
Primary Care Expenditures
Summary of current primary care expenditures
and investment in Washington
Report to the Legislature
As required by Chapter 415, Laws of 2019
Forecasting and Research
Office of Financial Management
December 2019
Contents
Executive summary ............................................................................................. 1
Background ......................................................................................................... 2
Approach to estimate primary care spending ....................................................... 3
Results ................................................................................................................ 7
Previous research on primary care .................................................................... 11
Non-claims-based expenditures ........................................................................ 12
Limitations of current report ............................................................................... 16
Future considerations ........................................................................................ 18
Conclusion ........................................................................................................ 18
References ........................................................................................................ 20
Appendix A: Budget proviso .............................................................................. 22
Appendix B: Primary Care Expenditures Stakeholder Group ............................. 23
Appendix C: List of providers ............................................................................. 24
Appendix D: Procedure codes ........................................................................... 27

Primary Care Expenditures Report 1
Executive summary
This is the first comprehensive analysis of annual primary care medical expenditures in Washington.
In the 2019–21 biennial budget, the Legislature directed the Office of Financial Management to
determine annual primary care medical expenditures as a percentage of total medical expenditures by
carrier. This report summarizes the approach and data sets used to calculate these expenditures,
compares and contrasts the methods and results with other state and national reports on primary
care medical expenditures, and discusses limitations to current data sources.
OFM, working with key stakeholders representing different areas of primary care practitioners,
created a definition for primary care providers and services that takes into account the range of
interpretations of primary care. A narrow and broad definition of providers and services were
created, and then claims meeting the service and provider definitions were used to calculate primary
care expenditures. This approach ensured expenditures attributed to primary care services were
incurred by primary care providers. Expenditures were calculated using cost information from the
Washington All-Payer Health Care Claims Database.
In Washington for 2018, primary care expenditures as a percentage of total medical
expenditures ranged from 4.4% (about $838 million) to 5.6% (about $1 billion) based on
either a narrow or broad definition, respectively, of primary care. Primary care spending
as a percentage of total spending was highest for people under 18 years and lowest in
people 65 years and older.
With respect to market sector: Similar percentages of primary care spending were seen in public
employee, Medicaid managed care and commercial coverage. Medicare Advantage had the lowest
percentage, reflecting differences already seen by age. Differences in primary care spending by
health care company and market sector vary considerably and could be influenced by the needs of
the population covered (average age, sex, comorbidity and geography).
This report’s estimates for the proportion of medical expenditures attributable to primary care
appears smaller than estimates calculated in other reports. Because there is no national standard for
how to measure primary care expenditures, however, these estimates cannot be compared directly
because of differences in data sets, methodologies and definitions of primary care. When comparing
Washington’s proportion of primary care spending with reports from Oregon and Rhode Island, the
differences in approaches and definitions of primary care make these types of comparisons
challenging. For instance, Washington included pharmacy claims in its total medical expenditures
while Oregon did not. Washington and Oregon also differed in their methods for capturing costs of
primary care services. Oregon and Rhode Island included non-claims-based expenditures in their
total primary care spending which are not included in Washington’s estimates. An overview of the
non-claims-based expenditures collected by Oregon and Rhode Island is included in this report, in
addition to examples for future consideration in data collection efforts for Washington.
This report highlights a low rate of investment in primary care in Washington and, as a baseline, can
be used to monitor future spending. Research has shown health care systems with higher
proportions of investments oriented toward primary care have better health outcomes and lower
costs. Monitoring the impact of policies and system performance will be key to successfully
strengthening Washington’s primary care system.

Primary Care Expenditures Report 2
Background
In the 2019–21 biennial operating budget, Chapter 415, Laws of 2019,
1
the Legislature directed the
Office of Financial Management to conduct a study to determine annual primary care medical
expenditures as a percentage of total medical expenditures in Washington (Appendix A). Having an
estimate of primary care expenditures, in addition to reports on the primary care workforce,
enhances the state’s understanding of the current level of investment in primary care (Yen, 2018).
With a baseline of primary care spending, the state will have better:
• Benchmarking of spending and investments on primary care;
• Tracking of efforts to increase primary care spending;
• Measurement of the impacts of payment reform;
• Focus of interventions to increase patient access to primary care; and
• Information to compare to other states’ efforts to increase primary care spending.
Similar reports have been completed in Oregon and Rhode Island; efforts are underway in other
states to understand primary care spending levels to guide new investments.
As required in the proviso, OFM convened a group of stakeholders (Appendix B) representing
family practice, general internal medicine, general pediatrics and the state Health Care Authority to
advise on the parameters for estimating primary care expenditures for the state.
The stakeholder group worked with OFM to answer the following questions:
• Who are primary care providers?
• What are primary care services?
• What percentage of total health care expenditures is currently allocated to primary care?
• How does this percentage differ by health insurance carrier?
• What information about primary care is not captured by current data sources?
OFM also contacted researchers in Oregon and Rhode Island, and from other institutions who
worked on similar primary care expenditure reports, to discuss methodology and gather advice for
pursuing the Washington report.
The goals for Washington’s primary care expenditure report are to:
• Conduct a transparent process for determining what providers and services are
considered primary care;
• Develop a transparent and detailed methodology that can be replicated to measure
trends and changes in primary care spending in future years;
• Discuss differences between Washington’s methodology and results compared with
other estimates and reports;
• Identify barriers to accurately estimating primary care expenditures; and
• Provide suggestions and guidance for future tracking of primary care spending and
iterations of this type of report.
OFM intends for this report to be the baseline for tracking and monitoring new investments and
initiatives to increase primary care spending in Washington. This report can help frame discussions
1
http://lawfilesext.leg.wa.gov/biennium/2019-20/Pdf/Bills/Session%20Laws/House/1109-S.SL.pdf
Primary Care Expenditures Report 3
on what additional information will be beneficial for understanding primary care needs and how to
measure outcomes of increasing primary care spending.
But first, we must start with a definition of primary care.
What is primary care?
Primary care as defined by the National Academy of Medicine (formerly the Institute of Medicine):
“… is the provision of integrated, accessible health care services by clinicians who are accountable
for addressing a large majority of personal health care needs including physical, mental, emotional,
and social concerns, developing a sustained partnership with patients, and practicing in the context
of family and community (Donaldson, M.S., Yordy, K.D., Lohr, K.N., & Vanselow, N.A., 1996).”
This definition has been used to measure how well four main features of primary care services are
fulfilled (Starfield, B., Shi, L., Macinko, J., 2005):
• First-contact access (into the health care system) for each new need
• Long-term person- (not disease-) focused care (also referred to as continuous care)
• Comprehensive care for most health needs
• Coordinated care when it must be sought elsewhere
Investing in primary care and ensuring access to primary care can reduce health care costs by
lowering rates of preventable emergency department visits, hospital admissions and specialist visits
(Friedberg, Hussey, & Schneider, 2010; Glass, Kanter, Jacobsen, & Minardi, 2017; Starfield, B.,
Shi, L., Macinko, J., 2005). Primary care helps to achieve health equity by providing access to health
services and promotes care at the most appropriate level (Starfield, 1998) and, as a result, can reduce
premature mortality (Basu et al., 2019; Starfield, B., Shi, L., Macinko, J., 2005). Internationally, health
systems with higher proportions of health care spending on primary care have better health
outcomes and lower health care costs (Friedberg et al., 2010; Jabbarpour, Y., Greiner, A., Jetty, A.,
Coffman, M., Jose, C., Petterson, S., 2019; OECD, 2017).
Many states are implementing strategies to improve primary care investment by adopting patient-
centered medical home incentives or other value-based care models; focusing on social determinants
of health; expanding the primary care workforce and infrastructure; or increasing rates for primary
care providers.
Approach to estimate primary care spending
OFM contracted with Onpoint Health Data to estimate primary care expenditures using the state-
run Washington All-Payer Health Care Claims Database, or WA-APCD. Onpoint Health Data is the
data vendor for the WA-APCD, which was established by OFM through legislation passed in 2014.
Launched in the summer of 2018, the WA-APCD contains pharmacy, medical and dental claims
along with eligibility information. It is the most comprehensive source of claims data in the state
with more than 6 million covered lives from more than 50 commercial, Medicaid and Medicare
payers. Self-insured (not covered by state public employee benefits), federal insurance and Veterans
Benefits Administration claims are not included in the database. The WA-APCD contains cost
information, including billed, allowed and paid amounts that allow for calculations of total and
primary care expenditures. Data from 2014 through the third quarter of 2019 are included in the
database; submissions from carriers are completed on a quarterly basis and validated on a yearly
basis. Data from calendar year 2018 were used for this report.
Primary Care Expenditures Report 4
Inclusion and exclusion criteria
As per the budget proviso, total medical expenditures excluded dental care, but included costs of
prescription drugs. The proviso also called for vision care to be excluded, but it was unclear what
types of vision services should be excluded (e.g., eyeglasses, cataract surgery, glaucoma testing).
Many commercial insurance plans lack vision coverage, but because vision services are not
submitted separately from medical claims to the WA-APCD (unlike dental claims that are a separate
submission), it was determined for this report to leave vision services as part of total medical
expenditures.
Only claims paid using the member’s primary insurance are included in the calculations for
expenditures. Claims paid using a secondary insurance or payer were not included to avoid double
counting expenditures. Only members who had a medical or pharmacy claim paid in 2018 are
included in the analysis, limiting the members who are included. According to the National Health
Interview Survey, about 16% of adults did not have contact with a doctor or other health care
professional in the past year (Centers for Disease Control and Prevention, 2019).
Additionally, Medicare fee-for-service data were excluded from this report because the 2018 data
will not be available until 2020. Medicaid fee-for-service data were excluded due to errors in
submission to the WA-APCD, and health care claims from Coordinated Care for Medicaid managed
care were excluded because labeling of its claims in the submission process made it difficult to
distinguish if claims were paid as a primary or secondary payer.
Oregon and Rhode Island included estimates of non-claims-based expenditures for primary care,
which are usually self-reported by the individual insurance carriers in the state, in their reports on
primary care spending. Currently, there is no process in Washington to collect this type of
information from all commercial carriers. The Health Care Authority collects information from the
Medicaid managed care organizations and the public employee benefits carriers for managed care
rate development, and is developing processes to collect non-claims information for future
contracts. OFM was unable to access this information for this report. Suggestions for future data
collection of non-claims-based expenditures are outlined later in this report.
Defining primary care claims
Identifying primary care services in claims data is not straightforward. Most analyses of primary care
expenditures using claims data must construct a definition for primary care provider and primary
care services. There are several reasons for this approach:
• Identifying primary care clinics or offices in claims data is difficult because there is no field
or value that indicates primary care as a setting of care.
• Providers who list primary care as their specialty may work in a variety of places, some of
which would not be considered a traditional primary care setting (e.g., hospitalists in in-
patient settings or nurse practitioners working in a specialist’s office) or may be delivering
nonprimary care services.
• Some primary care services may be delivered by specialists or others who would not be
defined as a primary care provider (e.g., a cardiologist ordering a basic lab test).
• Some institutions (e.g., Federally Qualified Health Center) may submit both a facility and
professional claim for primary care services depending on the health insurance company,
and the provider identification on these types of claims may be different.
Primary Care Expenditures Report 5
As a first step for this analysis, separate definitions of primary care provider and primary care
services were determined and then claims meeting both definitions were included as primary care
expenditures. This approach follows the concepts of the Primary Care Spend Model to narrow
primary care services to those that are performed specifically by primary care providers (Baillieu et
al., 2019).
Primary care providers
Washington does not have a roster or other data source identifying individual providers who are
practicing in primary care settings. Some health insurance companies may have a listing of providers
delivering primary care, but it is not included in claims submissions to the WA-APCD. There is also
no agreed-upon definition used in the literature to define primary care providers. Some of the
variation in definition is due to the availability of different data sources that may or may not include
certain types of providers (e.g., homeopaths).
The stakeholder group began by reviewing taxonomy codes, which are used to categorize health care
providers by their specialization, and descriptions included in the 2019 Primary Care Spending in
Oregon report (Oregon Health Authority and the Department of Consumer and Business Services,
2019). The stakeholder group decided upon two groups of providers (Appendix C):
• Narrow definition: representing providers who traditionally perform roles contained within
strict definitions of primary care
• Broad definition: representing providers who perform roles not traditionally contained
within a strict definition of primary care (e.g., obstetricians)
This approach is similar to other reports on primary care expenditures (Bailit, Friedberg, & Houy,
2017; Jabbarpour, Y., Greiner, A., Jetty, A., Coffman, M., Jose, C., Petterson, S., et al., 2019; Reid,
Damberg, & Friedberg, 2019), but was not the approach taken in the Oregon report. Results for
both the narrow and broad definitions of primary care providers are included in this report.
Taxonomy codes for the narrow definition of primary care provider are family medicine, internal
medicine, Federally Qualified Health Center, general practice, naturopath, pediatrics, preventive
medicine, nurse practitioner, physician assistant, primary care clinic and rural health clinic. The
broad definition of providers included behavioral health providers, clinical nurse specialist,
registered nurse, midwives, obstetrics and gynecology, family medicine and pediatric subspecialties,
homeopath, psychiatry and neurology, psychologist, registered nurse and social worker.
Primary care services
Primary care procedures or services were defined using the American Medical Association’s Current
Procedure Terminology, or CPT, and the Healthcare Common Procedure Coding System, or
HCPCS. For this report, the stakeholder group began by reviewing the list of primary care
procedure codes included in the Oregon report and added services (e.g., additional preventive
medicine screenings) based on various works stakeholders had completed in other areas. Both a
narrow and broad list of services were considered for estimating primary care. Many of the services
included in the broad definition reflected services that were specific to provider taxonomies included
in the broad definition of primary care provider (e.g., obstetricians and care following a cesarean
delivery). Inpatient visits billed by primary care providers using a CPT or HCPC inpatient code were
not included in either the broad or narrow definition of primary care services. The stakeholder
group did not feel that these types of visits represented traditional primary care (e.g., first-contact
access, continuous, comprehensive, coordinated) or getting people the right care in the right setting.
In many instances, it’s difficult to identify which services on claims were performed by a primary
Primary Care Expenditures Report 6
care provider in inpatient hospital settings. Emergency department visits billed by a primary care
practitioner were also not included for similar reasons.
Other reports on primary care expenditures have used one definition for primary care services cross-
walked with different definitions for primary care providers (Bailit et al., 2017; Jabbarpour, Y.,
Greiner, A., Jetty, A., Coffman, M., Jose, C., Petterson, S., 2019). Reid et al (Reid et al., 2019) used
both a narrow and broad definition for primary care providers in combination with a narrow
definition for primary care services and then again with all professional services.
This report contains the results from both the narrow and broad definition of primary care services.
Examples of primary care procedure codes are those for routine medical exams, preventive medicine
services, screening for diseases, vaccine administration and newborn care services (Appendix D).
Expenditure calculations
Expenditures for health care services were calculated using the total allowed amount submitted on
claims to the WA-APCD. The total allowed amount includes the health insurance plan paid amount
plus any deductibles, coinsurance or copays paid by the patient. For insurance companies that pay
providers using capitated payment arrangements (e.g., a per-member per-month payment), the fee-
for-service equivalent amount is submitted to the WA-APCD and used as the paid amount for that
health care service.
Total health care expenditures comprised all medical claims (including in-patient hospitalizations)
and pharmacy claims. With respect to immunizations: Although vaccines are included in the total
health care expenditures calculations, only the costs associated with administering the vaccine, if
administered by a primary care provider, were included in primary care expenditures. Expenditures
for primary care services provided by primary care providers were aggregated by provider specialty
and then summed across all provider groupings to estimate total primary care expenditures.
Although Appendix C (List of Providers) lists a large number of behavioral health specialist
taxonomy codes, when primary care service codes were applied, most claims and associated
expenditures for these providers were not included in primary care expenditures.
All nurse practitioner and physician assistant taxonomy codes were included in this report.
Adjustments were made to the total primary care expenditures calculated for these providers. These
adjustments (41% for nurse practitioners and 34% for physician assistants) were needed because
many nurse practitioners and physician assistants may have a provider taxonomy code included in
the definition for a primary care provider, but actually provide care in other settings (e.g., surgical).
Because claims data do not indicate if a health care setting is primary care, the adjustment factors
were needed to avoid overestimating primary care expenditures by counting services for nurse
practitioners or physician assistants that were not conducted in primary care settings. These
adjustments were based on recommendations from the stakeholder group and studies conducted by
the Washington State University College of Nursing (Kaplan & Gill, 2018) and the Washington
Medical Commission (Washington Medical Commission, 2019).
Primary care services for people without insurance and services paid with cash by patients who did
not file an insurance claim were not included in the analyses.
Calculations for carriers
More than 50 commercial, Medicare and Medicaid data suppliers submit claims data to the WA-
APCD. Data are submitted either at the company level or at the individual health insurance plan
level, depending upon how the company’s claims processing system is set up and the number of

Primary Care Expenditures Report 7
health insurance plans issued in the state. Plans were first grouped by market sector (commercial,
public employee benefits, Medicaid managed care organizations and Medicare Advantage) and then
rolled up to the company level. Primary care and total expenditures were calculated at the company
level within each market sector. Companies that had fewer than 1,000 covered persons were
excluded from analyses. Dental companies were also excluded, and only medical and pharmacy
claims from 2018 were used.
Results
Monthly enrollment
Included in this report is claims information for more than 1.2 million Medicaid managed care
organization members, more than 1.1 million commercial members, and more than 300,000 public
employees and 300,000 Medicare Advantage members. The total amount of health care spending
captured in the WA-APCD for this report for 2018 was almost $19 billion, 21% of which was for
pharmacy claims.
In 2018, overall investments in primary care as a total of all medical expenditures for Washington
ranged from 4.4% to 5.6%, depending on whether a narrow or broad definition of providers and
services were used (Figure 1). Limiting the definition of primary care providers and procedures to
narrow definitions each resulted in approximately $838 million in claims. Including the broad
category of procedures resulted in about $50 million more and an increase in the primary care share
to 4.7% of total medical expenditures. Including a broad definition of providers, in addition to a
broad definition of procedures, increased primary care expenditures by about $169 million and
resulted in a 19% increase in primary care expenditures, but overall, the total percentage of all health
care expenditures specific to primary care was only 5.6%.
Figure 1. Summary of Medical Expenditures in Washington State, 2018
Pharmacy
$3,862M
(20.5%)
Other Medical
$13,955M
(73.9%)
Broad Provider &
Broad Procedure
$169M (0.9%)
Narrow Provider &
Broad Procedure
$50M (0.3%)
Narrow Provider &
Narrow Procedure
$838M (4.4%)
Primary Care
(5.6%)

Primary Care Expenditures Report 8
This highest percentage of primary care spending was for individuals younger than 18 years, ranging
from 10.4% to 11.2% of about $2 billion in total medical expenditures for the narrow (narrow
definition of providers and narrow definition of procedures) and broad (broad definition of
providers and broad definition of procedures) definitions of primary care, respectively (Figure 2). Of
working age adults aged 18 to 64 years, the percentage of primary care spending ranged from 3.8%
to 5.4% of about $11 billion in total medical expenditures. It should be noted that this age group
could be affected the most by the inclusion of obstetrics in the broad definition of primary care. For
adults aged 65 and older, primary care spending was 3.5% to 4% of about $5.5 billion in total
medical spending. Older adults have a higher rate of hospital inpatient stays and other costs outside
of primary care because of the higher prevalence of chronic and comorbid conditions and greater
use of specialists.
Figure 2. Primary Care as Percentage of Total Expenditures by Age
4.4% 5.6%
10.4% 11.2%
3.8% 5.4%
3.5% 4.0%
Statewide
Age < 18
Age 18-64
Age >= 65
% PC narrow
% PC broad

Primary Care Expenditures Report 9
Considering primary care expenditures by market sector, public employee coverage had the highest
percentage of primary care spending, ranging from 5.8% to 7.3% of about $1.8 billion in 2018
(Figure 3). Medicaid managed care organizations ranged between 5.1% to 6.8% of about $4 billion in
2018; commercial plans ranged between 4.5% and 5.7% of about $8 billion; and Medicare
Advantage plans ranged from 3.4% to 3.9% of about $5 billion in total claims. Some of these
differences in primary care spending reflect differences in patient characteristics between market
sectors. Additionally, primary care spending for public employee coverage may be overestimated
because many of the pharmacy claims were not designated for public employees when submitted to
the WA-APCD. This would result in lower total expenditures for this group.
Figure 3. Primary Care as Percentage of Total Expenditures by Market Sector
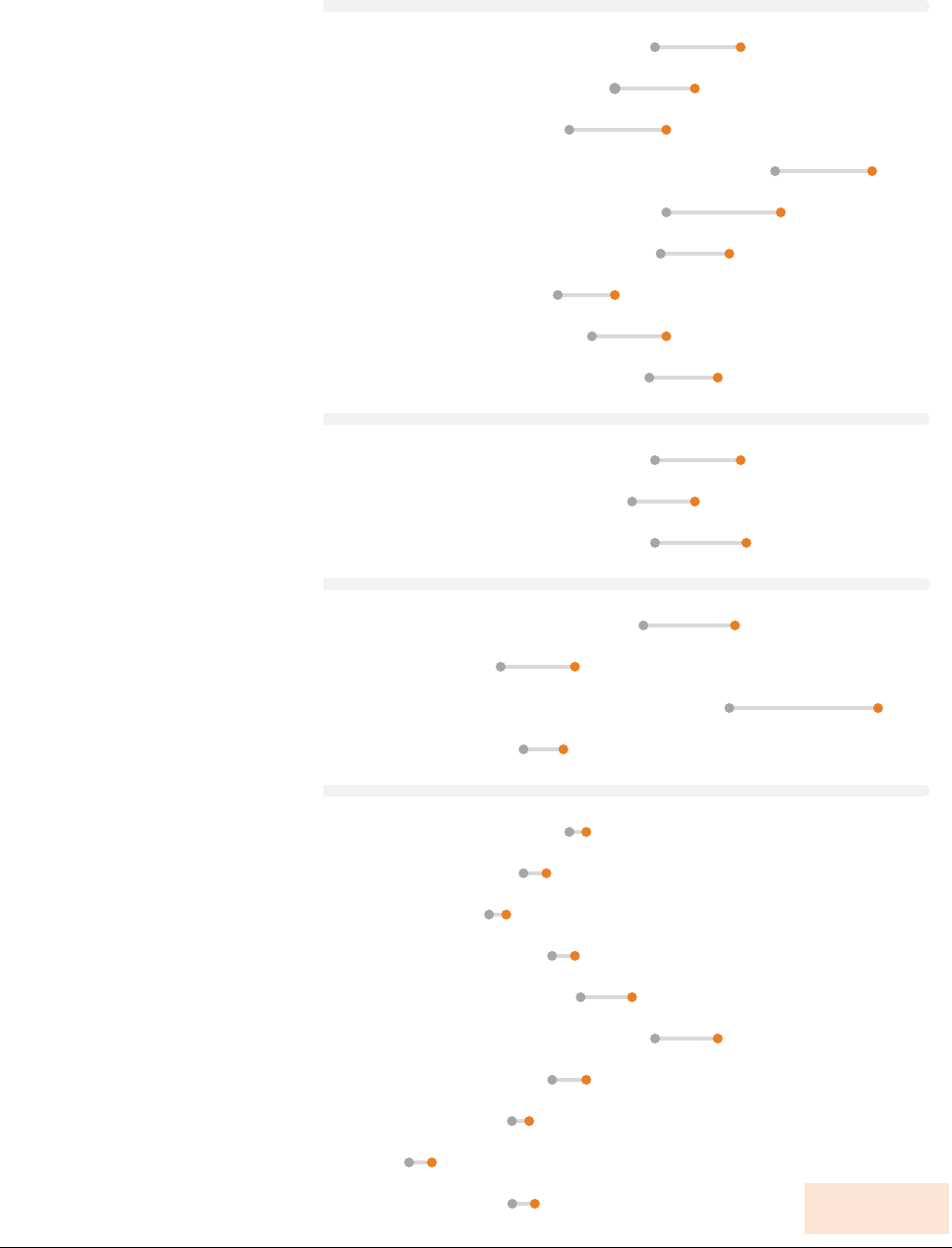
Of commercial plans, the percentage of primary care investment as a total of all medical
expenditures ranged from 4.1% to 5.1% for Premera Blue Cross to 7.9% to 9.6% for Kaiser
Foundation Health Plan of the Northwest. For public employee plans in the Public Employee
Benefits Board program, the range of primary care spending was very similar among the three
companies. For Medicaid managed care plans, the percentage of primary care spending as a total of
all medical expenditures ranged from 3.1% to 4.4% for Community Health Plan of Washington to
7.1% to 9.7% for Molina Healthcare. For Medicare Advantage plans, the percentage of primary care
investment was less than 7% for all plans (Figure 4). Even within market sector, caution should be
exercised in comparing expenditures by health plan or company because of differences in
characteristics of enrollees that are not adjusted for in these analyses.
4.5% 5.7%
5.8% 7.3%
5.1% 6.8%
3.4% 3.9%
Commercial
PEBB
Medicaid managed care
Medicare Advantage
% PC narrow
% PC broad
Primary Care Expenditures Report 10
5.8% 7.3%
5.1% 6.5%
4.3% 6.0%
7.9% 9.6%
6.0% 8.0%
5.9% 7.1%
4.1% 5.1%
4.7% 6.0%
5.7% 6.9%
5.8% 7.3%
5.4% 6.5%
5.8% 7.4%
5.6% 7.2%
3.1% 4.4%
7.1% 9.7%
3.5% 4.2%
4.3% 4.6%
3.5% 3.9%
2.9% 3.2%
4.0% 4.4%
4.5% 5.4%
5.8% 6.9%
4.0% 4.6%
3.3% 3.6%
1.5% 1.9%
3.3% 3.7%
COMMERCIAL*
Aetna Life Insurance Co.
Cambia Health Solutions
Cigna
Kaiser Foundation Health Plan of the NW
Kaiser Foundation Health Plan of WA
Molina Healthcare
Premera Blue Cross
Providence Health Plan
UnitedHealthcare
PEBB
Cambia Health Solutions
Kaiser Foundation Health Plan of NW
Kaiser Foudation Health Plan of WA
MEDICAID MANAGED CARE ORGANIZATIONS*
Amerigroup Washington, Inc.
Community Health Plan of WA
Molina Healthcare
United Health Care
MEDICARE ADVANTAGE
Aetna Life Insurance Co.
Cambia Health Solutions
Community Health Plan of WA
Humana
Kaiser Foundation Health Plan of the NW
Kaiser Foundation Health Plan of WA
Molina Healthcare
Providence Health Plan
Soundpath Health
UnitedHealthcare
Figure 4. Primary Care as Percentage of Total Expenditures by Carrier or Company
% PC narrow
% PC broad
* Data for Coordinated Care are not listed due to data issues.
Primary Care Expenditures Report 11
Previous research on primary care
There have been a number of efforts to estimate primary care spending as a proportion of total
health care spending. While Washington’s estimates might appear low, these estimates cannot be
compared directly with other published studies. Indeed, there is no national standard for how to
measure primary care expenditures. As a result, estimates between reports may differ as a result of
different definitions of primary care, different data sets used in analyses, different populations
included in data sets and different methodologies to estimate primary care spending.
The Robert Graham Center, using survey data from the Medical Expenditure Panel Survey, or
MEPS, estimated that Washington spends between 5.9% and 10.1% of health care expenditures on
primary care (depending on whether a narrow or broad definition of primary care provider is used)
(Jabbarpour, Y., Greiner, A., Jetty, A., Coffman, M., Jose, C., Petterson, S., 2019). While this study
used a standardized measure (MEPS data) to compare primary care spending across states, it does
have some limitations. The definition of primary care used in the analysis was based only on the
taxonomy of the provider without taking into account the particular health care services performed,
which may have resulted in an overestimate of actual primary care spending. Furthermore, nurses,
nurse practitioners and physician assistants were included as primary care providers irrespective of
whether they practiced in primary care settings because that information cannot be ascertained in the
MEPS data. In addition, some MEPS data is self-reported and may be subject to recall bias.
The Milbank Memorial Fund undertook a proof-of-concept study to assess the feasibility of
calculating primary care spending using commercial claims data (Bailit et al., 2017). The study used
national data and found that 7.1% to 8.6% of total health care spending was specifically primary
care-related. Differing interpretations of how to calculate primary care spending may have occurred,
however, because each health insurance carrier calculated and submitted its data independently.
A recent report in the Journal of the American Medical Association Internal Medicine using claims
data estimated about 2% to 4% of total medical and prescription drug spending for Medicare fee-
for-service beneficiaries was for primary care (Reid et al., 2019). In comparison, while this report
does not include Medicare fee-for-service beneficiaries, it does include Medicare Advantage
members; these estimates as a market sector were between 3.4% and 3.9%.
Oregon and Rhode Island routinely produce reports estimating primary care spending. For 2017,
Oregon estimated the percentage of total medical spending for primary care was:
• 16.5% for coordinated care organizations
• 13.4% for commercial carriers
• 12.2% for Medicare Advantage
• 10.6% for public employees and educators benefits
Rhode Island estimated primary care spending for its commercial plans to be close to 9.1% (in
2012), an increase of 3.5% from 2008.
It is difficult to compare Washington’s proportion of primary care spending to Oregon’s or Rhode
Island’s estimates due to differences in approaches and definitions of primary care. For example,
Oregon did not include any health care spending by patients such as copay, coinsurance or
deductibles while these were included in Washington’s estimates. Oregon also excluded prescription
drugs from its estimates of total claims-based payments or total medical expenditures. Per the
budget proviso, this report included all pharmacy claims costs in total medical expenditures, which
would make the percentage of primary care spending in Washington appear smaller than if these

Primary Care Expenditures Report 12
claims had been excluded. For this report, only claims paid by the primary payer are included in the
calculations to avoid any duplications of cost. It is not clear whether Oregon and Rhode Island
employed this same strategy.
Additionally, Washington’s estimates do not include non-claims-based expenditures, which are
included in estimates for Oregon and Rhode Island. When limiting Oregon’s primary care spending
to just claims-based, the estimated percentage of total medical spending for primary care for 2017
was closer to Washington’s estimates:
• 6.6% for coordinated care organizations
• 7.3% for commercial carriers
• 3.6% for Medicare Advantage
• 8% for public employees and educators benefits
Excluding non-claims-based estimates from this report produces a smaller overall estimate for
Washington, although some of these included in other states may not be exclusive to primary care.
For Oregon, many of the non-claims-based expenditures were capitated salaries for primary care or
provider incentive payments. Because Washington uses a fee-for-service equivalent for capitated
payments, the methods used in this report could be capturing some of the non-claims-based
payments that Oregon reported separately in its total.
Non-claims-based expenditures
Many services and activities are needed to fulfill the four main features of primary care services
(first-contact, continuous, comprehensive and coordinated care). These activities are not always
captured in fee-for-service expenditures submitted on health care claims. Non-claims-based
expenditures may occur in a provider’s office, be delivered by health care companies or be part of
government initiatives. Because of the broad nature of these types of activities, these investments
may not be specific to primary care (e.g., health information technology) or may be unique to certain
health care systems and populations. Collecting non-claims-based primary care expenditure
information in a standard way across payers will be difficult with current data sources. Clear
guidelines, definitions and reporting requirements, along with a critical examination of what non-
claims-based investments will benefit the delivery of primary care specifically (versus the cost of
business), should be included in future discussions on primary care expenditures.
Oregon and Rhode Island included a variety of non-claims-based expenditures in their primary care
spending estimates. Originally, Rhode Island had a requirement from its Office of the Health
Insurance Commissioner’s Affordability Standards that all commercial insurers allocate at least 35%
of their total spending on primary care to non-claims-based (Rhode Island referred to these as non-
fee-for-service) payments increasing to 40% in 2014. While these targets were retired in 2015, the
aggregate value of non-fee-for-service investments in primary care has continued to increase (King,
2019).
Non-claims-based expenditures included incentive payments to providers or practices, health
information technology investments such as health insurance exchanges, expansion of primary care
workforce with supplemental staff and other investments. Oregon and Rhode Island collected this
information directly from their health plans using Excel templates. Oregon included in rule the
definitions for non-claims-based primary care expenditures
2
and gave additional guidance in its
2
https://secure.sos.state.or.us/oard/viewSingleRule.action?ruleVrsnRsn=260735 Accessed Oct 2019.

Primary Care Expenditures Report 13
reporting templates on how to consider what expenditures to report. Rhode Island’s Office of the
Health Commissioner collects the non-claims-based information through its Affordability Standards
program, which aims to lower costs and improve quality. This program includes investment
requirements like patient-centered medical homes, but also allows for insurance companies to
submit expenditures for other types of investments for primary care (e.g., loan repayment).
Washington has no process to collect non-claims-based information from all plans that submit
claims to the WA-APCD, nor has the state developed any universal guidance or definitions of non-
claims-based expenditures. Some information outside of fee-for-service payments is submitted
through the Medicaid managed care rate development process for Medicaid and the Public
Employees Benefit Board. The Health Care Authority is developing a process to collect information
related to primary care for these programs, but OFM was not able to obtain this information for this
report.
For future primary care expenditures reports, Washington may want to consider developing a
standardized process to collect, across payers, a variety of non-claims-based investments. Outlined
below are several such areas and examples.
Provider incentives
Provider incentives such as those to encourage providers to adopt certain behaviors or pay providers
based on performance are often included in non-claims-based investments in primary care. Oregon
includes retrospective incentive payments “to primary care providers or practices based on their
performance at decreasing cost or improving value for a defined population” and prospective
incentive payments “to providers or practices aimed at developing capacity for improving care for a
defined population of patients.”
3
For example, Oregon collects information on bonus payments to
providers when they meet a target for vaccination rates. Rhode Island collects information on
incentive distributions under shared savings contracts.
Washington should consider how to collect information on provider incentives, including:
• Carrier-specific quality improvement programs aimed at specific in-network providers.
• State-sponsored quality improvement initiatives such as pay for performance metrics or
other bonus payments to providers.
• Federal quality improvement initiatives such as the Centers for Medicare and Medicaid
Services Merit-Based Incentive Payment System.
Patient-Centered Medical Home Models
According to the American College of Physicians, a Patient-Centered Medical Home, or PCMH, is a
care delivery model whereby treatment is coordinated through the patient’s primary care physician to
ensure they receive the necessary care when and where they need it, in a manner they can
understand. The Agency for Healthcare Research and Quality defines the core functions of the
medical home as follows:
4
• comprehensive care
• patient-centered
• coordinated care
3
Ibid.
4
https://pcmh.ahrq.gov/page/defining-pcmh Accessed Oct 2019.

Primary Care Expenditures Report 14
• accessible services
• quality and safety
Oregon and Rhode Island collect information from carriers on investments in PCMH models (in
addition to provider incentives). Oregon has a Patient-Centered Primary Care Home program that
allows for the inclusion of the per-member per-month payment based upon a practice’s tier level.
Rhode Island hosts a Care Transformation Collaborative, called CTC-RI, which brings together key
care stakeholders to promote care for patients with chronic disease through the PCMH model.
Rhode Island’s only multi-payer PCMH initiative, it helps practices apply for national PCMH
recognition, hire on-site care management/coordination to improve the health of patients with the
highest needs, and enhance data capabilities to manage and improve population health.
5
Additionally, Oregon and Rhode Island collect information on investments from carriers on other
PCMH initiatives.
Washington should consider how to collect information on practice and provider PCMH payments
and how to include this information in future reports, e.g., carrier-specific investments or aggregated
payments at the state level.
Investments in technology
Oregon and Rhode Island collect information on investments in primary care related to health
information technology. These investments include payments to providers to adopt electronic
medical records or payments for providers’ license fees. Additionally, Rhode Island, which requires
health insurance companies to invest in the state health information exchange called CurrentCare,
includes this investment in insurers’ non-claims-based expenditures.
In deciding which technology to include in primary care investments, Washington stakeholders
should consider not only the four main features of primary care (first-contact, continuous,
comprehensive and coordinated), but also technology advances that improve health equity. Below
are ideas for the types of technology investments that stakeholders in Washington may want to
consider:
• Technology to promote interoperability of electronic health records between providers and
facilities.
• Telehealth services including secure online chat tools for members to speak with primary
care providers and for video visits with providers.
• Texting services for reminders of appointments, lab test results or provider communication.
• Mobile applications to access medical records, pay bills or order refills on medications.
• E-consults between providers through electronic medical record platforms.
• Transcription services or talk-to-text services to help input information directly into
electronic medical records.
• Investments in OneHealthPort to improve the state’s health information exchange.
• Grants from state programs or federal programs to promote the exchange of health
information.
5
https://www.ctc-ri.org/about-us/what-ctc-ri Accessed Oct 2019.
Primary Care Expenditures Report 15
Many of the investments in technology previously mentioned may not be exclusive to primary care,
and care should be taken if these types of investments are counted toward future primary care
investments.
Workforce expenditures
In addition to typical staffing of primary care offices for administrative roles or billing, many of the
non-claims-based initiatives already mentioned — investments in technology, provider incentives
and PCMH models — require supplemental primary care staff and activities. Oregon and Rhode
Island collect non-claims-based primary care expenditures for certain workforce investments such as
practice coaches, patient educators, patient navigators and nurse case managers. Embedding
supplemental staff, including registered nurses and practice coaches, in primary care supports the
“whole person” model, will be in greater demand as the prevalence of multiple chronic conditions
increases and can improve patient health outcomes (Bauer & Bodenheimer, 2017; Grumbach, K.,
Bainbridge, E., and Bodenheimer, T., 2012).
Examples of how supplemental staff can benefit a primary care setting are:
• Implementing electronic medical records or a health information exchange.
• Providing technical support for technology enhancements in care delivery.
• Supporting adoption of new models of care delivery and continuous quality improvement.
• Helping patients change or adapt unhealthy behaviors (e.g., weight loss or smoking
cessation).
• Improving care of chronic conditions, including medication adherence.
• Connecting patients with social services.
• Improving cultural competence among clinic staff.
• Integrating behavioral health services.
• Managing continuity of care.
In addition to investments in supplemental staff, investments in primary care providers is needed to
maintain enough providers to support Washington’s growing population. Baicker and Chandra
(2004) found that states where more physicians are general practitioners have greater use of high-
quality care and lower cost per beneficiary (among Medicare patients).
Although there are numerous ways to increase and maintain the primary care provider workforce in
Washington — preventing provider burnout, increasing the number of residency slots in primary
care, increasing the funding for primary care provider education — this report will focus only on
one area, loan repayment, because Rhode Island has useful experience from which Washington can
draw information.
The Washington Student Achievement Council and the Department of Health administer two
programs to help health professionals pay back student loan debt. The median amount of that debt
is about:
• $200,000 for medical school (for class of 2018) (American Association of Medical Colleges,
2018)
• $112,500 for physician assistants (for class of 2018) (National Commission on Certification
of Physician Assistants, 2019)
• $40,000 to $55,000 for graduate nursing education (class of 2016, most recent year available)
(American Association of Colleges of Nursing, 2017)

Primary Care Expenditures Report 16
The Federal-State Loan Repayment Program, or FSLRP, awards $70,000 for loan reimbursement
with federal and state funds in return for two years of full-time work at an approved site. The Health
Professional Loan Repayment Program, or HPLRP, is a state-funded award that reimburses $75,000
of loans for three years of full-time employment (or five years for less than full-time employment).
This program requires the approved site to meet the definition of providing comprehensive primary
care services: comprehensive outpatient, ambulatory and primary health care services. This
definition includes critical access or rural hospitals but excludes all other hospitals. (Program-specific
criteria are available from the WSAC website.
6
) In the last cycle (funds obligated in fiscal year 2015–
16 and disbursed in fiscal years 2016–18 for FSLRP and fiscal years 2016–19 for HPLRP), 72
primary care providers (who also matched the definition of primary care used in this study) were
awarded more than $4.4 million in student loan debt relief.
Other investments
Additional types of investments that Oregon or Rhode Island collected and included in its non-
claims (or non-fee-for-service) primary care expenditure calculations included:
• Vaccine clinics (specifically for influenza vaccines)
• Integration of behavioral health services (outside of supplemental staff)
• Risk-based reconciliation
• Capitated or salaried expenditures not captured in claims
In considering the broad context of primary care, investments in evaluation and research on primary
care services, community-based programs to address social determinants of health and activities
undertaken by community health workers could all be counted as primary care expenditures
although they may not be part of the direct delivery of primary care services. Understanding and
defining the sphere in which primary care is taking place outside of the fee-for-service system is
essential for capturing non-claims-based investments in primary care (Baillieu et al., 2019). In
addition to what has already been mentioned about caveats to collecting non-claims-based
investments or expenditures for primary care, future reports will want to consider mechanisms to
evaluate these types of expenditures and how to allow for their inclusion over time.
Limitations of current report
This is the first comprehensive analysis of annual primary care expenditures in Washington using
claims data from the WA-APCD. Although future reports may continue to use claims data extracted
from the WA-APCD or other sources, there are inherent limitations to health care claims data from
any data source. The gaps in data identified during the study included the following:
Procedure codes
The stakeholder group conducted an extensive review of primary care procedure codes. This report
included all procedures from various reports on primary care (Bailit et al., 2017; Oregon Health
Authority and the Department of Consumer and Business Services, 2019; Reid et al., 2019) and
additional codes the stakeholder group identified as services performed in primary care settings by
primary care providers. Even with the exhaustive list of codes, there could still be procedures that
were not included in this report, but are billed for by primary care providers (e.g., hospice visits,
6
https://wsac.wa.gov/sites/default/files/2019.FSLRP.HPLRP.Guide.pdf Accessed Sept 2019.
Primary Care Expenditures Report 17
charges for vaccines). Caution should be used when comparing this report to other reports that do
not use the same codes.
No primary care location indicator
We were not able to identify if the setting for the primary care service was a primary care clinic or
other type of health care setting; this information is not captured on claims submitted to the WA-
APCD. It is unclear if this underestimated or overestimated the true level of primary care
expenditures for the state. OFM is working on solutions to gather the primary care location
information for future reports.
No primary care provider roster or consensus on definition
Without a roster or other continually updated source for primary care providers for Washington,
stakeholder groups will need to determine and define who is a primary care provider outside of
relying on just the taxonomy code. This is especially important for nurse practitioners and physician
assistants: It is unclear from the methods used to define primary care and the adjustment used for
nurse practitioners and physician assistants if we over- or under-estimated primary care providers for
the state. Additionally, not all reports have included obstetrics and behavioral health as primary care
providers. Without a national standard or consensus on definition of primary care providers, it will
continue to be difficult to compare estimates between reports.
Bundled payment services
As health care services move to bundled payments for services (e.g., obstetrics), it becomes difficult
to carve out which services are attributable or defined as primary care (e.g., prenatal visits). Future
reports should consider possible adjustments to methodology to identify and capture primary care
services within bundled payments.
Federally Qualified Health Centers and rural health centers
Claims submitted by Federally Qualified Health Centers or rural health centers may be submitted by
the facility or by the individual provider. Because this practice varies by location, an accurate
estimate of primary care services delivered at or by these facilities cannot be determined.
Integrated delivery systems
Some health insurance carriers are part of integrated delivery systems or use capitated payments.
These type of systems do not follow the traditional fee-for-service model when paying for health
care services. Although the methodology in this report used the fee-for-service equivalent in claims
data for capitated payments, there could still be an underestimate of primary care expenditures for
these services that could result in an underestimate of the true primary care investment by these
health insurance carriers.
Medicaid fee-for-service and Medicare fee-for-service claims
Neither Oregon nor Rhode Island, nor the current report for Washington include Medicaid fee-for-
service or Medicare fee-for-service primary care expenditures. These results could be inferred from
results calculated for Medicare Advantage and Medicaid managed care organizations, but these
results would not take into account differences in population characteristics, health status or
reimbursement rates between the fee-for-service groups and the managed care groups. Future
reports may want to consider including these health insurance claims to better understand how
investments in primary care differ among these populations.
Primary Care Expenditures Report 18
Non-claims-based expenditures
As discussed previously in this report, there is no standardized statewide system in place to collect
non-claims-based expenditures from health insurance carriers in Washington. Although not all
primary care reports have used this type of data, Oregon and Rhode Island used it in their reports.
Without non-claims-based expenditures, estimates of primary care spending will appear lower in
Washington compared with states that collect these data.
Future considerations
This report provides a baseline estimate of primary care spending in Washington. This estimate can
be used to monitor primary care spending and to compare the impacts of new investments and
initiatives. Future reports should continue to evaluate limitations to evolving methodology and
measurements. However, if future iterations of this report update or add codes or services, any
changes in spending results could be due to these changes in methodology and may not be the result
of any policy or behavior change. Oregon updated its inclusion of costs and primary care service
codes between its reports released in 2018 and 2019 (Oregon Health Authority and the Department
of Consumer and Business Services, 2019). There was no discussion on how this may have
influenced its primary care expenditure results between reports.
Because primary care utilization is heavily influenced by needs of the population, future reports may
include more detailed stratifications of population characteristics (e.g., sex, comorbidity, geography)
to better understand variations in primary care spending. These population characteristics could help
explain differences in primary care spending by market sector and by carriers outside of provider
networks and business agreements.
This report cannot differentiate how spending among carriers in different market sectors correlates
with quality of services, patient and provider satisfaction, or population health outcomes. If
additional population characteristics are included in future reports, additional indicators previously
mentioned should also be considered for collection
If non-claims-based expenditures are to be collected and included in future iterations of this report,
care should be given on whether to consider these types of investments as spending in addition to
what is identified from claims and fee-for-service expenditures.
Conclusion
This primary care spending report provides not only a baseline to compare new investments or
initiatives, but also caveats and considerations for how to continue to measure primary care
expenditures.
The results in this report highlight a low rate of investment in primary care in Washington. Based on
current research, the health care system would benefit from increased primary care investments. To
ensure the best results, decisions should be guided by additional research into best practices based
on current evidence, available data and broad stakeholder input. Monitoring the impact of policies
and system performance will be key to successfully strengthening Washington’s primary care system
(Center for Health Care Strategies and State Health Access Data Assistance Center, 2014).
Primary Care Expenditures Report 19
Future stakeholders should pose the following questions suggested by Koller et al (Koller, C.F.,
Khullar, 2017):
• What is the right level of primary care spending based on evidence?
• How large of an improvement in care outcomes could be expected with a unit increase in
primary care spending?
• How does the effect of additional spending on primary care vary with the patient population
being served?
State-level efforts to control costs and increase primary care spending are possible. Rhode Island’s
efforts to control costs have resulted in decreased overall spending among commercial insurers
through lower prices while increasing primary care spending without affecting quality or utilization
(Baum et al., 2019).
Primary Care Expenditures Report 20
References
American Association of Colleges of Nursing. (2017). The Numbers Behind the Degree: Financing
Graduate Nursing Education. Retrieved from https://www.aacnnursing.org/Policy-
Advocacy/View/ArticleId/20715/AACN-Releases-2017-Graduate-Nursing-Student-Debt-
Report
American Association of Medical Colleges. (2018). October 2018 Medical Student Education: Debt,
Costs, and Loan Repayment Fact Card. Retrieved October 17, 2019, from
https://store.aamc.org/downloadable/download/sample/sample_id/240/
Baicker, K., & Chandra, A. (2004). Medicare spending, the physician workforce, and beneficiaries’
quality of care. Health Affairs, 23(SUPPL.), 184–197. https://doi.org/10.1377/hlthaff.W4.184
Bailit, M. H., Friedberg, M. W., & Houy, M. L. (2017). Standardizing the Measurement of Commercial
Health Plan Primary Care Spending. Retrieved from www.milbank.org
Baillieu, R., Kidd, M., Phillips, R., Roland, M., Mueller, M., Morgan, D., … Bazemore, A. (2019).
The Primary Care Spend Model: A systems approach to measuring investment in primary care.
BMJ Global Health, 4(4). https://doi.org/10.1136/bmjgh-2019-001601
Basu, S., Berkowitz, S. A., Phillips, R. L., Bitton, A., Landon, B. E., & Phillips, R. S. (2019).
Association of Primary Care Physician Supply With Population Mortality in the United States,
2005-2015. JAMA Internal Medicine, 179(4), 506–514.
https://doi.org/10.1001/jamainternmed.2018.7624
Bauer, L., & Bodenheimer, T. (2017). Expanded roles of registered nurses in primary care delivery of
the future. Nursing Outlook, 65(5), 624–632. https://doi.org/10.1016/j.outlook.2017.03.011
Baum, A., Song, Z., Landon, B. E., Phillips, R. S., Bitton, A., & Basu, S. (2019). Health care
spending slowed after Rhode Island applied affordability standards to commercial insurers.
Health Affairs, 38(2), 237–245. https://doi.org/10.1377/hlthaff.2018.05164
Center for Health Care Strategies & State Health Access Data Assistance Center. (2014). Multi-Payer
Investments in Primary Care: Policy and Measurement Strategies. Trenton, NJ.
Centers for Disease Control and Prevention. (2019). Tables of Summary Health Statistics for U.S. Adults:
2018 National Health Interview (Vol. 0). Retrieved from
http://www.cdc/gov/nchs/nhs/SHS/tables.htm
Donaldson, M.S., Yordy, K.D., Lohr, K.N., & Vanselow, N. A. (Ed.). (1996). Primary Care: America’s
Health in a New Era. https://doi.org/10.1002/clc.4960190202
Friedberg, M. W., Hussey, P. S., & Schneider, E. C. (2010). Primary care: A critical review of the
evidence on quality and costs of health care. Health Affairs, 29(5), 766–772.
https://doi.org/10.1377/hlthaff.2010.0025
Glass, D. P., Kanter, M. H., Jacobsen, S. J., & Minardi, P. M. (2017). The impact of improving
access to primary care. Journal of Evaluation in Clinical Practice, 23(6), 1451–1458.
https://doi.org/10.1111/jep.12821
Primary Care Expenditures Report 21
Grumbach, K., Bainbridge, E., and Bodenheimer, T. (2012). Facilitating Improvement in Primary
Care: The Promise of Practice Coaching. Commonwealth Fund, 15 (pub. 1605). Retrieved from
https://www.commonwealthfund.org/sites/default/files/documents/___media_files_publicat
ions_issue_brief_2012_jun_1605_grumbach_facilitating_improvement_primary_care_practice_
coaching.pdf
Jabbarpour, Y., Greiner, A., Jetty, A., Coffman, M., Jose, C., Petterson, S. et al. (2019). Investing in
primary care: A state-level analysis. Retrieved from https://www.pcpcc.org/resource/evidence2019
Kaplan, L., & Gill, J. (2018). 2018 Washington State Advanced Registered Nurse Practitioner Survey Data
Report. Vancouver, WA.
King, C. (2019). Email Communication.
Koller, C.F., Khullar, D. (2017). Primary Care Spending Rate – A Lever for Encouraging Investment
in Primary Care. New England Journal of Medicine, 377(18), 1709–1711.
National Commission on Certification of Physician Assistants. (2019). 2018 Statistical Profile of Recently
Certified Physician Assistants: An Annual Report of the National Commission on Certification of Physician
Assistants. Retrieved from http://www.nccpa.net
OECD. (2017). Health at a Glance 2017: OECD Indicators. Retrieved from
http://dx.doi.org/10.1787/health_glance-2017-en
Oregon Health Authority and the Department of Consumer and Business Services. (2019). Primary
Care Spending in Oregon: A Report to the Oregon Legislature. Retrieved from
https://www.oregon.gov/oha/HPA/ANALYTICS/Documents/SB-231-Report-2019.pdf
Reid, R., Damberg, C., & Friedberg, M. W. (2019, July 1). Primary Care Spending in the Fee-for-
Service Medicare Population. JAMA Internal Medicine, Vol. 179, pp. 977–980.
https://doi.org/10.1001/jamainternmed.2018.8747
Starfield, B., Shi, L., Macinko, J. (2005). Contribution of primary care to health systems and health.
Milbank Quarterly, 83(3), 457–502.
Starfield, B. (1998). Primary Care: Balancing Health Needs, Services, and Technology. New York, NY:
Oxford University Press.
Washington Medical Commission. (2019). Physician Assistant Demographic Census Aggregate Report.
Retrieved from https://wmc.wa.gov/sites/default/files/public/PAReportOctober2019.pdf
Yen, W. (2018). 2016 Physician Supply. Retrieved from
https://www.ofm.wa.gov/sites/default/files/public/dataresearch/healthcare/workforce/physi
cian_supply_2016.pdf
Primary Care Expenditures Report 22
Appendix A: Budget proviso
ESHB 1109, Section 131(9)
(9) $110,000 of the general fund—state appropriation for fiscal year 2020 is provided solely for the
office of financial management to determine annual primary care medical expenditures in
Washington, by insurance carrier, in total and as a percentage of total medical expenditure. Where
feasible, this determination must also be broken down by relevant characteristics such as whether
expenditures were for in-patient or out-patient care, physical or mental health, by type of provider,
and by payment mechanism.
(a) The determination must be made in consultation with statewide primary care provider
organizations using the state's all payer claims database and other existing data.
(b) For purposes of this section:
(i) "Primary care" means family medicine, general internal medicine, and general
pediatrics.
(ii) "Primary care provider" means a physician, naturopath, nurse practitioner,
physician assistant, or other health professional licensed or certified in Washington
state whose clinical practice is in the area of primary care.
(iii) "Primary care medical expenditures" means payments to reimburse the cost of
physical and mental health care provided by a primary care provider, excluding
prescription drugs, vision care, and dental care, whether paid on a fee-for-service
basis or as a part of a capitated rate or other type of payment mechanism.
(iv) "Total medical expenditure" means payments to reimburse the cost of all health
care and prescription drugs, excluding vision care and dental care, whether paid on a
fee-for-service basis or as part of a capitated rate or other type of payment
mechanism.
(c) By December 1, 2019, the office of financial management shall report its findings to the
legislature, including an explanation of its methodology and any limits or gaps in existing
data which affected its determination.
Primary Care Expenditures Report 23
Appendix B: Primary Care Expenditures Stakeholder Group
Office of Financial Management staff:
Thea Mounts
Mandy Stahre
Advanced Registered Nurse Practitioners United of Washington State:
Devon S. Connor-Green
Louise Kaplan
Washington Academy of Family Physicians:
Tony Butruille
Jonathan Seib
Alexa Silver
Jonathan Sugarman
Washington Chapter of the American Academy of Pediatrics:
Francie Chalmers
Sarah Rafton
Amber Ulvenes
University of Washington Center for Health Workforce Studies:
Bianca Frogner
Davis Patterson
Susan Skillman
University of Washington Department of Global Health:
Matthew Thompson
Washington Health Care Authority:
Rachel Quinn
Emily Transue
Judy Zerzan

Primary Care Expenditures Report 24
Appendix C: List of providers
Narrow definition of primary care provider
Taxonomy Code
Description
207Q00000X
Family Medicine
207QA0000X
Family Medicine, Adolescent Medicine
207QA0505X
Family Medicine, Adult Medicine
207QG0300X
Family Medicine, Geriatric Medicine
261QF0400X
Federally Qualified Health Center
208D00000X
General Practice
207R00000X
Internal Medicine
207RG0300X
Internal Medicine, Geriatric Medicine
175F00000X
Naturopath
208000000X
Pediatrics
2080A0000X
Pediatrics, Adolescent Medicine
2083P0500X
Preventive Medicine, Preventive
Medicine/Occupational Environmental Medicine
261QP2300X
Primary care clinic
261QR1300X
Rural health clinic
Nurse practitioner and physician assistant definitions
Taxonomy Code
Description
363L00000X
Nurse Practitioner
363LA2100X
Nurse Practitioner, Acute Care
363LA2200X
Nurse Practitioner, Adult Health
363LC1500X
Nurse Practitioner, Community Health
363LC0200X
Nurse Practitioner, Critical Care Medicine
363LF0000X
Nurse Practitioner, Family
363LG0600X
Nurse Practitioner, Gerontology
363LN0000X
Nurse Practitioner, Neonatal
363LN0005X
Nurse Practitioner, Neonatal, Critical Care
363LX0001X
Nurse Practitioner, Obstetrics & Gynecology
363LX0106X
Nurse Practitioner, Occupational Health
363LP0200X
Nurse Practitioner, Pediatrics
363LP0222X
Nurse Practitioner, Pediatrics, Critical Care
363LP1700X
Nurse Practitioner, Perinatal
363LP2300X
Nurse Practitioner, Primary Care
363LP0808X
Nurse Practitioner, Psychiatric/Mental Health
363LS0200X
Nurse Practitioner, School
363LW0102X
Nurse Practitioner, Women’s Health
363A00000X
Physician Assistant
363AM0700X
Physician Assistant, Medical
363AS0400X
Physician Assistant, Surgical

Primary Care Expenditures Report 25
Broad definition of primary care provider
Taxonomy Code
Description
367A00000X
Advanced Practice Midwife
106E00000X Assistant Behavior Analyst
106S00000X Behavior Technician
103K00000X
Behavioral Analyst
103G00000X Clinical Neuropsychologist
364S00000X Clinical Nurse Specialist
163W00000X Registered Nurse
101Y00000X
Counselor
101YA0400X Counselor, Addiction (Substance Use Disorder)
101YM0800X Counselor, Mental Health
101YP1600X
Counselor, Pastoral
101YP2500X Counselor, Professional
101YS0200X Counselor, School
207QA0401X
Family Medicine, Addiction Medicine
207QB0002X Family Medicine, Bariatric Medicine
207QH0002X Family Medicine, Hospice and Palliative Medicine
207QS1201X Family Medicine, Sleep Medicine
207QS0010X
Family Medicine, Sports Medicine
175L00000X Homeopath
207RA0401X Internal Medicine, Addiction Medicine
106H00000X
Marriage & Family Therapist
176B00000X Midwife
207V00000X Obstetrics & Gynecology
207VG0400X
Obstetrics & Gynecology, Gynecology
2080P0006X
Pediatrics, Developmental – Behavioral Pediatrics
2080P0008X Pediatrics, Neurodevelopmental Disabilities
2084A0401X
Psychiatry & Neurology, Addiction Medicine
2084P0802X
Psychiatry & Neurology, Addiction Psychiatry
Broad definition of primary care provider
Taxonomy Code
Description
2084P0804X
Psychiatry & Neurology, Child & Adolescent
Psychiatry
2084F0202X Psychiatry & Neurology, Forensic Psychiatry
2084P0805X Psychiatry & Neurology, Geriatric Psychiatry
2084P0005X
Psychiatry & Neurology, Neurodevelopmental
Disabilities
2084P0800X
Psychiatry & Neurology, Psychiatry
2084P0015X Psychiatry & Neurology, Psychosomatic Medicine
102L00000X Psychoanalyst
103T00000X
Psychologist
103TA0400X Psychologist, Addiction (Substance Use Disorder)
103TA0700X Psychologist, Adult Development & Aging
103TC0700X
Psychologist, Clinical
103TC2200X Psychologist, Clinical Child & Adolescent
103TB0200X Psychologist, Cognitive & Behavioral
103TC1900X Psychologist, Counseling
103TE1000X
Psychologist, Educational
103TE1100X Psychologist, Exercise & Sports
103TF0000X Psychologist, Family
103TF0200X
Psychologist, Forensic
103TP2701X Psychologist, Group Psychotherapy
103TH0004X Psychologist, Health
103TH0100X
Psychologist, Health Service
103TM1700X
Psychologist, Men & Masculinity
103TM1800X
Psychologist, Mental Retardation & Developmental
Disabilities
103TP0016X Psychologist, Prescribing (Medical)
103TP0814X
Psychologist, Psychoanalysis
103TP2700X Psychologist, Psychotherapy
103TR0400X Psychologist, Rehabilitation

Primary Care Expenditures Report 26
Broad definition of primary care provider
Taxonomy Code
Description
103TS0200X
Psychologist, School
103TW0100X Psychologist, Women
104100000X Social Worker
1041C0700X
Social Worker, Clinical
1041S0200X Social Worker, School

Primary Care Expenditures Report 27
Appendix D: Procedure codes
Narrow definition of procedures
HCPCs or
CPT codes
Procedure Category Procedure Long Description
99497
Advance Care Planning Evaluation &
Management Services
ADVANCE CARE PLANNING FIRST 30 MINS
99498
Advance Care Planning Evaluation &
Management Services
ADVANCE CARE PLANNING EA ADDL 30 MINS
99450
Basic Life and/or Disability Exam
BASIC LIFE AND/OR DISABILITY EXAMINATION
99455 Basic Life and/or Disability Exam WORK RELATED/MED DBLT XM TREATING PHYS
99456 Basic Life and/or Disability Exam WORK RELATED/MED DBLT XM OTH/THN TREATING PHYS
99366 Case Management Services TEAM CONFERENCE FACE-TO-FACE NONPHYSICIAN
99367 Case Management Services TEAM CONFERENCE NON-FACE-TO-FACE PHYSICIAN
99368
Case Management Services
TEAM CONFERENCE NON-FACE-TO-FACE NONPHYSICIAN
99487
Chronic Care Management Services
CMPLX CHRON CARE MGMT W/O PT VST 1ST HR PER MO
99489
Chronic Care Management Services
CMPLX CHRON CARE MGMT EA ADDL 30 MIN PER MONTH
99490
Chronic Care Management Services
CHRON CARE MANAGEMENT SRVC 20 MIN PER MONTH
G0506
Chronic Care Management Services
COMP ASMT OF & CARE PLNG PT RQR CC MGMT SRVC
99241
Consultation Services
OFFICE CONSULTATION NEW/ESTAB PATIENT 15 MIN
99242 Consultation Services OFFICE CONSULTATION NEW/ESTAB PATIENT 30 MIN
99243 Consultation Services OFFICE CONSULTATION NEW/ESTAB PATIENT 40 MIN
99244 Consultation Services OFFICE CONSULTATION NEW/ESTAB PATIENT 60 MIN
G0438 Counseling, Screening, & Prevention Services ANNUAL WELLNESS VISIT; PERSONALIZ PPS INIT VISIT
G0439
Counseling, Screening, & Prevention Services
ANNUAL WELLNESS VST; PERSONALIZED PPS SUBSQT VST
G0442
Counseling, Screening, & Prevention Services
ANNUAL ALCOHOL MISUSE SCREENING 15 MINUTES
G0443
Counseling, Screening, & Prevention Services
BRIEF FACE-FACE BEHAV CNSL ALCOHL MISUSE 15 MIN
99324
Domiciliary, Rest Home or Custodial Care
DOMICIL/REST HOME NEW PT VISIT LOW SEVER 20 MIN
99325
Domiciliary, Rest Home or Custodial Care
DOMICIL/REST HOME NEW PT VISIT MOD SEVER 30 MIN
99326
Domiciliary, Rest Home or Custodial Care
DOMICIL/REST HOME NEW PT HI-MOD SEVER 45 MINUTES
99327 Domiciliary, Rest Home or Custodial Care DOMICIL/REST HOME NEW PT VISIT HI SEVER 60 MIN

Primary Care Expenditures Report 28
Narrow definition of procedures
HCPCs or
CPT codes
Procedure Category Procedure Long Description
99328
Domiciliary, Rest Home or Custodial Care
DOM/R-HOME E/M NEW PT SIGNIF NEW PROB 75 MINUTES
99334
Domiciliary, Rest Home or Custodial Care
DOM/R-HOME E/M EST PT SELF-LMTD/MINOR 15 MINUTES
99335
Domiciliary, Rest Home or Custodial Care
DOM/R-HOME E/M EST PT LW MOD SEVERITY 25 MINUTES
99336
Domiciliary, Rest Home or Custodial Care
DOM/R-HOME E/M EST PT MOD HI SEVERITY 40 MINUTES
99337 Domiciliary, Rest Home or Custodial Care DOM/R-HOME E/M EST PT SIGNIF NEW PROB 60 MINUTES
99078 Educational Service Group Setting PHYS/QHP EDUCATION SVCS RENDERED PTS GRP SETTING
G0466 FQHC Visits FEDERALLY QUALIFIED HEALTH CENTER VISIT NEW PT
G0467 FQHC Visits FEDERALLY QUALIFIED HEALTH CENTER VISIT ESTAB PT
G0468 FQHC Visits FEDERALLY QUALIFIED HEALTH CENTER VISIT IPPE/AWV
G0469
FQHC Visits
FED QUAL HEALTH CNTR VISIT MENTAL HEALTH NEW PT
G0470
FQHC Visits
FED QUAL HEALTH CNTR VST MENTAL HEALTH ESTAB PT
T1015
FQHC Visits - T1015
CLINIC VISIT/ENCOUNTER ALL-INCLUSIVE
96160
Health Risk Assessment & Screenings
PT-FOCUSED HLTH RISK ASSMT SCORE DOC STND INSTRM
96161
Health Risk Assessment & Screenings
CAREGIVER HLTH RISK ASSMT SCORE DOC STND INSTRM
99339
Health Risk Assessment & Screenings
INDIV PHYS SUPVJ HOME/DOM/R-HOME MO 15-29 MIN
99340 Health Risk Assessment & Screenings INDIV PHYS SUPVJ HOME/DOM/R-HOME MO 30 MIN/>
99483 Health Risk Assessment & Screenings ASSMT & CARE PLANNING PT W/COGNITIVE IMPAIRMENT
G0396 Health Risk Assessment & Screenings ALCOHOL &/SUBSTANCE ABUSE ASSESSMENT 15-30 MIN
G0397 Health Risk Assessment & Screenings ALCOHOL &/SUBSTANCE ABUSE ASSESSMENT >30 MIN
G0444
Health Risk Assessment & Screenings
ANNUAL DEPRESSION SCREENING 15 MINUTES
G0505
Health Risk Assessment & Screenings
COGN & FUNCT ASMT USING STD INST OFF/OTH OP/HOME
99341
Home Health Services
HOME VISIT NEW PATIENT LOW SEVERITY 20 MINUTES
99342
Home Health Services
HOME VISIT NEW PATIENT MOD SEVERITY 30 MINUTES
99343
Home Health Services
HOME VST NEW PATIENT MOD-HI SEVERITY 45 MINUTES
99344
Home Health Services
HOME VISIT NEW PATIENT HI SEVERITY 60 MINUTES
99345 Home Health Services HOME VISIT NEW PT UNSTABL/SIGNIF NEW PROB 75 MIN

Primary Care Expenditures Report 29
Narrow definition of procedures
HCPCs or
CPT codes
Procedure Category Procedure Long Description
99347
Home Health Services
HOME VISIT EST PT SELF LIMITED/MINOR 15 MINUTES
99348
Home Health Services
HOME VISIT EST PT LOW-MOD SEVERITY 25 MINUTES
99349
Home Health Services
HOME VISIT EST PT MOD-HI SEVERITY 40 MINUTES
99350
Home Health Services
HOME VST EST PT UNSTABLE/SIGNIF NEW PROB 60 MINS
99374 Home Health Services SUPVJ PT HOME HEALTH AGENCY MO 15-29 MINUTES
99375 Home Health Services SUPERVISION PT HOME HEALTH AGENCY MONTH 30 MIN/>
99376 Home Health Services CARE PLAN OVERSIGHT/OVER
G0179 Home Health Services PHYS RE-CERT MCR-COVR HOM HLTH SRVC RE-CERT PRD
G0180 Home Health Services PHYS CERT MCR-COVR HOM HLTH SRVC PER CERT PRD
G0181
Home Health Services
PHYS SUPV PT RECV MCR-COVR SRVC HOM HLTH AGCY
G0463
Hospital Outpatient Clinic Visit
HOSPITAL OUTPATIENT CLIN VISIT ASSESS & MGMT PT
90460
Immunization Administration for
Vaccines/Toxoids
IM ADM THRU 18YR ANY RTE 1ST/ONLY COMPT VAC/TOX
90461
Immunization Administration for
Vaccines/Toxoids
IM ADM THRU 18YR ANY RTE ADDL VAC/TOX COMPT
90471
Immunization Administration for
Vaccines/Toxoids
IM ADM PRQ ID SUBQ/IM NJXS 1 VACCINE
90472
Immunization Administration for
Vaccines/Toxoids
IM ADM PRQ ID SUBQ/IM NJXS EA VACCINE
90473
Immunization Administration for
Vaccines/Toxoids
IM ADM INTRANSL/ORAL 1 VACCINE
90474
Immunization Administration for
Vaccines/Toxoids
IM ADM INTRANSL/ORAL EA VACCINE
G0402 Initial Services for Medicare Enrollment INIT PREV PE LTD NEW BENEF DUR 1ST 12 MOS MCR
96372 Injections THERAPEUTIC PROPHYLACTIC/DX INJECTION SUBQ/IM
11055
Minor Procedures and Tests
PARING/CUTTING BENIGN HYPERKERATOTIC LESION 1
11056
Minor Procedures and Tests
PARING/CUTTING BENIGN HYPERKERATOTIC LESION 2-4
11200
Minor Procedures and Tests
REMOVAL SKN TAGS MLT FIBRQ TAGS ANY AREA UPW/15
11201
Minor Procedures and Tests
REMOVAL SK TGS MLT FIBRQ TAGS ANY AREA EA 10

Primary Care Expenditures Report 30
Narrow definition of procedures
HCPCs or
CPT codes
Procedure Category Procedure Long Description
11719
Minor Procedures and Tests
TRIMMING NONDYSTROPHIC NAILS ANY NUMBER
11720
Minor Procedures and Tests
DEBRIDEMENT NAIL ANY METHOD 1-5
11721
Minor Procedures and Tests
DEBRIDEMENT NAIL ANY METHOD 6/>
11740
Minor Procedures and Tests
EVACUATION SUBUNGUAL HEMATOMA
11900 Minor Procedures and Tests INJECTION INTRALESIONAL UP TO & INCLUD 7 LESIONS
11901 Minor Procedures and Tests INJECTION INTRALESIONAL >7 LESIONS
15851 Minor Procedures and Tests REMOVAL SUTURES UNDER ANESTHESIA OTHER SURGEON
16020 Minor Procedures and Tests DRS&/DBRDMT PRTL-THKNS BURNS 1ST/SBSQ SMALL
17110 Minor Procedures and Tests DESTRUCTION BENIGN LESIONS UP TO 14
17111
Minor Procedures and Tests
DESTRUCTION BENIGN LESIONS 15/>
24640
Minor Procedures and Tests
CLTX RDL HEAD SUBLXTJ CHLD NURSEMAID ELBW W/MANJ
30300
Minor Procedures and Tests
REMOVAL FOREIGN BODY INTRANASAL OFFICE PROCEDURE
36415
Minor Procedures and Tests
COLLECTION VENOUS BLOOD VENIPUNCTURE
36416
Minor Procedures and Tests
COLLECTION CAPILLARY BLOOD SPECIMEN
43760
Minor Procedures and Tests
CHANGE GASTROSTOMY TUBE PERCUTANEOUS W/O GDNCE
51702 Minor Procedures and Tests INSJ TEMP NDWELLG BLADDER CATHETER SIMPLE
54150 Minor Procedures and Tests CIRCUMCISION W/CLAMP/OTH DEV W/BLOCK
57170 Minor Procedures and Tests DIAPHRAGM/CERVICAL CAP FITTING W/INSTRUCTIONS
69200 Minor Procedures and Tests RMVL FB XTRNL AUDITORY CANAL W/O ANES
69210
Minor Procedures and Tests
REMOVAL IMPACTED CERUMEN INSTRUMENTATION UNILAT
81000
Minor Procedures and Tests
URINLS DIP STICK/TABLET REAGNT NON-AUTO MICRSCPY
81001
Minor Procedures and Tests
URNLS DIP STICK/TABLET REAGENT AUTO MICROSCOPY
81002
Minor Procedures and Tests
URNLS DIP STICK/TABLET RGNT NON-AUTO W/O MICRSCP
81025
Minor Procedures and Tests
URINE PREGNANCY TEST VISUAL COLOR CMPRSN METHS
82044
Minor Procedures and Tests
URINE ALBUMIN SEMIQUANTITATIVE
82270 Minor Procedures and Tests BLOOD OCCULT PEROXIDASE ACTV QUAL FECES 1 DETER

Primary Care Expenditures Report 31
Narrow definition of procedures
HCPCs or
CPT codes
Procedure Category Procedure Long Description
82272
Minor Procedures and Tests
BLOOD OCCULT PEROXIDASE ACTV QUAL FECES 1-3 SPEC
82465
Minor Procedures and Tests
CHOLESTEROL SERUM/WHOLE BLOOD TOTAL
82947
Minor Procedures and Tests
GLUCOSE QUANTITATIVE BLOOD XCPT REAGENT STRIP
82948
Minor Procedures and Tests
GLUCOSE BLOOD REAGENT STRIP
82950 Minor Procedures and Tests GLUCOSE POST GLUCOSE DOSE
82962 Minor Procedures and Tests GLUC BLD GLUC MNTR DEV CLEARED FDA SPEC HOME USE
83718 Minor Procedures and Tests LIPOPROTEIN DIR MEAS HIGH DENSITY CHOLESTEROL
85013 Minor Procedures and Tests BLOOD COUNT SPUN MICROHEMATOCRIT
85014 Minor Procedures and Tests BLOOD COUNT HEMATOCRIT
85018
Minor Procedures and Tests
BLOOD COUNT HEMOGLOBIN
86580
Minor Procedures and Tests
SKIN TEST TUBERCULOSIS INTRADERMAL
87205
Minor Procedures and Tests
SMR PRIM SRC GRAM/GIEMSA STAIN BCT FUNGI/CELL
87880
Minor Procedures and Tests
IAADIADOO STREPTOCOCCUS GROUP A
92551
Minor Procedures and Tests
SCREENING TEST PURE TONE AIR ONLY
92567
Minor Procedures and Tests
TYMPANOMETRY
93000 Minor Procedures and Tests ECG ROUTINE ECG W/LEAST 12 LDS W/I&R
93005 Minor Procedures and Tests ECG ROUTINE ECG W/LEAST 12 LDS TRCG ONLY W/O I&R
93010 Minor Procedures and Tests ECG ROUTINE ECG W/LEAST 12 LDS I&R ONLY
93040 Minor Procedures and Tests RHYTHM ECG 1-3 LEADS W/INTERPRETATION & REPORT
93268
Minor Procedures and Tests
XTRNL PT ACTIV ECG TRANSMIS W/R&I </30 DAYS
93270
Minor Procedures and Tests
XTRNL PT ACTIVATED ECG RECORD MONITOR 30 DAYS
93272
Minor Procedures and Tests
XTRNL PT ACTIVTD ECG DWNLD W/R&I </30 DAYS
93784
Minor Procedures and Tests
AMBL BLD PRESS W/TAPE&/DISK 24/> HR ALYS I&R
94010
Minor Procedures and Tests
SPMTRY W/VC EXPIRATORY FLO W/WO MXML VOL VNTJ
94060
Minor Procedures and Tests
BRNCDILAT RSPSE SPMTRY PRE&POST-BRNCDILAT ADMN
94640 Minor Procedures and Tests PRESSURIZED/NONPRESSURIZED INHALATION TREATMENT

Primary Care Expenditures Report 32
Narrow definition of procedures
HCPCs or
CPT codes
Procedure Category Procedure Long Description
94664
Minor Procedures and Tests
DEMO&/EVAL OF PT UTILIZ AERSL GEN/NEB/INHLR/IP
94760
Minor Procedures and Tests
NONINVASIVE EAR/PULSE OXIMETRY SINGLE DETER
94761
Minor Procedures and Tests
NONINVASIVE EAR/PULSE OXIMETRY MULTIPLE DETER
95115
Minor Procedures and Tests
PROF SVCS ALLG IMMNTX X W/PRV ALLGIC XTRCS 1 NJX
95117 Minor Procedures and Tests PROF SVCS ALLG IMMNTX X W/PRV ALLGIC XTRCS NJXS
97597 Minor Procedures and Tests DEBRIDEMENT OPEN WOUND 20 SQ CM/<
97602 Minor Procedures and Tests RMVL DEVITAL TISS N-SLCTV DBRDMT W/O ANES 1 SESS
99000 Minor Procedures and Tests HANDLG&/OR CONVEY OF SPEC FOR TR OFFICE TO LAB
99050 Minor Procedures and Tests SERVICES PROVIDED OFFICE OTH/THN REG SCHED HOURS
99051
Minor Procedures and Tests
SVC PRV OFFICE REG SCHEDD EVN WKEND/HOLIDAY HRS
99058
Minor Procedures and Tests
SVC PRV EMER BASIS IN OFFICE DISRUPTING SVCS
A4627
Minor Procedures and Tests
SPACR BAG/RESRVOR W/WO MASK W/METRD DOSE INHAL
A6448
Minor Procedures and Tests
LT COMPRS BANDGE ELAST WDTH < 3 IN PER YARD
A6449
Minor Procedures and Tests
LT COMPRS BANDGE ELAST WDTH >/= 3 & <5 IN PER YD
A7003
Minor Procedures and Tests
ADMN SET SM VOL NONFILTR PNEUMAT NEBULIZR DISPBL
A7015 Minor Procedures and Tests AREO MASK USED W/ DME NEB
G0403 Minor Procedures and Tests ECG RTN ECG W/12 LEADS SCR INIT PREVNTV PE W/I&R
G0404 Minor Procedures and Tests ECG RTN ECG W/12 LEADS TRACING ONLY W/O I&R
G0405 Minor Procedures and Tests ECG RTN ECG W/12 LEADS INTERPR & REPORT ONLY
S8100
Minor Procedures and Tests
HOLDING CHAMB/SPACR W/INHAL/NEBULIZR; W/O MASK
S8101
Minor Procedures and Tests
HOLDING CHAMB/SPACR W/AN INHAL/NEBULIZR; W/MASK
99460
Newborn Care Services
1ST HOSP/BIRTHING CENTER CARE PER DAY NML NB
99461
Newborn Care Services
1ST CARE PR DAY NML NB XCPT HOSP/BIRTHING CENTER
99462
Newborn Care Services
SUBQ HOSPITAL CARE PER DAY E/M NORMAL NEWBORN
99463
Newborn Care Services
1ST HOSP/BIRTHING CENTER NB ADMIT & DSCHG SM DAT
98969 Non-Face-to-Face Non-Physician Services NONPHYSICIAN ONLINE ASSESSMENT AND MANAGEMENT

Primary Care Expenditures Report 33
Narrow definition of procedures
HCPCs or
CPT codes
Procedure Category Procedure Long Description
99441
Non-Face-to-Face Physician Services
PHYS/QHP TELEPHONE EVALUATION 5-10 MIN
99442
Non-Face-to-Face Physician Services
PHYS/QHP TELEPHONE EVALUATION 11-20 MIN
99443
Non-Face-to-Face Physician Services
PHYS/QHP TELEPHONE EVALUATION 21-30 MIN
99444
Non-Face-to-Face Physician Services
PHYS/QHP ONLINE EVALUATION & MANAGEMENT SERVICE
99446 Non-Face-to-Face Physician Services NTRPROF PHONE/NTRNET/EHR ASSMT&MGMT 5-10 MIN
99447 Non-Face-to-Face Physician Services NTRPROF PHONE/NTRNET/EHR ASSMT&MGMT 11-20 MIN
99448 Non-Face-to-Face Physician Services NTRPROF PHONE/NTRNET/EHR ASSMT&MGMT 21-30 MIN
99449 Non-Face-to-Face Physician Services NTRPROF PHONE/NTRNET/EHR ASSMT&MGMT 31/> MIN
99451 Non-Face-to-Face Physician Services NTRPROF PHONE/NTRNET/EHR ASSMT&MGMT 5/> MIN
99452
Non-Face-to-Face Physician Services
NTRPROF PHONE/NTRNET/EHR REFERRAL SVC 30 MIN
99453
Non-Face-to-Face Physician Services
REM MNTR PHYSIOL PARAM 1ST SET UP PT EDUCAJ EQP
99454
Non-Face-to-Face Physician Services
REM MNTR PHYSIOL PARAM 1ST DEV SUPPLY EA 30 D
99457
Non-Face-to-Face Physician Services
REMOTE PHYSIOLOGIC MONITORING 20 MIN+ PER MONTH
98966
Non-Physician Telephone Services
NONPHYSICIAN TELEPHONE ASSESSMENT 5-10 MIN
98967
Non-Physician Telephone Services
NONPHYSICIAN TELEPHONE ASSESSMENT 11-20 MIN
98968 Non-Physician Telephone Services NONPHYSICIAN TELEPHONE ASSESSMENT 21-30 MIN
99201 Office/Other Outpatient Services OFFICE OUTPATIENT NEW 10 MINUTES
99202 Office/Other Outpatient Services OFFICE OUTPATIENT NEW 20 MINUTES
99203 Office/Other Outpatient Services OFFICE OUTPATIENT NEW 30 MINUTES
99204
Office/Other Outpatient Services
OFFICE OUTPATIENT NEW 45 MINUTES
99205
Office/Other Outpatient Services
OFFICE OUTPATIENT NEW 60 MINUTES
99211
Office/Other Outpatient Services
OFFICE OUTPATIENT VISIT 5 MINUTES
99212
Office/Other Outpatient Services
OFFICE OUTPATIENT VISIT 10 MINUTES
99213
Office/Other Outpatient Services
OFFICE OUTPATIENT VISIT 15 MINUTES
99214
Office/Other Outpatient Services
OFFICE OUTPATIENT VISIT 25 MINUTES
99215 Office/Other Outpatient Services OFFICE OUTPATIENT VISIT 40 MINUTES

Primary Care Expenditures Report 34
Narrow definition of procedures
HCPCs or
CPT codes
Procedure Category Procedure Long Description
98925
Osteopathic Manipulation
OSTEOPATHIC MANIPULATIVE TX 1-2 BODY REGIONS
98926
Osteopathic Manipulation
OSTEOPATHIC MANIPULATIVE TX 3-4 BODY REGIONS
98927
Osteopathic Manipulation
OSTEOPATHIC MANIPULATIVE TX 5-6 BODY REGIONS
98928
Osteopathic Manipulation
OSTEOPATHIC MANIPULATIVE TX 7-8 BODY REGIONS
98929 Osteopathic Manipulation OSTEOPATHIC MANIPULATIVE TX 9-10 BODY REGIONS
11981 Preventive Medicine Services INSJ NON-BIODEGRADABLE DRUG DELIVERY IMPLANT
11982 Preventive Medicine Services REMOVAL NON-BIODEGRADABLE DRUG DELIVERY IMPLANT
11983 Preventive Medicine Services RMVL W/RINSJ NON-BIODEGRADABLE DRUG DLVR IMPLT
58300 Preventive Medicine Services INSERTION INTRAUTERINE DEVICE IUD
83655
Preventive Medicine Services
ASSAY OF LEAD
99173
Preventive Medicine Services
SCREENING TEST VISUAL ACUITY QUANTITATIVE BILAT
99381
Preventive Medicine Services
INITIAL PREVENTIVE MEDICINE NEW PATIENT <1YEAR
99382
Preventive Medicine Services
INITIAL PREVENTIVE MEDICINE NEW PT AGE 1-4 YRS
99383
Preventive Medicine Services
INITIAL PREVENTIVE MEDICINE NEW PT AGE 5-11 YRS
99384
Preventive Medicine Services
INITIAL PREVENTIVE MEDICINE NEW PT AGE 12-17 YR
99385 Preventive Medicine Services INITIAL PREVENTIVE MEDICINE NEW PT AGE 18-39YRS
99386 Preventive Medicine Services INITIAL PREVENTIVE MEDICINE NEW PATIENT 40-64YRS
99387 Preventive Medicine Services INITIAL PREVENTIVE MEDICINE NEW PATIENT 65YRS&>
99391 Preventive Medicine Services PERIODIC PREVENTIVE MED ESTABLISHED PATIENT <1Y
99392
Preventive Medicine Services
PERIODIC PREVENTIVE MED EST PATIENT 1-4YRS
99393
Preventive Medicine Services
PERIODIC PREVENTIVE MED EST PATIENT 5-11YRS
99394
Preventive Medicine Services
PERIODIC PREVENTIVE MED EST PATIENT 12-17YRS
99395
Preventive Medicine Services
PERIODIC PREVENTIVE MED EST PATIENT 18-39 YRS
99396
Preventive Medicine Services
PERIODIC PREVENTIVE MED EST PATIENT 40-64YRS
99397
Preventive Medicine Services
PERIODIC PREVENTIVE MED EST PATIENT 65YRS& OLDER
99401 Preventive Medicine Services PREVENT MED COUNSEL&/RISK FACTOR REDJ SPX 15 MIN

Primary Care Expenditures Report 35
Narrow definition of procedures
HCPCs or
CPT codes
Procedure Category Procedure Long Description
99402
Preventive Medicine Services
PREVENT MED COUNSEL&/RISK FACTOR REDJ SPX 30 MIN
99403
Preventive Medicine Services
PREVENT MED COUNSEL&/RISK FACTOR REDJ SPX 45 MIN
99404
Preventive Medicine Services
PREVENT MED COUNSEL&/RISK FACTOR REDJ SPX 60 MIN
99406
Preventive Medicine Services
TOBACCO USE CESSATION INTERMEDIATE 3-10 MINUTES
99407 Preventive Medicine Services TOBACCO USE CESSATION INTENSIVE >10 MINUTES
99408 Preventive Medicine Services ALCOHOL/SUBSTANCE SCREEN & INTERVEN 15-30 MIN
99409 Preventive Medicine Services ALCOHOL/SUBSTANCE SCREEN & INTERVENTION >30 MIN
99411 Preventive Medicine Services PREV MED COUNSEL & RISK FACTOR REDJ GRP SPX 30 M
99412 Preventive Medicine Services PREV MED COUNSEL & RISK FACTOR REDJ GRP SPX 60 M
99420
Preventive Medicine Services
ADMN & INTERPJ HEALTH RISK ASSESSMENT INSTRUMENT
99429
Preventive Medicine Services
UNLISTED PREVENTIVE MEDICINE SERVICE
G0101
Preventive Medicine Services
CERV/VAGINAL CANCER SCR; PELV&CLIN BREAST EXAM
G0102
Preventive Medicine Services
PROS CANCER SCREENING; DIGTL RECTAL EXAMINATION
G0436
Preventive Medicine Services
SMOKE TOB CESSATION CNSL AS PT; INTRMED 3-10 MIN
G0437
Preventive Medicine Services
SMOKING & TOB CESS CNSL AS PT; INTENSIVE >10 MIN
J1050 Preventive Medicine Services INJECTION MEDROXYPROGESTERONE ACETATE 1 MG
Q0091 Preventive Medicine Services SCREEN PAP SMEAR; OBTAIN PREP &C ONVEY TO LAB
G0513 Prolonged Preventive Services PRLNG PREV SRVC OFC/OTH O/P RQR DIR CTC;1ST 30 M
G0514 Prolonged Preventive Services PRLNG PREV SRVC OFC/OTH O/P DIR CTC;EA ADD 30 M
99354
Prolonged Services
PROLNG E&M/PSYCTX SVC OFFICE O/P DIR CON 1ST HR
99355
Prolonged Services
PROLNG E&M/PSYCTX SVC OFFICE O/P DIR CON ADDL 30
99358
Prolonged Services
PROLNG E/M SVC BEFORE&/AFTER DIR PT CARE 1ST HR
99359
Prolonged Services
PROLNG E/M BEFORE&/AFTER DIR CARE EA 30 MINUTES
99360
Prolonged Services
PHYS STANDBY SVC PROLNG PHYS ATTN EA 30 MINUTES
99495
Transitional Care Management Services
TRANSITIONAL CARE MANAGE SRVC 14 DAY DISCHARGE
99496 Transitional Care Management Services TRANSITIONAL CARE MANAGE SRVC 7 DAY DISCHARGE

Primary Care Expenditures Report 36
Narrow definition of procedures
HCPCs or
CPT codes
Procedure Category Procedure Long Description
G0008
Vaccine Administration
ADMINISTRATION OF INFLUENZA VIRUS VACCINE
G0009
Vaccine Administration
ADMINISTRATION OF PNEUMOCOCCAL VACCINE
G0010
Vaccine Administration
ADMINISTRATION OF HEPATITIS B VACCINE
Broad definition of procedure codes
HCPCs or
CPT codes
Procedure Category Procedure Long Description
59510 Cesarean Delivery Procedures OB ANTEPARTUM CARE CESAREAN DLVR & POSTPARTUM
59515
Cesarean Delivery Procedures
CESAREAN DELIVERY ONLY W/POSTPARTUM CARE
59610
Delivery Procedures After Previous Cesarean Delivery
ROUTINE OB CARE VAG DLVRY & POSTPARTUM CARE VB
59614 Delivery Procedures After Previous Cesarean Delivery VAGINAL DELIVERY & POSTPARTUM CARE VBAC
59618
Delivery Procedures After Previous Cesarean Delivery
ROUTINE OBSTETRICAL CARE ATTEMPTED VBAC
59622 Delivery Procedures After Previous Cesarean Delivery CESAREAN DLVRY & POSTPARTUM CARE ATTEMPTED VBA
99464
Delivery/Birthing Room Attendance & Resuscitation Services
ATTN AT DELIVERY 1ST STABILIZATION OF NEWBORN
99465
Delivery/Birthing Room Attendance & Resuscitation Services
DELIVERY/BIRTHING ROOM RESUSCITATION
99377 Hospice Services SUPERVISION HOSPICE PATIENT/MONTH 15-29 MIN
99378
Hospice Services
SUPERVISION HOSPICE PATIENT/MONTH 30 MINUTES/>
G0182 Hospice Services PHYS SUPV PT UNDER MEDICARE-APPROVED HOSPICE
99304
Nursing Facility Services
INITIAL NURSING FACILITY CARE/DAY 25 MINUTES
99305
Nursing Facility Services
INITIAL NURSING FACILITY CARE/DAY 35 MINUTES
99306 Nursing Facility Services INITIAL NURSING FACILITY CARE/DAY 45 MINUTES
99307
Nursing Facility Services
SBSQ NURSING FACILITY CARE/DAY E/M STABLE 10 MIN
99308 Nursing Facility Services SBSQ NURSING FACIL CARE/DAY MINOR COMPLJ 15 MIN
99309
Nursing Facility Services
SBSQ NURSING FACIL CARE/DAY NEW PROBLEM 25 MIN
99310
Nursing Facility Services
SBSQ NURS FACIL CARE/DAY UNSTABL/NEW PROB 35 MIN

Primary Care Expenditures Report 37
Broad definition of procedure codes
HCPCs or
CPT codes
Procedure Category Procedure Long Description
99315
Nursing Facility Services
NURSING FACILITY DISCHARGE MANAGEMENT 30 MINUTES
99316
Nursing Facility Services
NURSING FACILITY DISCHARGE MANAGEMENT 30 MINUTES
99318 Nursing Facility Services E/M ANNUAL NURSING FACILITY ASSESS STABLE 30 MIN
99379
Nursing Facility Services
SUPERVISION NURS FACILITY PATIENT MO 15-29 MIN
99380 Nursing Facility Services SUPERVISION NURS FACILITY PATIENT MONTH 30 MIN/>
99484
Psychiatric Care Management
CARE MGMT SERVICES BEHAVIORAL HLTH COND 20 MINS
99492
Psychiatric Care Management
1ST PSYCHIATRIC COLLAB CARE MGMT 1ST 70 MINS
99493 Psychiatric Care Management SBSQ PSYCHIATRIC COLLAB CARE MGMT 1ST 60 MINS
99494
Psychiatric Care Management
1ST/SBSQ PSYCH COLLAB CARE MGMT EA ADDL 30 MINS
G0502 Psychiatric Care Management INIT PS CCM 1ST 70 MIN 1ST CAL MO BEH HC MGR AC
G0503
Psychiatric Care Management
SUBSQT PS CCM 1ST 60 MIN SUBSQT MO BEH HC MGR AC
G0504
Psychiatric Care Management
INIT/SUBSQ PS CCM EA ADD 30 MN CAL MO BHC MGR AC
G0507 Psychiatric Care Management CARE MGMT BH COND AL 20 MIN CL STAFF TM P CAL MO
59400
Vaginal Delivery, Antepartum & Postpartum Care Procedures
OB CARE ANTEPARTUM VAG DLVR & POSTPARTUM
59410 Vaginal Delivery, Antepartum & Postpartum Care Procedures VAGINAL DELIVERY ONLY W/POSTPARTUM CARE
59425
Vaginal Delivery, Antepartum & Postpartum Care Procedures
ANTEPARTUM CARE ONLY 4-6 VISITS
59426
Vaginal Delivery, Antepartum & Postpartum Care Procedures
ANTEPARTUM CARE ONLY 7/> VISITS
59430 Vaginal Delivery, Antepartum & Postpartum Care Procedures POSTPARTUM CARE ONLY SEPARATE PROCEDURE

Office of Financial Management
P.O. Box 43113 • Olympia, WA • 98504-3113
Phone: 360-902-0555
