social security.
Mr. C files an application for Medicaid payment for nursing facility care. The worker explains the
income limit, and Mr. C sets up a medical assistance income trust.
Spousal diversion calculation:
$ 3,853.50
- 500.00
$ 3,353.50
Minimum monthly maintenance needs allowance
Mrs. C’s income
Deficit to be met by diversion from Mr. C’s income to Mrs. C
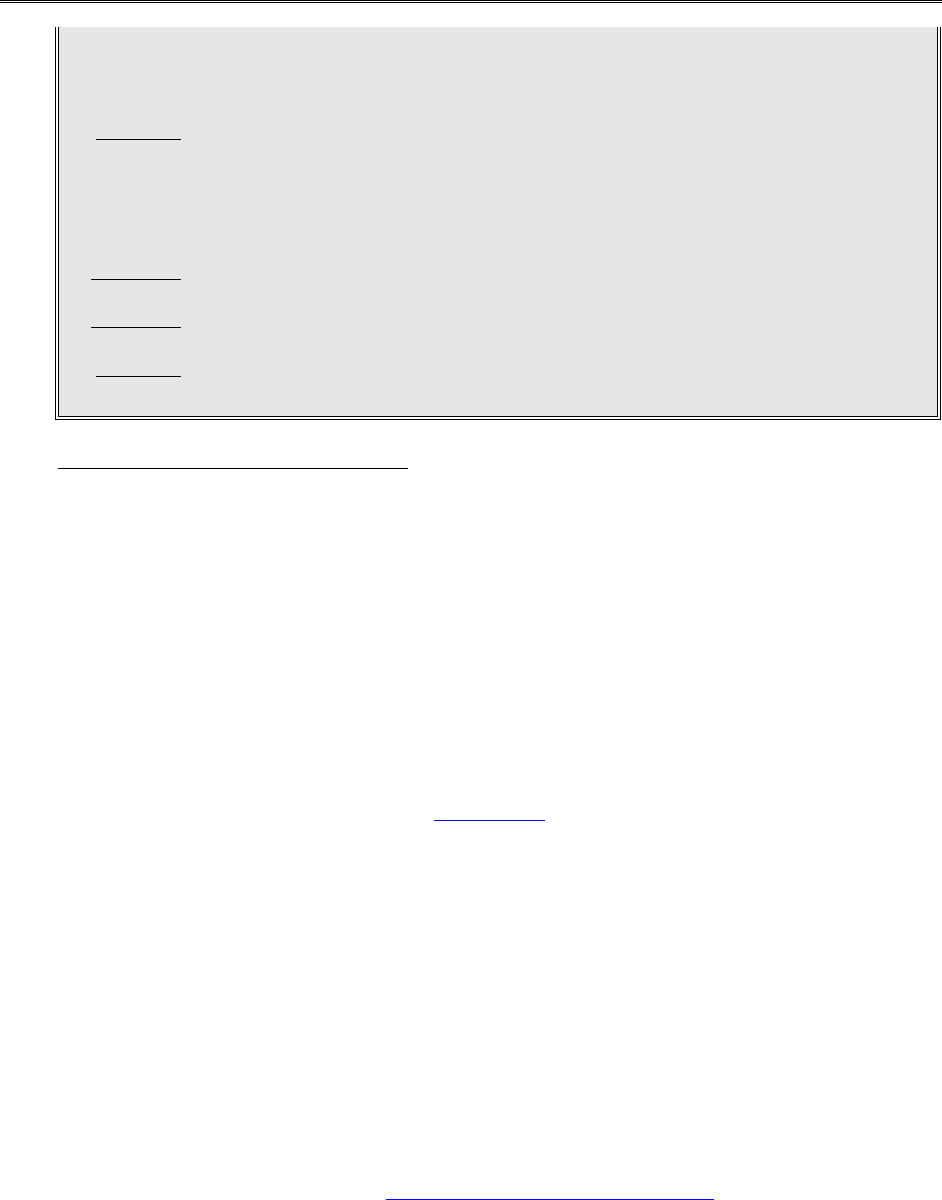
Title 8: Medicaid Page 52
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Other Third-Party Payments
Income to the trust:
$ 2,400.00
+ 442.00
+ 731.00
$ 3,573.00
Gross Social Security
IPERS pension
VA pension
Total income that is deposited into the trust
Client participation calculation:
$ 3,573.00
- 10.00
- 50.00
$ 3,513.00
- 3,353.50
$ 159.50
+ 489.00
$ 648.50
Mr. C’s gross income
Trust administration fee
Personal needs allowance
Income available for diversion
Diversion to Mrs. C
VA aid and attendance
Client participation
Changes in Client Participation
Legal reference: 42 CFR 435.725, 441 IAC 76 (Rules in Process)
Process changes in client participation for future months within ten days after receiving information of
errors in computation or changes in income or expenses. Consider all nonexempt income for client
participation in the current month.
Issue timely and adequate notice when client participation increases. Client participation adjustments
that cannot be made due to timely notice requirements may require vendor adjustments. The first step
in completing a vendor adjustment is to determine the cause of the error or incorrect payment and
calculate the correct amount of client participation.
If the income was not reported timely and Medicaid eligibility is affected, an overpayment has occurred
and recoupment should be completed. (See 8-A, Recovery.)
When the member remains eligible, the member is still obligated to pay the increased client
participation amount for the month that the client participation increases but timely notice could not
be given. Complete the following steps:
1. Recalculate client participation, taking into consideration the additional income in the month
received.
2. Manually issue a notice of decision telling the member to pay the additional client participation to
the facility.
3. Complete changes to the client participation in IoWANS, either by:
▪ Using the IoWANS Change Tool after completing the change for the current month in the
ABC system; or
▪ Completing and sending form 470-3924, Request for IoWANS Changes, to the DHS, IoWANS-
Facilities e-mail box.

Title 8: Medicaid Page 53
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Changes in Client Participation
4. If the facility reports that the member refused to pay the additional client participation, reverse the
client participation amount and complete a recoupment.
On March 24, Mr. W, a nursing facility member, receives a retroactive veterans payment of $2,000
and an award of $600 monthly veterans income. He reports this April 2. The worker changes client
participation on the system for May. Mr. W also owes extra client participation for March and April,
but no more than the state would pay for the care.
For computation of March client participation, the worker adds $2,000 to March’s income. For April,
the worker adds the monthly veterans income ($600) to April’s income. The worker notifies Mr. W
and the facility of adjusted client participation for March and April. When Mr. W pays the facility, the
worker corrects the amount on IoWANS for March and April.
When the member has paid too much client participation, prepare an adjustment to return the money
to the medical institution. The member collects the excess client participation from the facility.
If Lower Level of Care Is Needed
Legal reference: 441 IAC 75 (Rules in Process), 441 IAC 78.3(6), 441 IAC 78.3(14), 441
IAC 81.10(4)“g”
As described in Medical Necessity, the IME Medical Services Unit or the MCO may decide that a
member needs a lower level of medical care than the level provided by the facility where the
member lives. If the facility agrees to accept payment at the lower level, the member may stay in
the facility temporarily until placement at the correct lower level is found.
Assess client participation based on the type of facility in which the member lives. For members
in a hospital, do not assess client participation if the hospital is providing SNF or NF care in an
acute-care bed. If the hospital is a swing-bed hospital, the member is considered to be in a skilled
facility as long as the member needs skilled care. When the member does not need skilled care,
the bed “swings” back to an acute-care bed.
If a member is eligible or potentially eligible for Medicaid only under the Medically Needy
coverage group, there is no client participation, since Medicaid does not pay for institutional care
under Medically Needy.
See Payment for Inpatient Hospitals Who Require a Lower Level of Care for how to handle
payments to facilities when a member needs a lower level of care but an alternative placement
cannot be found.
1. Mr. G is in a hospital at acute level of care and is eligible for Medicaid. It has just been
determined that he no longer needs acute hospital care but needs skilled care. The
hospital is not a skilled care provider, but provides skilled care for Mr. G until an
appropriate placement is available.
Mr. G’s client participation for skilled care would normally be $695 per month but since
Mr. G is receiving a lower level of care in a hospital, he does not owe any client
participation.

Title 8: Medicaid Page 54
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Changes in Client Participation
2. Ms. F is Medicaid member in a nursing facility with $250 monthly income. The IM
Medical Services Unit determines that she does not need care in a medical facility. She
is seeking appropriate placement. She remains eligible for Medicaid nursing facility
payment. Her client participation is determined by subtracting $50 personal needs and
her $30 medical insurance payment from her gross income.
3. The IM Medical Services Unit determines that Mrs. M no longer needs nursing care
but she does need residential care. The facility agrees to keep her at the lower level of
care and accept the RCF rate. The Department agrees to pay the lower level of care
amount while Mrs. M is looking for another placement. The worker keeps the case
under the nursing facility aid type, with the nursing care MED CP code and the nursing
facility vendor number.
Effect of Buy-In
Legal reference: 42 CFR 435.725(c)(4), 441 IAC 75 (Rules in Process)
Initially determine income for client participation based on the gross amount of social security or
railroad retirement benefits. Consider any amounts withheld for overpayments as income.
After the Department completes the buy-in process to pay the cost of Medicare Part A or Part
B, change the social security or railroad retirement income to indicate that the member no
longer pays this cost. Do not allow the Medicare premium as a deduction. The ABC system may
automatically reflect this adjustment.
The member is issued a refund check for the Medicare premium costs in the same month that
the buy-in occurs. The social security check increases in the next month. You will receive a
Bendex form to show completion of the buy-in when the social security income changes.
The Medicare premium refund check is counted as a nonrecurring lump sum. Count the refund
as income in the month received.
1. Mr. B enters a nursing facility on January 15 and is approved for Medicaid as of his
date of entry. Mr. B receives $811.00 gross Social Security before buy-in. Mrs. B
remains at home and receives $605.00 gross monthly Social Security. Mr. B’s client
participation before buy-in is calculated as follows:
$ 3,853.50
- 605.00
$ 3,248.50
Minimum monthly maintenance needs allowance
Mrs. B’s social security
Deficit to be diverted from Mr. B’s income to Mrs. B
$ 811.00
- 50.00
$ 761.00
- 761.00
$ 0.00
Mr. B’s social security
Personal needs allowance
Mr. B’s income available to divert to Mrs. B
Diversion to Mrs. B
Mr. B’s income available for unmet medical diversion and client
participation

Title 8: Medicaid Page 55
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Changes in Client Participation
Mr. B’s gross social security is used to determine client participation, but Mr. B does
not have enough income to divert the entire allowable spousal diversion to Mrs. B
($3,248.50 was the monthly shortfall but the actual amount will be $761.00, or all of
Mr. B’s income after deductions).
Buy-in occurs in April. Mr. B receives a Medicare premium refund check on April 17
for $698.80. Since Mr. B’s gross social security income was used to determine client
participation and the entire allowable spousal diversion was not received, the
Medicare premium refund check can be paid to Mrs. B.
2. Mr. D enters a nursing facility on March 21 and is approved for Medicaid as of his date
of entry. Mr. D receives $1,951.00 gross social security before buy-in. Mrs. D remains
at home and receives $908.00 gross Social Security and a $1,250 gross monthly
pension. Mr. D’s client participation before buy-in is calculated as follows:
$ 3,853.50
- 2,158.00
$ 1,695.50
Minimum monthly maintenance needs allowance
Mrs. D’s gross income
Deficit to be diverted from Mr. D’s income to Mrs. D
$ 1,951.00
- 50.00
$ 1,901.00
- 1,695.50
$ 205.50
Mr. D’s social security
Personal needs allowance
Mr. D’s income available to divert to Mrs. D
Diversion to Mrs. D
Mr. D’s income available for unmet medical diversion and client
participation
Only $1,695.50 of Mr. D’s income is available for the spousal diversion.
Buy-in occurs in June. Mr. D receives a Medicare premium refund check on June 15
for $698.80. Since Mr. D was able to divert enough of his income back to Mrs. D to
bring her to the MMMNA amount, Mr. D will need to pay $698.80 additional client
participation to the facility.
Timely and adequate notice must be given when client participation increases. The member is
still obligated to pay the increased client participation amount for the month that the payment
was received.
Although the ABC system has been designed to complete buy-in automatically, there may be
cases that the system cannot handle. To manually complete buy-in, please follow the steps
below:
1. Calculate the correct amount of client participation for the current month that included the
refund received due to buy-in. This will be the 1ST CP AMT when making ABC entries.
2. Calculate the correct client participation for ongoing months. This will be the ONGO CP
amount when making the ABC entries.
3. Complete ABC entries according to 14-B(9), Changing Client Participation: Manual.
4. Send a manually prepared Notice of Decision: Medical Assistance or State Supplementary
Assistance, form 470-0490. Use the comments section of the notice to explain that member
owes additional client participation for the current month due to receipt of the refund.

Title 8: Medicaid Page 56
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Changes in Client Participation
5. If a member does not pay the facility the additional client participation for the current
month, complete form 470-3924, Request for IoWANS Changes, to reduce the client
participation back to the original amount and establish an overpayment for the amount
owed.
If the Member Receives a Lump Sum
Count a nonrecurring lump-sum payment in the month the payment is received. Send a notice
telling the member to pay the difference between the client participation already assessed and
either the redetermined client participation or the maximum Medicaid reimbursement rate to
the facility, whichever is less.
Prorate a recurring lump-sum payment over the period it is intended to cover. Do not count
any lump-sum income received before the month Medicaid eligibility is granted.
If a member receives a lump-sum VA check, divide the check into pension and aid and
attendance. The pension portion is income in the month of receipt, regardless of the months it is
intended to cover. The aid and attendance portion is a medical payment for the months the
lump-sum payment is intended to cover.
Send a notice showing the new client participation for ongoing months and the additional
payment for the back months. The member pays the difference between the assessed client
participation and either the Medicaid payment or the redetermined client participation,
whichever is less.
Complete vendor adjustments for the pension portion and the VA aid and attendance after the
member repays the facility.
Determine the maximum Medicaid reimbursement rate by multiplying the per diem rate of the
facility (from the MMIS screen) by the number of days in the month. Adjust the per diem rate for
any reserved bed days or days that Medicaid would not pay due to the member’s absence from
the facility exceeding reserved bed days.
When the payment is made to the facility, completes form 470-3924, Request for IoWANS
Changes for each of the months involved.
1. In October, Mrs. Z receives a retroactive VA payment for $2,500. This amount is all
pension money; no VA aid and attendance is included. Mrs. Z’s client participation is
$300 and she has paid this for the month of October. The maximum Medicaid
reimbursement rate for the facility for October is $1,900.
The worker considers the VA amount a lump sum in October and notifies Mrs. Z to
pay $1,600 to bring the total payments by Mrs. Z to the maximum Medicaid
reimbursement rate to the facility for the month of October. The worker completes a
Request for IoWANS Changes for October.

Title 8: Medicaid Page 57
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 14, 2023 Changes in Client Participation
2. Mrs. A receives a retroactive VA payment in December for $8,700. $2,500 is for VA
aid and attendance for August through December. The remainder of this, $6,200, is
pension.
Mrs. A’s client participation is $800 per month. The worker considers $6,200 pension
and $500 VA aid and attendance when determining client participation for December.
The maximum Medicaid reimbursement rate for the facility is $1,922. The worker
sends a notice to Mrs. A to pay $1,122 to the facility to bring her total client
participation for the month of December to the maximum Medicaid reimbursement
rate.
The worker completes a Request for IoWANS Changes for December.
The worker recalculates client participation for the months of August through
November using the VA aid and attendance, which equals $500 per month. The
worker sends a notice to Mrs. A to pay $500 per month for each month August
through November. The worker completes a Request for IoWANS Changes for
August through November.
If the Member Leaves or Transfers Facilities
Legal reference: 42 CFR 435.725, 441 IAC 81.5(1), 441 IAC 81.13(6)“a,” 441 IAC 82.10(1),
441 IAC 85.6(249A)
A member who transfers from one medical institution to another in the same month must pay
any unused client participation to the new institution.
If the member transfers from a medical institution to a residential care facility (RCF), the
member pays unused client participation computed for the medical institution to the RCF.
If a member transfers from an RCF to a medical institution in the same month, the member pays
the unused client participation computed for the RCF to the medical institution.
To determine the amount of unused client participation:
1. Find the per diem rate of the facility in which the member lived during the first part of the
month. Multiple the rate times the number of days in that facility. Do not include the day of
discharge, because Medicaid does not pay for the discharge day.
2. Subtract this amount from the member’s previously calculated total client participation. If
any amount remains, this is the unused client participation and must be paid to the second
facility.
If a member transfers from an RCF to a medical institution, do not make an adjustment to client
participation to allow for the decreased personal needs allowance in a medical institution. The
member is allowed to retain the higher personal needs allowance for the month of transfer, but
client participation must be recomputed for the month following the month of transfer.

Title 8: Medicaid Page 58
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Changes in Client Participation
1. Mrs. M transfers January 6 from skilled care to regular nursing care. Her client
participation is $540. Her client participation for each type of care is computed as
follows:
Per diem for skilled care = $90
$90 x 5 = $450 owed for skilled care
$ 540.00
- 450.00
$ 90.00
Ms. M’s client participation
Owed for the skilled care
Available to pay for the nursing care
2. Mrs. Q transfers from an RCF to a nursing facility on July 5. Her client participation at
the RCF is $500. The RCF rate is $19 per day. She owes $76 to the RCF for the
month of July ($19 x 4 days). Her client participation to the nursing facility is $424
($500 client participation - $76 for the RCF = $424).
If a member goes home and is approved for either Programs for All-Inclusive Care for the
Elderly (PACE) or waiver services in the month of discharge from the facility, adjust the facility
client participation to allow for the increased personal needs allowance in the month of
discharge. Calculate waiver client participation according to 8-N, Client Participation and allow a
deduction for client participation paid to the medical facility in the month of discharge.
1. Mrs. N has $900 social security income, is discharged from a nursing facility on June 5,
and is approved for waiver services the same month.
Nursing facility client participation calculation:
$ 900.00
- 50.00
- 841.00
$ 9.00
Social security
Personal needs allowance
Personal needs in month of discharge
Nursing facility client participation
Waiver client participation calculation:
$ 900.00
- 2,829.00
$ 0.00
Social security
Waiver maintenance allowance
Waiver client participation
2. Mr. O, who has a MAIT and $3,000 gross monthly income, is discharged from nursing
facility on June 15 and is approved for waiver services on June 28. The nursing facility
per diem rate is $175.
Nursing facility client participation calculation:
$ 3,000.00
- 10.00
- 50.00
- 943.00
$ 1,997.00
Gross income
Trust administration fee
Personal needs allowance
Personal needs in month of discharge
Nursing facility client participation (Actual cost of care is $2,450
($175.00 per diem x 14 days))

Title 8: Medicaid Page 59
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Client Participation
Revised April 5. 2024 Changes in Client Participation
Waiver client participation calculation:
$ 3,000.00
- 10.00
- 2,829.00
161.00
- 1,997.00
$ 0.00
Gross income
Trust administration fee
Waiver maintenance allowance
Remaining income
Unmet medical deduction for nursing facility client participation paid
Waiver client participation
3. Same as Example 2, except that Mr. O’s discharge date is June 2.
Nursing facility client participation calculation:
$ 3,000.00
- 10.00
- 50.00
- 943.00
$ 1,997.00
Gross income
Trust administration fee
Personal needs allowance
Personal needs in month of discharge
Nursing facility client participation (Actual cost of care is $175 ($175.00
per diem x 1 day))
Waiver client participation calculation:
$ 3,000.00
- 10.00
- 2,829.00
161.00
- 175.00
$ 00.00
Gross income
Trust administration fee
Waiver maintenance allowance
Remaining income
Unmet medical deduction for nursing facility client participation paid
Waiver client participation
4. Mr. P is a PACE enrollee residing in an ICF/ID. He has $3,000 in gross monthly income
which is deposited into a MAIT. He is discharged from the ICF/ID on July 10. He re-enters
ICF/ID on August 25.
July PACE client participation:
$ 3,000.00
- 10.00
- 50.00
$ 2,940.00
Gross trust income
Trust administration fee
Personal needs allowance
PACE client participation for institutionalized enrollee
Adjusted PACE client participation for the month of ICF/ID discharge
$ 3,000.00
- 10.00
- 50.00
- 943.00
$ 1,997.00
Gross trust income
Trust administration fee
Personal needs allowance
Personal needs in month of discharge
Recalculated PACE client participation for July
August PACE client participation:
$ 3,000.00
- 10.00
- 2,829.00
$ 161.00
Gross trust income
Trust administration fee
Maintenance allowance
PACE client participation for August (no adjustment is made in the
month of institutionalization)

Title 8: Medicaid Page 60
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Qualified Medicare Beneficiaries in Skilled Care
Revised April 14, 2023
Qualified Medicare Beneficiaries in Skilled Care
Legal reference: P.L. 100-360, 441 IAC 75 (Rules in Process), 441 IAC 76.13(1)“a”
For people whose only Medicaid eligibility is under the qualified Medicare beneficiary (QMB) coverage group,
Medicaid pays only for the Medicare Part A and Part B premiums, coinsurance and deductibles. If a person is
receiving skilled care or hospital care, Medicare pays the cost of care within certain limits. (See Medicare
Coverage for Institutional Care for payment limits.)
Eligibility for QMB applicants begins the month after the month of decision. The person is not eligible for
Medicaid payment until the month following the month of decision unless the worker determined Medicaid
eligibility under another coverage group.
Some members may be concurrently eligible for QMB and another Medicaid coverage group. Examples of
these members include:
▪ SSI recipients with Medicare
▪ People in the 300% group with Medicare
▪ FIP recipients with Medicare
When a person is concurrently eligible both for skilled care payments under a nursing facility aid type and for
QMB benefits on the date of entry, the person has no client participation until Medicare is exhausted.
Medicaid payment for skilled care stops for a person who is only QMB-eligible when the Medicare is
exhausted.
A member who is eligible for SSI, FIP, or FMAP and has Medicare Part A has already been determined eligible
as a QMB member. No QMB application is needed.
In order for Medicare to make skilled care payments, the member must be hospitalized for three days and
enter skilled care within 30 days of leaving the hospital. If this requirement is not met, Medicare does not pay
for skilled care and QMB also does not pay, because there is no coinsurance. Determine eligibility under
another coverage group. The member does have client participation under the other coverage group.
If you are examining eligibility under both QMB and the 300% group for a person who is not a QMB member
when the person enters skilled level of care, determine whether the 30-day stay or QMB eligibility happened
first.
Initially approve eligibility for the coverage group under the eligibility that occurred first. If a client is eligible
for QMB and the 300% group, approve eligibility for the 300% aid type and enter the percent of poverty in
the poverty level indicator field. If the member wants QMB assistance only, do not approve 300% group
coverage.

Title 8: Medicaid Page 61
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Qualified Medicare Beneficiaries in Skilled Care
Revised April 14, 2023 Client Participation for QMBs Entering Skilled Care
1. Mr. and Mrs. P are QMB-eligible in July. Mr. P enters a nursing facility (not receiving skilled level of care)
where he is expecting to stay indefinitely. Mr. P is considered a single person for QMB eligibility for the
month of July, or is evaluated under the program of his choice. Eligibility for Mrs. P must be reexamined
after the resource determination is made for Mr. P.
2. Mr. C, age 83, enters a hospital February 1 and then enters a nursing facility at the skilled level of care
and applies for Medicaid on February 4. He receives $385 monthly in social security benefits. He is
eligible for and receiving Medicare benefits. Mr. C’s countable resources are $3,800 as of February 1.
He is not resource-eligible for any SSI-related coverage group except for QMB and Medically Needy.
The IM worker explains that due to the amount of his countable resources, the only Medicaid coverage
group for which he may be eligible that would pay for his cost of care is QMB. Mr. C is also eligible for
Medically Needy. The Medically Needy program will pay for services other than the cost of facility care.
The worker approves eligibility on February 28, with the Medically Needy program effective February 1
and a QMB effective date of March 1. The worker enters the approval with the Medically Needy aid
type (37-E).
The ABC system establishes QMB eligibility for March based on the coding and poverty level indicator
and the date of entry. No client participation or any other facility entries are made on the ABC system,
because they do not apply under QMB or under Medically Needy.
Mr. C is responsible for paying the coinsurance for February 24-28, which is before the QMB effective
date. If Mr. C’s resources still remain in excess of Medicaid limits after Medicare pays for the 100 days,
he is totally responsible for paying his own cost of care.
3. Mr. W, age 68, enters a hospital on February 1, and then enters a nursing facility at the skilled level of
care on February 5. He applies for QMB on the same day. He is approved for QMB March 1, with an
effective date of April 1.
If Mr. W needs help with the cost of skilled care for February and March, he must be determined
eligible under the 300% group or as a person who would be eligible for SSI or SSA, if not in a medical
institution.
Client Participation for QMBs Entering Skilled Care
Legal reference: 441 IAC 75 (Rules in Process)
When an application is for QMB and skilled care payment, assess client participation until QMB
eligibility becomes effective. When the person becomes QMB eligible, access zero client participation
while Medicare is paying for the cost of the skilled care and Medicaid pays the copayment.
If Medicare coverage has not been exhausted, you may need to enter zeros in the first-month client
participation and ongoing client participation fields. This prevents the facility from overcharging the
member and provides the Iowa Medicaid Enterprise (IME) with the correct payment amount. See
Client Participation for Skilled Care.
You may contact the Medicare intermediary to verify the number of days to be paid by Medicare. You
need a signed release of information to contact the intermediary.
The facility will complete the Case Activity Report to verify the number of days to be paid by Medicare.

Title 8: Medicaid Page 62
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Qualified Medicare Beneficiaries in Skilled Care
Revised April 14, 2023 Client Participation for QMBs Entering Skilled Care
Manually issue a notice to notify the applicant of the client participation amount for days 21 through
100 and to tell the applicant that client participation will not be charged until Medicare coverage is
exhausted. Include the following wording:
“Medicare and Medicaid will pay for the cost of care in the facility until Medicare coverage ends. If you
remain at this level of care after Medicare coverage ends, you will be charged for part of the cost of care.
The client participation amount on this notice is the amount you will be responsible for paying the facility
each month after the Medicare payments end.”
When the Medicare coverage has been exhausted and the client is concurrently eligible for payment at
the skilled level of care under a facility aid type, enter client participation into the ABC system. Allow
deductions, including personal needs in the month of entry to the facility.
Enter the first month and ongoing client participation on the ABC system effective the day after
Medicare coverage ends. For this purpose, “first month” means the first month that the member has to
pay client participation. This usually is not the month that the member entered the facility.
1. Ms. P, age 78, applies for Medicaid on March 5. She reports that she entered the hospital on
March 1 and transferred to skilled care on March 5. The worker verifies that Ms. P began a new
spell of illness as of March 1.
The worker processes the application under the 300% group. The worker approves eligibility for
QMB on March 22, effective April 1, and for the 300% group on April 4, effective March 1. The
worker calculates client participation for March 5 (first month) and the ongoing months.
The worker enters the client participation for the first month on TD05, because Ms. P was not
QMB-eligible for March. The worker enters zero client participation for the ongoing months, and
enters a tickler for the month before the 101st day so that client participation can be reentered
on the ABC system.
Ms. P is issued a notice informing her of the client participation for March and ongoing months,
and that she will not be responsible for paying client participation after March until Medicare is
no longer paying the facility. On the 101st day, she must pay client participation.
2. Mr. B, a QMB Medicaid member, enters skilled level of care on January 15. Mr. B asks that the
worker determine whether another coverage group would be more advantageous for his
situation. Since Mr. B is still receiving skilled care on February 15, the IM worker determines that
eligibility also could exist under the 300% group. He chooses the 300% group.
Since Mr. B is QMB-eligible and was hospitalized for a week before entering skilled level of care,
he has Medicare coverage for 100 days of skilled care. Medicaid pays the Medicare coinsurance
for days 21 through 100.
If the Medicaid rate is higher than the Medicare rate, the IM worker computes client participation
but enters zeros on the ABC system for the first month and ongoing client participation. The
poverty level indicator is also entered. The ongoing client participation amount is entered on the
notice of decision.
If Mr. B still lives in a nursing facility receiving skilled care after the 100-day period covered by
Medicare, no change in aid type is required. The IM worker enters the already computed client
participation on the TD05 screen. NOTE: If this were a new applicant, there would be client
participation charged for January.

Title 8: Medicaid Page 63
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Qualified Medicare Beneficiaries in Skilled Care
Revised April 14, 2023 Client Participation for QMBs Entering Skilled Care
3. Ms. L is currently receiving Medicaid as a Medically Needy member and is QMB eligible. There is
no spenddown. On March 5, Ms. L reports that she entered the hospital on February 15 and
entered a skilled level of care on March 1. Ms. L continues to be QMB-eligible.
Eligibility can be established under the 300% group after the 30-day residency requirement is met.
No facility entries are made until there is eligibility in a 300% aid type. After eligibility for the
300% group has been met on March 16, the IM worker closes the Medically Needy case on the
ABC system and reopens the case with a 300% aid type.
Zeros are entered for the first month and ongoing client participation fields if Medicare is paying
for the cost of care and the Medicaid rate is higher than the Medicare rate.
The IM worker computes client participation for the ongoing months and informs Ms. L on the
notice when she will be required to pay client participation to the facility and the amount she will
be charged.
4. Mrs. N is eligible for Medicaid as part of the 300% group and also has QMB eligibility. The nursing
facility reports that Mrs. N no longer needs skilled level of care on June 4. On July 4, she again
meets skilled level of care after having been hospitalized for three days. A new benefit period has
not started for Mrs. N. The facility reports that Mrs. N has used all but ten days of Medicare
entitlement for skilled level of care.
No changes are needed unless the Medicaid rate is higher than the Medicare rate. In August, Mrs.
N is required to pay the facility $350 in client participation per month.
5. Mr. G, age 79, enters a hospital on May 27, then transfers to a nursing facility on May 30 receiving
skilled care. He applies for Medicaid for help to pay for the cost of care. On July 1, the IM
worker determines that he is both eligible under the 300% group and QMB-eligible.
Medicare pays for the cost of care from May 30 through June 18. Since QMB cannot be effective
until August 1, Mr. G is responsible for paying client participation from June 1 through July 31.
Medicaid will pay the Medicare coinsurance beginning August 1. If the Medicaid rate is higher than
the Medicare rate, change the client participation to zero effective August 1.
The IM worker enters the amount of client participation for May, June, and July, because these
months are before QMB eligibility.
The worker also enters the poverty level indicator. The following day, after the client
participation is entered on TD05, the worker enters zeros for the month of August when
applicable. Zeros remain in the client participation fields until Medicare is no longer paying for the
cost of care.
The worker does a tickler for September 8 so that client participation entries can be made on
the ABC system.
The worker issues a manual notice to inform Mr. G that he is responsible for paying client
participation for May, June, and July, and that he will be responsible for client participation when
Medicare is no longer paying the facility after the 100th day.

Title 8: Medicaid Page 64
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Billing and Payment
Revised April 14, 2023
Billing and Payment
Legal reference: 441 IAC 79.1(249A), 441 IAC 80.2(249A), 441 IAC 80.3(249A), 441 IAC 81.10(5), 441
IAC 81.11(1), 441 IAC 81.22(2), 441 IAC 82.14(4), 441 IAC 82.15(1)
When a resident becomes eligible for Medicaid payment for facility care, the facility must accept Medicaid or
MCO contracted rates effective with the date the resident’s Medicaid eligibility begins. A nursing facility is
required to refund any payment received from a resident or family member for any period of time during
which the resident is determined to be eligible for Medicaid.
If the beginning Medicaid eligibility date is a future month, the facility must accept the Medicaid rate effective
the first of that future month.
NOTE: When a resident enters skilled care in a facility outside the state of Iowa, refer the facility to the
Bureau of Medical and Long Term Services and Supports to obtain approval of out-of-state skilled payments.
Nursing facility services can be paid for many Medicaid members who are nonfacility aid types in the month
of entry into the facility and for short stays. A “short stay” means less than 30 days. Also, people in nursing
facilities may go back and forth between facilities. If the worker is not informed of these changes, payment
may be delayed or not made at all.
In both instances, an IoWANS file must be created or updated and transferred to the Iowa Medicaid
Enterprise (IME) before payment for the appropriate facility care can be made.
When a Medicaid member in a nonfacility aid-type is admitted to a medical institution and continues care at
the medical facility the month following the month of admission, and you are informed before the discharge,
close the regular Medicaid case. (Enter code 401 in the MED RSN2 field on the ABC TD05 screen.) Complete
an automatic redetermination and reopen the case beginning the date of admission under the applicable
facility aid type.
When a Medicaid member in a nonfacility aid type is admitted to a medical institution and continues care the
month following the month of admission, but you are informed after the discharge, do not close the regular
Medicaid case. Complete an automatic redetermination for the applicable facility aid type.
Follow these steps to get authorization into IoWANS:
1. Complete a manual notice of decision showing the approval and the cancellation on the same notice.
2. Complete form 470-3924, Request for IoWANS Changes, and e-mail it to DHS, IoWANS-Facilities. The
form must include:
▪ The member’s name, case number, and state identification number.
▪ The facility name and vendor number.
▪ The dates of service (admission and discharge dates).
▪ The client participation amount (for each vendor and stay).
Remember that the 30 day stay requirement is for a person in the 300% group. Many Medicaid members in
nonfacility aid types do not need to meet this requirement, unless they are redetermined to the 300% group.

Title 8: Medicaid Page 65
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Billing and Payment
Revised April 14, 2023
When you are informed that a nursing facility member moved to a different facility (and is still there),
complete an automatic redetermination for the new, appropriate aid type. Make changes to the ABC case to
record the move.
When a nursing facility member is admitted to a different facility but returns to the original facility, and you
are informed of the moves after the member has returned, do not close the current case. Complete an
automatic redetermination for the care the member received in the other facility.
If a significant amount of time has passed and you are unable to update ABC all the way back to the original
admission date, follow these steps to get authorization into IoWANS:
1. Complete a manual notice of decision showing the approval and the cancellation to any facility stays that
are in the past.
2. Complete form 470-3924, Request for IoWANS Changes, and e-mail it to DHS IoWANS-Facilities. The
form must include:
▪ The member’s name, case number, and state ID number.
▪ The facility name and vendor number.
▪ The dates of service (admission and discharge dates).
▪ The client participation amount (for each vendor and stay).
Provider Rates
Facilities have an established rate based on their cost report. The fee-for-service rate for each facility
provider can be found by viewing the IoWANS My Reports screen. For client participation purposes,
use the rate on IoWANS My Reports screen for the facility in which the member resides.
Billing Process
Legal reference: 441 IAC 81.11(1), 441 IAC 82.15(1)
See 14-B(9), Facility Case Actions: Approving an Application for the appropriate ABC entries to make when
a person becomes eligible for Medicaid payments for institutional care. The facility can view a
member’s client participation through Iowa Medicaid Provider Access (IMPA). IMPA allows the facility
to view client participation that a member residing in their facility is required to pay.
Fee-for-service claims for medical institution care are submitted to the Iowa Medicaid Enterprise (IME).
The claims can be submitted any time after the end of the month of service. The facility is responsible
for billing other payers before filing a Medicaid claim. Payments are mailed from the IME after the
claims are approved. Medicaid is the payer of last resort.
For members enrolled in managed care, providers submit claims to the appropriate MCO.
Payment is made only for those services or for the part of the cost of a service for which no other
payer exists. Any health insurance, Medicare, client participation, or other payments made to the
facility by the member, relatives, or other source is deducted before payment is made.

Title 8: Medicaid Page 66
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Billing and Payment
Revised April 14, 2023 Payment for Reserve Bed Days
Payment for Reserve Bed Days
Legal reference: 441 IAC 81.10(4), 441 IAC 82.14(4)
Different limits apply to payments to reserve a bed in a nursing facility or an ICF/ID during a member’s
absence. No reserve-bed payments are allowed for nursing facilities, hospitals or MHIs.
Nursing Facilities
Legal reference: 441 IAC 81.10(4)“f”
Effective December 1, 2009, Medicaid no longer pays for reserved bed days in nursing facility for
persons at the NF/ICF level of care.
Skilled care is a level of care received by residents of a nursing facility. The number of bed-hold
days is the same when a resident is receiving skilled care. The resident is not required to receive
skilled care for 90 days before the bed-hold days can be paid.
Reserve bed days stop when:
▪ The resident enters a different long-term care facility (whether for skilled care, nursing care,
or ICF/ID care).
▪ The facility will not accept the client back from hospitalization due to care needs.
Payment for reserve bed days is at 42% of the facility’s rate. No worker entries are required to
stop or lower payments to a nursing facility for bed hold. Payments are adjusted based on claims
submitted by the facility.
Facilities use the Case Activity Report, to notify you if the resident is discharged, including reserve
bed information from the month of discharge. If reserve bed days run out before the person is
discharged, remaining days are noncovered days, and are not paid by Medicaid.
Use the information from the Case Activity Report to recalculate client participation between
facilities. When calculating the payment for reserved bed days, use the facility per diem listed on
the IoWANS My Reports screen.
Mr. N leaves a nursing facility and goes to the hospital August 10. He stays 15 days in the
hospital and is placed in skilled care. His total client participation is $1,500. The portion
computed for each facility is as follows:
NF Medicaid per diem is $90.00
42% of $90.00 = $37.80
$37.80 x 10 days = $378.00
$ 810.00
+ 378.00
$ 1,188.00
$90.00 x 9 resident days
$37.80 x 10 bed hold days
CP owed for nursing care
$ 1,500.00
- 1,188.00
$ 312.00
Total CP
CP paid for nursing care
CP owed for skilled care beginning August 20

Title 8: Medicaid Page 67
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Billing and Payment
Revised April 14, 2023 Payment for Reserve Bed Days
ICFs/ID
Legal reference: 441 IAC 82.14(4)“d,” “e,” and “f”
Payment will be made to reserve a bed in an ICF/ID as follows:
▪ For visits home, payment is made up to a maximum of 30 days annually.
Additional days may be approved for special programs of evaluation, treatment, or
habilitation outside the facility. A physician or qualified intellectual disability professional
must sign documentation indicating the appropriateness and therapeutic value of the
resident’s visits and programming days.
Visit days may be taken at any time. There is no restriction on the number of days taken in
any month or any visit as long as the maximum number is not exceeded.
▪ For hospitalization, payment is made up to a maximum of ten days in any calendar month.
Reserve bed days stop if the resident enters a different long-term care facility, whether for
skilled care, nursing care, or ICF/ID care.
An ICF/ID with 16 or more beds receives 80% of its actual per diem for reserve bed days. An
ICF/ID with 15 or less beds receives 95% of its actual per diem for reserve bed days. No worker
activity is required to correct reserve bed day payment.
When Reserve Bed Days Are Paid Privately
Legal reference: 441 IAC 81.10(5)“e”, 441 IAC 82.14(5)
The resident, family, or friends may choose to pay reserve bed days when the resident has
exhausted reserve bed days. If the resident is not discharged, the payment made by the resident
must be consistent with the Department payment. These days paid by family or friends are not
covered days for Medicaid.
If the facility plans to discharge a resident after Medicaid payment stops, the resident or the
family may make an arrangement to hold the bed when the resident is discharged. The facility
must follow normal discharge procedures (e.g., clothing and possession are returned to the
family, the personal needs account is closed and all resident records are closed), and send a Case
Activity Report to the local office.
No Supplementation of Payment Allowed
Legal reference: 441 IAC 80.3 (249A), 441 IAC 81.10(5), 441 IAC 82.14(5)
Only client participation can be billed to the member. The facility cannot require supplementation of a
Medicaid payment. The facility must accept reimbursement based on the Department’s methodology as
payment in full. There are two exceptions:
▪ The member, family, or friends may pay to hold a bed when the member is absent over the limit
for reserve bed days. See When Reserve Bed Days Are Paid Privately.

Title 8: Medicaid Page 68
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Billing and Payment
Revised April 14, 2023 No Supplementation of Payment Allowed
▪ Payment of the cost of care by the resident or resident’s family is not supplementation when it is
included in the calculation of client participation and does not exceed the payment made by the
state.
Use form 470-0373, Voluntary Contribution Agreement, to document a voluntary contribution so that all
parties are aware of the contribution and its effect on the Medicaid payment.
Voluntary contribution amounts should be entered on the BCW2 as “Other” income benefits only.
Payment for items that the facility does not have to provide, such as a telephone or cable television, is
not considered supplementation.
Payment for items or care required to be provided by the facility is supplementation. For example,
payment for a private room is supplementation, since the facility must provide a room. If such payment
is made, it must be included in the member’s client participation.
Payment for Inpatient Hospitals Who Require a Lower Level of Care
Legal reference: 441 IAC 78.3, 441 IAC 78.3(13) and (14), 441 IAC 81.10(4)“g”
When the IME Medical Services Unit or the MCO determine that a resident needs a lower level of
care, the facility’s social worker is responsible for finding alternative placement. When an alternative
placement cannot be found, and the facility and the Department agree to this, Medicaid payment may
continue.
When payment is to be made at a lower level of care, code ABC with the aid type, MED CP code, and
vendor number for the original level of care.
Payment for Transferring a Resident by Ambulance
Legal reference: 441 IAC 78.11(249A)
Payment for transporting a resident by ambulance will be approved if medically necessary and the
resident is:
▪ Transferred to the nearest hospital with appropriate facilities.
▪ Transferred to a hospital in the same locality.
▪ Transferred from one hospital to another.
▪ Transferred from a hospital to a nursing facility.
The Iowa Medicaid Enterprise or the MCO will deny a claim for ambulance transportation from a
medical institution to a hospital if the transportation was not medically necessary.
When a nursing facility resident is hospitalized and later discharged from the hospital, payment will be
made for the trip to the nursing care facility in which the recipient lives, even if it is not the nearest
nursing care facility.

Title 8: Medicaid Page 69
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Billing and Payment
Revised April 14, 2023 Payment for Transferring a Resident by Ambulance
If a resident needs to move to another facility because a facility is closing, the requirements regarding
medical necessity and distance do not apply. Nor do these requirements apply to a resident moving
from a nursing home to a residential care facility because the resident no longer required nursing care.
Billing and Payment for Hospice Members
Legal reference: 441 IAC 78.36(3)
Before providing hospice service to a Medicaid member in a nursing facility, the hospice agency must
notify the member’s IM worker that the member has chosen to receive hospice services, and to verify
the amount of client participation. Determine eligibility and client participation as for other nursing
facility member.
When a hospice member enters a nursing facility, the hospice is responsible for paying for the nursing
facility care. Medicaid will pay the hospice for the care, and the hospice reimburses the nursing facility.
The hospice collects client participation, unless the hospice and nursing facility jointly agree that the
nursing facility will collect the client participation.
The hospice is responsible for obtaining the signature of the member or the member’s representative
on form 470-2618, Election of Medicaid Hospice Benefit, or a similar form as defined in the hospice
provider manual.
The hospice is also responsible for entering into a written agreement with the nursing facility under
which the hospice program takes responsibility for the professional management of the member’s
hospice care and the facility agrees to provide room and board to the member.
Use of IoWANS
IoWANS is the Iowa Department of Human Services’ Institutional and Waiver Authorization and Narrative
System. IoWANS (previously Individualized Services Information System (ISIS)) started supporting the facility
programs in October of 2004. The purpose of IoWANS is to assist workers in both processing and tracking
requests starting with entry from the ABC system through approval or denial.
Upon application, the consumer will be tracked through the eligibility determination process. Once the
application is approved, IoWANS will provide the Iowa Medicaid Enterprise or the MCO with information
and authority to make payments to or on behalf of a member. The member is tracked in IoWANS until that
member is no longer accessing a facility or waiver program.
A case normally starts with the income maintenance (IM) worker entering information into the ABC system.
Pertinent information is then passed to IoWANS. IoWANS identifies key tasks (called “milestones”) for the
IM worker and for other entities involved to complete approval of the member. The milestones form a
workflow, taking a request for facility payment to denial or final approval.
For details on IoWANS work flows for facilities and on using IoWANS, see 14-M, IoWANS User Guide.

Title 8: Medicaid Page 70
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Use of IoWANS
Revised April 14, 2023 Important Facts About IoWANS for Facility Programs
Different IoWANS work flows (sequences of key tasks presented on milestone screens) have been
established for medical facility enrollment processes:
▪ NF, skilled, PMIC, MHI, and hospice
▪ ICF/ID
Important Facts About IoWANS for Facility Programs
While 14-M, IoWANS User Guide is a rich source of information about IoWANS, some of the important
facts from that guide are repeated here for emphasis and convenience:
▪ IoWANS milestone screens present a question, instruction, or statement followed by choices for a
response on two to five response buttons. Reaching a choice may take activity outside of
IoWANS. Remember that while IoWANS tends to speed the process, it does not replace all the
work that must be done, such as collection of verification.
▪ All milestones in the process of approving a facility case must be completed before the Iowa
Medicaid Enterprise or the MCO can be authorized to start making payments.
▪ If you receive an IoWANS milestone and do not immediately know how to respond, clicking on
the CANCEL button will leave the milestone task on the workload page so it can be postponed for
a later response. You will be able to access the milestone screen again whenever you are ready to
respond.
▪ If the person responsible for a milestone responds prematurely with insufficient or erroneous
information, it may be possible to “undo” the milestone.
To see if that is possible, navigate to the STATUS screen for the member by clicking on the
STATUS subtab while the member is selected. If it is possible to undo the milestone, a TRASH
CAN icon will be present in the last column of the milestone’s record.
If the “undo” is not permitted because “downstream” milestones have been accomplished, it will
be necessary to contact people who have performed the downstream milestones to arrange for a
series of “undo” actions or to contact the IoWANS Facilities Help Desk for assistance.
▪ The LOC (level of care) and LOC EFFECTIVE DATE fields (on the PROGRAM REQUEST screen) will
be blank or show “unknown” when the pending application is first passed to IoWANS. During the
workflow process, an LOC milestone is generated. Once the level of care is formally entered, the
program request will display the correct level of care and the effective date.
▪ When entries are completed in the ABC system to move a consumer to a different facility,
IoWANS will start a new program request. All of the workflow associated to a new member must
be repeated before for the new facility can receive payment.
▪ IoWANS provides a screen that displays the current program request. This screen will eventually
show three years of program request history. Information for programs older than three years will
be archived. Reports will be available through the SPIRS Help Desk.
A request for facility payment is processed through the IoWANS workflow that ends with the
milestone for the IM worker to give final approval. When you give a positive response to this
milestone, it will authorize the IME or the MCO to make payments to the provider.

Title 8: Medicaid Page 71
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Use of IoWANS
Revised April 14, 2023 Important Facts About IoWANS for Facility Programs
IMPORTANT: Make sure that all actions necessary to establish eligibility, including those outside of
IoWANS are complete and accurate before you respond to the final milestone and enter the approval
on ABC.
Once the program request is authorized and a beginning date is passed from ABC, a facility provider
can view the member’s client participation amount using Iowa Medicaid Provider Access (IMPA).
For enrollment process details, see 14-M, IoWANS User Guide.
Facility Administrative Information
This section contains a brief overview of selected facility responsibilities. The facility provider manuals explain
more fully all the responsibilities of facilities that participate in the Medicaid program. Included in this section
are procedures relating to:
▪ Reporting changes in a resident’s status
▪ Transfers and discharges
▪ How personal needs accounts are handled
▪ What happens when a facility closes
▪ What happens when ownership of a facility changes
Reporting Changes in a Resident’s Status
Legal reference: 441 IAC 81.5(2), 441 IAC 82.10(2), 441 IAC 85.6(2), 441 IAC 85.24 (2), 441 IAC
85.45(2)
Medical institutions, except hospitals, are required to send the Case Activity Report to the office
responsible for the placement when a Medicaid applicant or member:
▪ Enters the facility.
▪ Dies or is discharged.
▪ Is covered by Medicare for skilled level of care.
▪ Is no longer covered by Medicare for skilled level of care.
Transfers and Discharges
Legal reference: 441 IAC 81.5(1), 441 IAC 81.13(6)“a,” 441 IAC 82.10(1),
The facility is not allowed to transfer or discharge the resident unless:
▪ A transfer or discharge is necessary for the resident’s welfare and the resident’s needs cannot be
met in the facility.
▪ The resident’s health improves so that the resident no longer needs the facility’s services.
▪ The safety of other residents in the facility is endangered.

Title 8: Medicaid Page 72
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Facility Administrative Information
Revised April 14, 2023 Transfers and Discharges
▪ The health of other residents in the facility would be endangered.
▪ The resident has failed, after reasonable and appropriate notice, to pay for stay at the facility. If the
resident became eligible for Medicaid after admission, the facility may charge only for those items
allowed by Medicaid.
▪ The facility ceases operation.
If a facility plans to discharge a resident, facility staff must provide advance written notice and explain
appeal rights. The facility must also send you form 470-0042, Case Activity Report, when the discharge is
made.
A resident may be transferred or discharged from a facility upon the request of the resident or the
resident’s family, guardian or physician. The facility’s social worker may help the resident by:
▪ Planning the move.
▪ Referring the resident to other resources for help.
▪ Coordinating the services of public health nursing, homemaker services and other agencies, and
work with the resident’s family.
▪ Performing follow-up visits.
▪ Involving family and friends in decision-making, planning, and the work of transfer or discharge.
Resident Trust Account
Legal reference: 441 IAC 81.4(3), 441 IAC 81.13(5)“c”, 441 IAC 82.9(3)
As described in Ongoing Personal Needs Allowance, residents may keep a portion of their monthly
income for personal needs, to spend as the resident wishes. Resident trust accounts are set up by the
facility to manage the personal needs funds for residents.
If the resident dies, the facility must release the balance in the account to the resident’s guardian or
next of kin to pay funeral expenses. The facility must get a receipt when it releases funds.
If there are no relatives, funds in the account revert to the Department. The facility should turn the
funds over to the Centralized Facility Eligibility Unit (CFEU). Forward the funds to the Department’s
Bureau of Accounting Services. If an estate is opened, the Department will turn the funds over to the
estate. The estate is responsible for paying claims to the Department under the estate recovery
program.
If a Facility Closes
Legal reference: 441 IAC 81.12(249A), 441 IAC 82.16(249A)
If a facility plans to close, facility staff must notify the Department 60 days in advance. (In an emergency,
this time may be shortened.) If the contract between the Department and a facility is terminated, the
local office must help residents who wish to transfer to a certified facility.

Title 8: Medicaid Page 73
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Facility Administrative Information
Revised April 14, 2023 If a Facility Closes
If the Department terminates the Medicaid contract with a facility, the Iowa Medicaid Enterprise (IME)
sends a notice of cancellation to the facility by certified mail. Copies are sent to the local office, the
service area manager or the MCO, the Division of Fiscal Management, and the Department of
Inspection and Appeals.
Local office staff and the administrator of the facility must immediately notify the residents and their
families of the closing, then plan for an orderly transfer of residents. Alternative placements must be
investigated. The facility may make transfer plans independently with the residents and their families.
In certain cases the federal government will continue participation of Medicaid funds for residents of
facilities that have lost certification. The extension cannot exceed 30 days beyond the date of contract
cancellation, and is allowed only to cover the time necessary to ensure the orderly transfer of
residents.
If a resident is transported by ambulance due to a facility closing, contact the Bureau of Medical and
Long Term Services and Supports before the date of service with the following information:
▪ Name and case number of resident to be transferred.
▪ Date of transfer.
▪ The vendor used in the transfer.
▪ The facility from which the resident is being moved and the facility to which the resident is being
moved.
This information is used to process the claim and authorize the Iowa Medicaid Enterprise to make
payment.
If Facility Ownership Changes
If ownership of a facility changes, the facility is given a different provider number for the new owner.
Payments will not be made until the provider number is changed from the old owner’s number to the
new owner’s number. This change occurs in IoWANS through the following steps:
1. DIA notifies the IME Provider Services Unit of the ownership change.
2. The new facility owner submits an enrollment application to IME Provider Services Unit.
3. The IME Provider Services Unit:
▪ Issues the facility a new provider number.
▪ Enters the number into MMIS.
▪ Verifies the reimbursement rate for the old provider number in MMIS.
▪ Verifies that the new provider number is active in MMIS.
▪ Sends a memo to IME Data Warehouse to initiate the automatic change in IoWANS.
▪ Sends a letter to inform the facility of the change, with copies to DIA Health Facilities and
Audits, the IM supervisor, and other IME units.
4. The IME Data Warehouse implements the “change of ownership” (CHOW) process for all
members who are identified as receiving services from the old provider. Any member whose
record has an open program request with the old provider number or has been closed with an

Title 8: Medicaid Page 74
Iowa Department of Health and Human Services Employees’ Manual
Chapter I: Medical Institutions Facility Administrative Information
Revised April 14, 2023 If Facility Ownership Changes
end date that is later than the effective date of the new provider number will be processed as follows:
▪ The program request is ended for the old provider on the date the new provider number is
effective.
▪ A new program request is started for the same date with the new provider number.
▪ The aid type, level of care, assessment date, county of residence, county of responsibility,
program, case number, and “app date” fields on the newly created program request are the
same as the program request that was closed.
▪ The change of ownership reason code of 077 will show on the new program request on
IoWANS.
5. Review the program request to ensure that the change was processed correctly. If the change is
effective the first day of the month, the approval is set. If the change is any day other than the first,
you will receive a workflow notification that the change has been made in IoWANS, and you must
respond to the workflow to set the approval.
Check the calculation of client participation. If there were bed hold or hospital days, the CP 1ST
MONTH entry should be lower and you need to send a request to DHS, SPIRS to correct this.
Check the calculation of the CP 1ST MONTH entry as follows:
▪ Determine the reimbursement rate of the facility in which the member lived during the first
part of the month.
▪ Multiply that rate by the number of days in the facility. This is the amount to be applied to the
last partial month at the old vendor number, before the change of ownership. Do not include
the last day, because Medicaid does not pay for that day. The last day will be paid under the
new provider number.
▪ Subtract this amount from the member’s previously calculated total client participation (found
in the CP ONGOING field on the program request that is being closed).
▪ The remainder is to be applied to the new vendor number for the remaining days in the
month and should be entered in the CP 1ST MONTH field.
The CP ONGOING entry should be the same as in the previous program request.
Any subsequent program requests with this same provider number must also have the provider
number changed. If there are subsequent program request with a different provider number, you
must process the ownership change manually.
6. You will also be notified through IoWANS workflow to make ABC entries on the TD05 screen to
change to the new provider number and effective date. If you don’t make the correct entries on
TD05, this could cause errors or an incorrect vendor number to be passed with the next ABC
activity.
7. Once approval is set on the new program request, the provider can submit claims to IME CORE
using the new provider number. The provider will need to check Iowa Medicaid Provider Access
(IMPA) to determine if the approval to the new provider number has been completed.
